

Marisa Novaes de Figueiredo1; Jeremiah Tao2; Patricia Akaishi3; Roberto Murillo Limongi1
DOI: 10.5935/0004-2749.20170085
ABSTRACT
Purpose: Increased tarsal platform show (TPS) and decreased brow fat span (BFS) are associated with favorable results in women undergoing cosmetic blepharoplasty. We conducted a study to evaluate the efficacy of upper blepharoplasty with or without a technique (brassiere sutures) to increase TPS and decrease BFS.
Methods: This is a prospective, randomized, comparative, case series study of 100 eyelids (50 consecutive women patients) treated with cosmetic upper blepharoplasty performed by a single surgeon. Patients were randomized to receive traditional upper blepharoplasty with a single running suture skin closure versus orbicularis oculi muscle fixation to the periosteum (brassiere sutures) prior to skin closure. Data on patient age, duration of follow-up, complications, and treatment were analyzed. The mean TPS, mean BFS, and mean TPS/BFS ratio were measured at three anatomic landmarks before and after surgery.
Results: Fifty-six eyelids (28 patients) were treated with traditional single suture blepharoplasty, and 44 eyelids (22 patients) had brassiere sutures. In both groups, paired t-tests indicate significant differences between preoperative and postoperative evaluations (p<0.05) for eyelid parameters in each location. However, when TPS, BFS, and TPS/BFS ratio were compared between groups with two-way ANOVA, there were no statistically significant differences (p>0.05).
Conclusions: Brassiere sutures during upper blepharoplasty and traditional blepharoplasty were associated with postoperative increase in TPS, decrease in BFS, and increase in TPS/BFS, without statistically significant differences between these surgeries.
Keywords: Blepharoplasty/surgery; Blepharoplasty/methods; Eyelids/surgery; Suture techniques
RESUMO
Objetivo: O aumento do TPS (porção pretarsal visível) e a diminuição do BFS (porção preseptal visível) estão associados com resultados favoráveis em mulheres submetidas a blefaroplastia estética. Os autores avaliaram a eficácia da cirurgia de blefaroplastia superior associada ou não à técnica (sutura de brassiere) em aumentar o TPS e diminuir o BFS.
Métodos: Estudo prospectivo, comparativo, randomizado de uma série de casos de 100 pálpebras (50 pacientes mulheres) tratados com blefaroplastia superior por um único cirurgião. Os pacientes foram randomizados para ser submetidos a tradicional blefaroplastia superior (com sutura única da pele) ou para realizarem sutura de fixação do músculo orbicular no periósteo (sutura de brassiere) antes da sutura de pele. Foi analisado idade do paciente, tempo de acompanhamento, complicações e tratamento. A média do TPS, BFS e relação TPS/BFS foram medidas antes e depois da cirurgia em três pontos anatômicos.
Resultados: Cinquenta e seis pálpebras (28 pacientes) foram submetidas à tradicional blefaroplastia e 44 pálpebras (22 pacientes) fizeram a blefaroplastia superior associado com sutura de brassiere. Em ambos os grupos, os testes t pareados indicam diferenças significativas entre as avaliações pré-operatórias e pós-operatórias (p<0,05) para os parâmetros da pálpebra nos três pontos anatômicos estudados. Contudo, ao comparar os resultados da relação TPS, BFS e TPS/BFS entre os grupos (usando ANOVA bidirecional), não há diferença estatisticamente significante (p>0,05).
Conclusão: Suturas de brassiere com blefaroplastia superior e blefaroplastia tradicional foram associadas com um aumento no pós-operatório do TPS, diminuição do BFS, e aumento da relação TPS/BFS, contudo sem diferença estatisticamente significativa entre essas cirurgias.
Descritores: Blefaroplastia/cirurgia; Blefaroplastia/métodos; Pálpebras/cirurgia; Técnicas de sutura
INTRODUCTION
Dermatochalasis is a common condition, usually associated with aging, in which redundant skin of the upper eyelids hangs on to or even below the eyelashes. The increase in the weight of the upper eyelids sometimes interferes with vision, and the excess hooded skin is also often undesirable because it causes a tired or aged appearance or both(1,2).
Upper blepharoplasty, one of the most commonly performed plastic surgical procedures, treats dermatochalasis. Modifications of upper eyelid blepharoplasty address the brow and include both browpexy and retro-orbicularis oculi fat (ROOF) pad suspension. Goldberg described a "brassiere suture" technique in which the orbicularis oculi is sutured to the superior lateral orbital rim periosteum(3). These adjuncts may enhance the contour, projection, and fullness of the eyebrow. Supporting the brow fat pad during blepharoplasty has been shown to increase eyebrow fullness and improve the eyebrow-eyelid transition and contour to help achieve a more youthful and feminizing appearance(4-8).
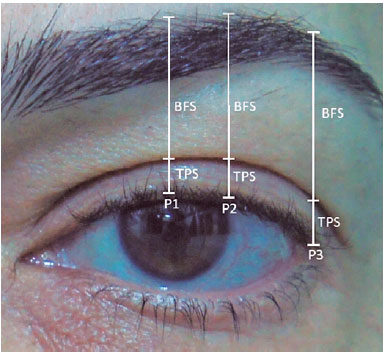
The tarsal platform show (TPS) and brow fat span (BFS) are key measurements for aesthetically quantifying the findings of the upper face. TPS is the distance between the upper eyelid margin and the crease, and BFS is the distance from the superior brow hairs to the crease in primary gaze. Especially in the Western eyelid, obliteration of the tarsal platform, or "eyeshadow space," may be an undesirable trait. Conversely, an unnaturally elongated TPS may be undesirable. Morley et al. demonstrated that in addition to TPS size, symmetry is a major input in upper eyelid aesthetics(9). This study compares the results of upper blepharoplasty with or without brassiere suture with the use of objective TPS and BFS measurements from a digital image system.
METHODS
The CBCO (Eye Surgery Brazilian Center) institutional review board approved the study. All patients provided written informed consent in accordance with the Declaration of Helsinki after receiving a detailed description of the nature and risks of the procedures.
This prospective, randomized, observational case series study included 100 eyelids (50 patients) that underwent cosmetic upper blepharoplasty. Patients with an odd total number of letters in their first name received traditional upper blepharoplasty with a single running suture skin closure (group A). The rest of the patients received orbicularis oculi muscle fixation to the periosteum (brassiere sutures) in conjunction with a single running suture skin closure (group B).
Data on patient age, duration of follow-up, type of surgery, visual acuity, complications, and treatment were analyzed. The exclusion criteria were a history of thyroid eye disease, levator dehiscence ptosis, blepharospasm, facial nerve paresis, a history of previous upper facial surgery or trauma, and postoperative follow-up for less than 6 months.
Using standardized photographs with the patient upright, the head and face in neutral position, and the patient in primary gaze, two measurements were obtained preoperatively and >6 months postoperatively. TPS was calculated between the upper eyelid margin and the crease. BFS was measured as the distance from the superior brow hairs to the crease. The mean TPS/BFS ratio was obtained by the equation: tarsal platform show/brow fat span (TPS/BFS). These were measured at three anatomic locations: the center of the pupil, the lateral corneal limbus, and the eyelid lateral canthus along the vertical meridian (Figure 1).
Pre- and postoperative images were analyzed with ImageJ 1.58 software (National Institutes of Health, rsbweb.nih.gov/ij/download). The software was calibrated using a corneal diameter of 11.5 mm in order to convert pixel measurements to millimeters. Comparisons were performed according to the type of surgery, and the data were submitted to preoperative and postoperative statistical analysis.
Surgical procedure
All surgeries were performed by a single surgeon (RML) between May 2014 and November 2015. The skin incisions were marked with a skin marking pen. On each side, 3 to 4 cc of 2% lidocaine with 1:100,000 epinephrine was infiltrated into the eyelids. The preseptal orbicularis skin and muscle were removed with a size 15 scalpel blade and scissors. Hemostasis was achieved with conservative electrocautery. For traditional blepharoplasty (group A), the skin was closed with a running 6-0 nylon suture.
The brassiere suture technique (group B) was performed as follows. Prior to skin closure as above, three 6-0 polyglactin sutures were passed along the lateral fourth of the orbital rim, from the orbicularis oculi muscle adjacent to the inferior skin edge to the periosteum at the arcus marginalis and back to the orbicularis (Figure 2). The sutures attached the inferior orbicularis oculi muscle edge to the arcus marginalis of the lateral ROOF. Sutures were placed until there was a visible "plumping" of the sub-brow tissues (Figure 2).

Postoperatively, the wounds were dressed with combined antibiotic/corticosteroid ointment four times per day for 1 week. Cold pads were applied off and on for 48 hours. The skin was cleansed with water and a neutral soap. The skin sutures were removed after 1 week.
Statistical analysis
The paired t-test was used to test the significance of the differences between the two groups for each continuous variable. Statistical analysis was performed with the SPSS version 18.0 software package. A p value <0.05 was considered to indicate statistical significance. Two-way analysis of variance (ANOVA) was performed to examine the influence of location and group on the absolute changes from baseline in eyelid parameters (TPS, BPS, and TPS/BPS ratio). Post hoc Tukey multiple comparison tests were performed when appropriate. All statistical analyses were performed with R software (R Foundation for Statistical Computing, Vienna, Austria). A p value <0.05 was considered to indicate statistical significance, and all reported p values are two-sided.
RESULTS
The mean age was 60.7 ± 10.71 years in group A (range, 44-81 years) and 55.0 ± 9.13 years in group B (range, 35-75 years). Fifty-six eyelids (28 patients) received blepharoplasty alone, and 44 eyelids (22 patients) had blepharoplasty with brassiere sutures. The mean follow-up time was 8.9 months (range, 6-12 months). No significant complications were noted, and there was no lagophthalmos.
The preoperative TPS was shorter in both groups separately and the blepharoplasty was successful in increasing the TPS in postoperative period, which means blepharoplasty alone and concurrent brassiere sutures caused the lengthening of TPS (Table 1). Preoperative BFS was similar in both groups, and postoperative BFS decreased in both groups (Table 1).
There was no evidence of a significant interaction (group versus location) on the changes in TPS and BFS. Thus, the group effect did not depend on the location, and the effect of location did not depend on the group (Table 2). In addition, there was no evidence of a significant group effect (p>0.05), which indicates that the mean changes in TPS and BFS did not differ between group A and group B. Furthermore, there was no evidence of significant location effects (p>0.05), which indicates that the mean changes in TPS and BFS did not differ significantly among the three anatomic locations (Table 2).
The preoperative to postoperative changes in the mean TPS/BFS ratio at all three anatomic locations were statistically significant in both groups (Table 1), but when the changes were compared between groups, there was no evidence of a significant group effect (p>0.05). This indicates that the mean changes in the TPS/BPS ratio did not differ between group A and group B (Table 2).
However, the change in the mean TPS/BFS ratio differed significantly among the three locations (p<0.05). Since there was no statistically significant interaction among the three locations, we can interpret the results for the different locations, which can be found in the multiple comparisons table (Table 3). The contrast between P3 (eyelid lateral canthus) and P1 (center of the pupil) has a higher mean change. P2 (lateral corneal limbus) has a higher mean change than P3 (eyelid lateral canthus). P1 (center of the pupil) and P2 (lateral corneal limbus) are not significantly different.
To evaluate preoperative and postoperative symmetry, we calculated TPS and BFS symmetry as the delta, or the smaller subtracted from the larger value of TPS or BFS (Table 4). The studied groups showed minimal asymmetry of TPS and BFS after surgery at all three anatomic landmarks, without a significant difference in measurements (p>0.05). No significant correlations were noted between the right and left upper eyelids.
DISCUSSION
Dermatochalasis is a common condition of the upper eyelids. The characteristic excess fold of skin obscures the normal upper eyelid crease, contributing to a tired or aged appearance(1,2). Upper blepharoplasty is one of the most frequently performed aesthetic surgeries of the periocular area(2,7). The removal of eyelid skin, however, may contribute to brow descent(4,10-12). Deflation and descent of the lateral eyebrow fat pad are other important contributors to the appearance of periorbital aging. In addition, a low, flat brow is associated with masculinity, while an arched or laterally peaked brow is associated with femininity(13-17). Brow ptosis and dermatochalasis obliterate the tarsal platform, also known as the "eyeshadow space."
Although some patients require a brow lift to adequately treat the brow, milder cases may benefit from browpexy(12). Goldberg first described the brassiere suture approach to restore the volume of the lateral eyebrow fat pad that may have some browpexy effects(3). Importantly, suture fixations of brow tissues provide some support but do not reliably the brow. Nevertheless, from an aesthetic standpoint, the suture may have a barrier effect on brow fat descent and bunches the brow fat, potentially enhancing volume and contributing to a more youthful appearance(3).
Brow findings should be incorporated in the preoperative upper eyelid aesthetic evaluation. Asymmetry anywhere along the upper eyelid and brow continuum should be factored into surgical planning(6,7). The authors, like others, have found that two parameters, tarsal platform show (TPS) and brow fat span (BFS), are useful for aesthetically quantifying the upper face(7,8). Small differences in TPS may be more noticeable than small amounts of asymmetry in BFS(8). In addition, a long TPS can create the impression of a ptotic eyelid. The TPS/BFS ratio may also be useful. Morley et al. describe a TPF/BFS of 1:1.5 medially and 1:3 laterally to be desirable(9).
The present study demonstrated an increase in TPS following blepharoplasty in both groups, without a significant difference in measures between the groups. The amount of BFS decreased in both groups, also without a significant difference between the groups.
Measuring the TPS/BFS ratio after surgery, we found that brassiere sutures provide the same desirable ratio at the lateral aspect of the superior eyelid/eyebrow previously reported by other studies(9).
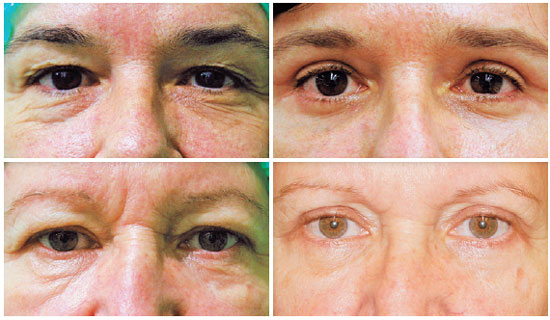
This study demonstrates, using a prospective, randomized methodology with objective measures, that adjunctive brassiere sutures improve the mean change in TPS and BFS, as does traditional blepharoplasty. These data demonstrate, in a prospective, randomized methodology with objective measures, that adjunctive brassiere sutures improve the mean change in TPS and BFS, like traditional blepharoplasty (Figure 3). These results do not suggest that brassiere sutures are more effective than traditional blepharoplasty for stabilizing the lateral brow.
CONCLUSION
Brassiere sutures and traditional blepharoplasty increase TPS and TPS/BFS ratio and decrease BFS in upper blepharoplasty, with no statistically significant differences between these surgeries. Both techniques may be useful to provide a more youthful and feminizing appearance in female patients undergoing upper blepharoplasty.
REFERENCES
1. DeAngelis DD, Carter SR, Seiff SR. Dermatochalasis. Int Ophthalmol Clin. 2002;42(2):89-101. Review.
2. Fagien S. Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita. Plast Reconstr Surg. 2002;110(1):278-91; discussion 292.
3. Varshney N, Lin JL, Kohn JC, Isaacs DK, Hoenig JA, Goldberg RA. Using a brassiere suture technique to de ne lateral tarsal platform and eyebrow fat contours. 43 rd. Annual Meeting of the American Society of Ophthalmic Plastic and Reconstructive Surgery. Chicago, IL; 2012.
4. Zarem HA, Resnick JI, Carr RM, Wootton DG. Browpexy: lateral orbicularis muscle fixation as an adjunct to upper blepharoplasty. Plast Reconstr Surg. 1997;100(5):1258-61.
5. Briceno CA, Zhang-Nunes SX, Massry GG. Minimally invasive surgical adjuncts to upper blepharoplasty. Facial Plast Surg Clin N Am. 2015;23(3):137-51.
6. Pool SM, van der Lei B. Asymmetry in upper blepharoplasty: A retrospective evaluation study of 365 bilateral upper blepharoplasties conducted between January 2004 and December 2013. J Plast Reconstr Aesthet Surg. 2015;68(4):464-8.
7. Goldberg RA, Lew H. Cosmetic outcome of posterior approach ptosis surgery (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2011;109: 157-67.
8. Papageorgiou KI, Ang M, Chang SH, Kohn J, Martinez S, Goldberg RA. Aesthetic considerations in upper eyelid retraction surgery, Ophthal Plast Reconstr Surg. 2012; 28(6):419-23.
9. Morley AM, Taban M, Malhotra R, Goldberg RA. Use of hyaluronic Acid gel for upper eyelid filling and contouring. Ophthal Plast Reconstr Surg. 2009;25(6):440-4.
10. Faigen S. Eyebrow analysis after blepharoplasty in patients with brow ptosis. Ophthal Plast Reconstr Surg. 1992;8(3):210-4.
11. Georgescu D, Anderson RL, McCann JD. Brow ptosis correction: a comparison of five techniques. Facial Plast Surg. 2010;26:186-92.
12. Baker MS, Shams PN, Allen RC. The quantitated internal suture browpexy: comparison of two brow-lifting techniques in patients undergoing upper blepharoplasty. Ophthal Plast Reconstr Surg. 2016;32(3):204-6.
13. Packiriswamy V, Kumar P, Bashour M. Photogrammetric analysis of eyebrow and upper eyelid dimensions in South Indians and Malaysian South Indians. Aesthet Surg J. doi: 10.1177/1090820X13503472. Epub 2013 Sep 9.
14. Price KM, Gupta PK, Woodward JA, Stinnett SS, Murchison AP. Eyebrow and eyelid dimensions: an anthropometric analysis of African Americans and Caucasians. Plast Reconstr Surg. 2009;124(2):615-23.
15. Dharap AS, Reddy SC. Upper eyelid and eyebrow dimensions in Malays. Med J Malaysia. 1995;50(4):377-81.
16. Cartwright MJ, Kurumety UR, Nelson CC, Frueh BR, Musch DC. Measurements of upper eyelid and eyebrow dimensions in healthy white individuals. Am J Ophthalmol. 1994;117(2):231-4.
17. Knoll BI, Attkiss KJ, Persing JA. The influence of forehead, brow, and periorbital aesthetics on perceived expression in the youthful face. Plast Reconstr Surg. 2008;121(5): 1793-802.
Submitted for publication:
September 15, 2016.
Accepted for publication:
May 18, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Approved by the following research ethics committee: Centro Brasileiro de Cirurgia de Olhos (#CBCO61).
Clinical trials: NCT02879552