

Manuela Bezerril Cipião Fernandes1; Rodrigo Vicentini Fernandes de Souza1; Gregório Carolino Vasconcelos2; Kérsia Gomes Ribeiro2; Bruno Bezerril Andrade3; Cláudia Regina Fernandes1
DOI: 10.1590/S0004-27492013000600005
ABSTRACT
PURPOSE: Ocular akinesia, the use of anticoagulants, and patient collaboration are some of the factors that must be taken into consideration when choosing the appropriate anesthesia for phacoemulsification cataract surgery. The satisfaction of patients with the use of topical anesthesia and conscious sedation for this procedure has not been enough described in Brazil. Conscious sedation allows patient walk and answer a voice command. To assess the satisfaction, pain, and perioperative hemodynamic alterations of patients subjected to phacoemulsification under conscious sedation and topical anesthesia supplemented with intracameral lidocaine. METHODS: Prospective cohort non-controlled study that included patients treated by the same surgical team over a 70-day period. Sedation was performed with midazolam at a total dose of 3 mg and topical anesthesia with 0.5% proxymetacaine chlorhydrate and 2% lidocaine gel combined with 2% lidocaine by intracameral route. The intraoperative vital parameters, scores based on the Iowa Satisfaction with Anesthesia Scale (ISAS), and the pain visual analog scale (VAS) were recorded at several time points after surgery. RESULTS: A total of 106 patients were enroled in study (73.6% female), the mean age was 65.9 years. The surgical procedures lasted 11.2 minutes on average. The hemodynamic parameters did not exhibit significant changes at any of the investigated time points. The average ISAS score was 2.67 immediately after surgery and 2.99 eight hours after the surgery; this increase was statistically significant (p<0.0001). More than two-thirds (68.9%) of the participants (73 patients) did not report any pain in the transoperative period, and 98.1% of patients denied the occurrence of pain after surgery. CONCLUSIONS: Patients that received topical anesthesia supplemented by intracameral lidocaine combined with sedation for phacoemulsification cataract surgery reported adequate level of satisfaction with the anesthetic choice. Furthermore, the patients exhibited hemodynamic parameter stability and pain control.
Keywords: Anesthesia; Lidocaine; Administration, topical; Ophthalmologic surgical procedures; Phacoemulsification; Cataract extraction; Patient satisfaction; Pain measurement; Conscious sedation
RESUMO
OBJETIVO: Acinesia ocular, uso de anticoagulantes e cooperação do paciente são fatores envolvidos na escolha da anestesia para cirurgia de catarata por facoemulsificação. A satisfação com anestesia tópica associada à sedação consciente neste procedimento foi pouco descrita no Brasil. Sedação consciente permite que o paciente sedado mantenha a capacidade de deambular e de responder ao chamado de voz. Avaliar a satisfação, dor e alterações hemodinâmicas perioperatórias de pacientes submetidos à facoemulsificação sob sedação consciente por anestesia tópica com injeção de lidocaína na câmara anterior. MÉTODOS: Estudo de coorte prospectivo, não controlado de pacientes operados pela mesma equipe em um período de 70 dias. Realizada sedação com 3 mg de midazolam, anestesia tópica com cloridrato de proximetacaína 0,5% e lidocaína gel 2%, associada à injeção de lidocaína 2% na câmara anterior. Registrados parâmetros vitais intraoperatórios, escala de satisfação com a anestesia de Iowa (ISAS) e a Escala Analógica Visual da Dor (EVA) em diferentes períodos do pós-operatório. RESULTADOS: Foram avaliados 106 pacientes (73,6% do sexo feminino), com idade média de 65,9 anos. O tempo cirúrgico médio foi de 11,2 minutos. Não houve diferença estatisticamente significante entre as variáveis hemodinâmicas nos momentos estudados. Ao final da operação, a média de escores na escala ISAS foi de 2,67 e 8 horas após foi de 2,99, apresentando aumento significativo (p<0,0001). Não houve relato de qualquer dor transoperatória em 68,9% dos casos, e 98,10% dos pacientes negaram dor pós-operatória. CONCLUSÕES: Em cirurgia de facectomia por facoemulsificação realizada sob sedação consciente associada à anestesia tópica com injeção de lidocaína 2% na câmara anterior, obtêm-se níveis adequados de satisfação com a anestesia, estabilidade de variáveis hemodinâmicas durante o procedimento e adequado controle da dor.
Descritores: Anestesia; Lidocaína; Administração tópica; Procedimentos cirúrgicos oftalmológicos; Facoemulsificação; Extração de catarata; Satisfação do paciente; Medição da dor; Sedação consciente
ORIGINAL ARTICLE
Assessing patient satisfaction with cataract surgery under topical anesthesia supplemented by intracameral lidocaine combined with sedation
Avaliação da satisfação dos pacientes submetidos à facectomia por facoemulsificação realizada com anestesia tópica associada à lidocaína na câmara anterior combinada com sedação
Manuela Bezerril Cipião FernandesI; Rodrigo Vicentini Fernandes de SouzaI; Gregório Carolino VasconcelosII; Kérsia Gomes RibeiroII; Bruno Bezerril AndradeIII; Cláudia Regina FernandesI
IPhysician, Center of Ophthalmology of Ceará - Fortaleza (CE), Brasil
IIPhysician, General Hospital of Fortaleza - Fortaleza (CE), Brasil
IIIPhysician, National Institutes of Health, Bethesda, Maryland, USA
ABSTRACT
PURPOSE: Ocular akinesia, the use of anticoagulants, and patient collaboration are some of the factors that must be taken into consideration when choosing the appropriate anesthesia for phacoemulsification cataract surgery. The satisfaction of patients with the use of topical anesthesia and conscious sedation for this procedure has not been enough described in Brazil. Conscious sedation allows patient walk and answer a voice command. To assess the satisfaction, pain, and perioperative hemodynamic alterations of patients subjected to phacoemulsification under conscious sedation and topical anesthesia supplemented with intracameral lidocaine.
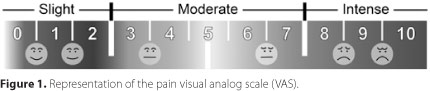
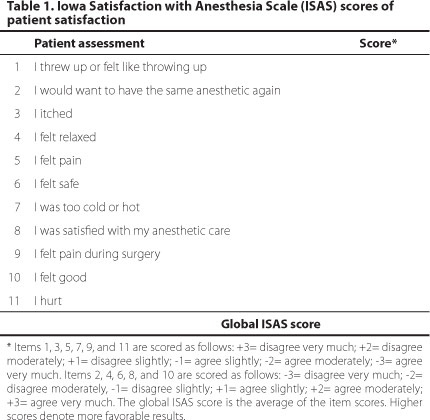
METHODS: Prospective cohort non-controlled study that included patients treated by the same surgical team over a 70-day period. Sedation was performed with midazolam at a total dose of 3 mg and topical anesthesia with 0.5% proxymetacaine chlorhydrate and 2% lidocaine gel combined with 2% lidocaine by intracameral route. The intraoperative vital parameters, scores based on the Iowa Satisfaction with Anesthesia Scale (ISAS), and the pain visual analog scale (VAS) were recorded at several time points after surgery.
RESULTS: A total of 106 patients were enroled in study (73.6% female), the mean age was 65.9 years. The surgical procedures lasted 11.2 minutes on average. The hemodynamic parameters did not exhibit significant changes at any of the investigated time points. The average ISAS score was 2.67 immediately after surgery and 2.99 eight hours after the surgery; this increase was statistically significant (p<0.0001). More than two-thirds (68.9%) of the participants (73 patients) did not report any pain in the transoperative period, and 98.1% of patients denied the occurrence of pain after surgery.
CONCLUSIONS: Patients that received topical anesthesia supplemented by intracameral lidocaine combined with sedation for phacoemulsification cataract surgery reported adequate level of satisfaction with the anesthetic choice. Furthermore, the patients exhibited hemodynamic parameter stability and pain control.
Keywords: Anesthesia; Lidocaine; Administration, topical; Ophthalmologic surgical procedures; Phacoemulsification; Cataract extraction; Patient satisfaction; Pain measurement; Conscious sedation
RESUMO
OBJETIVO: Acinesia ocular, uso de anticoagulantes e cooperação do paciente são fatores envolvidos na escolha da anestesia para cirurgia de catarata por facoemulsificação. A satisfação com anestesia tópica associada à sedação consciente neste procedimento foi pouco descrita no Brasil. Sedação consciente permite que o paciente sedado mantenha a capacidade de deambular e de responder ao chamado de voz. Avaliar a satisfação, dor e alterações hemodinâmicas perioperatórias de pacientes submetidos à facoemulsificação sob sedação consciente por anestesia tópica com injeção de lidocaína na câmara anterior.
MÉTODOS: Estudo de coorte prospectivo, não controlado de pacientes operados pela mesma equipe em um período de 70 dias. Realizada sedação com 3 mg de midazolam, anestesia tópica com cloridrato de proximetacaína 0,5% e lidocaína gel 2%, associada à injeção de lidocaína 2% na câmara anterior. Registrados parâmetros vitais intraoperatórios, escala de satisfação com a anestesia de Iowa (ISAS) e a Escala Analógica Visual da Dor (EVA) em diferentes períodos do pós-operatório.
RESULTADOS: Foram avaliados 106 pacientes (73,6% do sexo feminino), com idade média de 65,9 anos. O tempo cirúrgico médio foi de 11,2 minutos. Não houve diferença estatisticamente significante entre as variáveis hemodinâmicas nos momentos estudados. Ao final da operação, a média de escores na escala ISAS foi de 2,67 e 8 horas após foi de 2,99, apresentando aumento significativo (p<0,0001). Não houve relato de qualquer dor transoperatória em 68,9% dos casos, e 98,10% dos pacientes negaram dor pós-operatória.
CONCLUSÕES: Em cirurgia de facectomia por facoemulsificação realizada sob sedação consciente associada à anestesia tópica com injeção de lidocaína 2% na câmara anterior, obtêm-se níveis adequados de satisfação com a anestesia, estabilidade de variáveis hemodinâmicas durante o procedimento e adequado controle da dor.
Descritores: Anestesia; Lidocaína; Administração tópica; Procedimentos cirúrgicos oftalmológicos; Facoemulsificação; Extração de catarata; Satisfação do paciente; Medição da dor; Sedação consciente
INTRODUCTION
Significant changes have been introduced to the techniques and instruments used for cataract surgery over the past 20 years. Such changes include phacoemulsification without corneal suture and the development of foldable intraocular lenses, which allow smaller and self-sealing incisions(1). Additionally, a wide range of anesthetic techniques has been developed for cataract surgery during that period, including general, ophthalmic regional, and topical anesthesia(2).
In the United States, more than 60% of ophthalmologic surgeons prefer topical anesthesia(2). However, in addition to the preferences of the surgeon, patient satisfaction must be taken into consideration. Some of the main patient satisfaction criteria include preoperative anxiety and postoperative pain(3).
The assessment of patient satisfaction with anesthesia is a useful approach for monitoring and improving the quality of preoperative care(4), especially in procedures associated with a low incidence of adverse effects such as phacoemulsification cataract surgery(5).
The main aim of the present study is to assess patient satisfaction after phacoemulsification cataract surgery with intraocular lens implantation with topical anesthesia and intracameral lidocaine combined with conscious sedation. The secondary aims included assessment of the intraoperative hemodynamic parameters and postoperative pain.
METHODS
ETHICAL FEATURES AND INCLUSION CRITERIA
All patients signed an informed consent form before inclusion in the study. The Research Ethics Committee of Assis Chateaubriand Teaching Maternity School Hospital (protocol 80/11), associated with the National Health Council, approved the study. The present analysis was a cohort study conducted with patients subjected to a surgical intervention involving anesthetic and surgical outpatient procedures from September 2011 to November 2011. All procedures were performed by the same anesthesia and surgical teams.
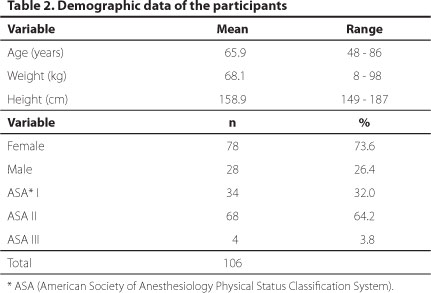
The inclusion criteria were diagnosed cataract and classification as American Society of Anesthesiology Physical Status Classification System (ASA) I to III. The exclusion criteria were as follow: patients with Parkinson's disease, bifascicular block, poor cognitive ability, coronary artery disease, severe lung disease, and heart failure. A total of 106 patients were considered during the recruitment period.
PREOPERATIVE PROTOCOL
Preanesthetic assessment was performed before the surgical procedure, and a questionnaire was completed to provide data regarding the state of the patient organs and systems. The medications used by the patients were recorded as well as the preoperative patient exams. The anesthetic technique was explained to the participants prior to surgery and their vital signs were assessed including: systolic (SAP) and diastolic (DAP) arterial pressure and heart rate (time point 1).
INTRAOPERATIVE PROTOCOL
Peripheral vein access was achieved using a 24-G catheter, after that normal saline solution was infused. Intraoperative monitoring included the following: cardioscope on D2 and V5 leads, pulse oximetry, and non-invasive blood pressure (BP). Midazolam (2 mg) was administered intravenously (IV). The following collyria were instilled in the eye to be operated: one drop of 0.5% proxymetacaine chlorhydrate (anesthetic eyedrops) followed by one drop of 5% povidone-iodine (antiseptic agent). One minute later, one drop of gatifloxacin eyedrops (antibiotic) was applied to the eye. The following sequence was started one minute after gatifloxacin administration: one drop of 0.5% proxymetacaine chlorhydrate every five minutes for 20 minutes (total of four drops) followed by 2% lidocaine gel on the cornea, which was left in place for five minutes. The patient was placed on the surgical table, and 1 mg of intravenous additional midazolam was applied. The hemodynamic parameters (non-invasive blood pressure and heart rate) and peripheral oxygen saturation were recorded before incision (time point 2).
At the beginning of the procedure, the surgeon injected 0.2 ml of 2% unpreserved lidocaine without vasoconstrictor into the intracameral area. The hemodynamic parameters were recorded following lidocaine injection (time point 3) and upon completion of the surgery following the intraocular lens apposition (time point 4). Participant pain complaints during surgery were recorded. When the patient reported pain, intracameral lidocaine was repeated. Upon exiting the operation room, a pain visual analog scale (VAS) was assessed(6,7) (Figure 1). Before discharge from the day-hospital (time point 5), the participants completed a questionnaire designed according to the Iowa Satisfaction with Anesthesia Scale (ISAS)(8-10) (Table 1). VAS and ISAS were also assessed eight hours after the procedure (time point 6). Dipyrone (1 g) was prescribed orally as postoperatively for pain if needed.
DATA ANALYSIS
Descriptive statistical analysis was performed using SPSS software version 19.0. Comparison of the means of the vital parameters was performed by ANOVA followed by the Tukey multiple comparison test.
Comparison of the level of patient satisfaction, as assessed by ISAS, was performed by using the Wilcoxon test for paired samples. Variation of the scores in the pain VAS was assessed by the chi-square test and the Fisher exact test. Statistical analysis was performed using the software Prism Graphpad version 5.0. The significance level was established at 5% (p<0.05).
RESULTS
Patient demographic data are described in table 2. Were included 106 patients with mean age of 65.9 years old (48 to 86 years). The surgical procedure lasted 11.2 minutes on average with a range of 5 to 25 minutes and a standard deviation of 3.34 minutes. The hemodynamic parameters and peripheral hemoglobin saturation are described in Table 3. Based on ANOVA, SAP exhibited a significant difference among the assessed time points (p=0.0458); however, the post-hoc test failed to indicate the specific time points where significant variation occurred (p>0.05 in all pairs assessed with Tukey's post-hoc test). The remainder of the hemodynamic parameters did not show significant variation among the investigated time points.
Regarding patient satisfaction, the lowest ISAS score immediately after surgery was 2.3 and was observed in 1.9% of the patients; the maximum ISAS score (3.0) was found in 53% of the participants. Eight hours after surgery, the lowest ISAS score was 2.63 and was observed in one patient (0.9%), while the maximum ISAS score 3.0 was found in 95.3% of the participants. The increase in the ISAS scores between these two time points was statistically significant (p<0.0001) (Figure 2).
Figure 2 depicts the results of pain assessment at time point 5. Of the 106 individuals analyzed, 68.9% did not report pain at time point 5, 25.4% reported slight pain (VAS 1 to 3), 3.8% reported moderate pain (VAS 4 to 6), and 1.8% reported intense pain (VAS 7 to 8). At time point 6 (eight hours after surgery), 98.1% of the participants reported no pain, and 1.9% reported a VAS=1. Eight patients used dipyrone during the postoperative period. One participant reported nausea at time point 5. At time-point 6 no patients reported nausea or vomiting.
DISCUSSION
The present study assessed patient satisfaction, hemodynamic alterations, and occurrence and intensity of pain following phacoemulsification cataract surgery under sedation and topical anesthesia associated with intracameral lidocaine. These results suggest a high overall level of patient satisfaction, lack of intraoperative hemodynamic alterations, and appropriate pain control.
The topical anesthetic technique used in the present study elicits minimal discomfort when compared with infiltration anesthesia. A study analyzing members of the American Society of Cataract and Refractive Surgery (ASCRS)(11) showed that the choice of topical anesthesia varied as a function of the number of procedures: in 2003, topical anesthesia was used in 38% of the institutions performing 1 to 5 procedures per month, and in 75% of the institutions performing more than 75 procedures per month. The present study was conducted in an institution that performs approximately 400 procedures per month.
An understanding of the factors that reduce patient satisfaction with a given anesthetic technique might contribute to improvement in the standards of quality in patient comfort. Dexter et al.,(8) formulated the ISAS scale (Table 1) to measure patient satisfaction undergoing monitored anesthetic care. This scale generates reliable total scores that are suitable for comparisons between groups of patients or within an individual patient. The usefulness of the ISAS scale for the assessment of satisfaction with anesthesia in cataract surgery has already been established(9). The present study was conducted based on limited subjective data regarding the satisfaction of patients assisted by the same medical team, as no Brazilian data on this topic had been previously reported in the literature.
Regarding patient vital signs, blood pressure (BP), heart rate (HR) and peripheral oxygen saturation did not exhibit significant changes over the anesthetized surgical procedure, which reflects the comfort associated with the investigated technique. These results corroborate findings reported by some authors(12), who assessed the advantages and disadvantages of topical anesthesia with intracameral lidocaine. These authors found that most patients did not exhibit any pain and that the experience was rated positive by the surgeons with respect to patient collaboration, stability of the anterior chamber, level of difficulty in the performance of phacoemulsification, and complications.
The anesthetic technique used in the present study has also been used in other surgical procedures, where it has proven advantages such as safety, efficacy, and preservation of the eye movements. These advantages allow the patient to discard eye dressings at the end of the surgery, increasing patient satisfaction with the procedure(13). Further advantages include no risk of eye perforation in patients with high myopia and no need to interrupt medication in patients with drug-eluting coronary stents using oral anticoagulants(14).
Topical anesthesia does not dismiss the need of an anesthesiologist in the operating room, as he or she is charged with the transoperative monitoring and immediate treatment of pain or other events(15). Conscious sedation is needed to avoid the occurrence of anxiety and for the patient to be able to report on discomfort. Based on that criterion, some authors(16) conducted a study to assess the effect of midazolam on anxiolysis related with topical anesthesia. According to these authors, ideal sedation might allow for patients to relax in the hands of a skillful surgeon and to provide the latter an opportunity to focus exclusively on the procedure. In addition, ideal sedation eliminates the surgical discomfort occasionally elicited by pressure or anxiety.
Two percent lidocaine gel topically applied to the cornea is non toxic to the eye surface(17), while it is efficacious as a topical anesthetic in cataract surgery(18). The use of lidocaine gel as a topical anesthetic in phacoemulsification is thought to hydrate the cornea thus improving visualization by the surgeon during surgery and to reduce the need for the postoperative administration of a balanced salt solution (BSS)(19).
Intracameral addition of lidocaine is performed quite often(20-24); because in topical approaches only the trigeminal nerve ends in the cornea and conjunctiva are anesthetized, whereby complementary anesthesia by means of intracameral unpreserved lidocaine is needed to avoid the irritation of the ciliary nerves due to occasional manipulation of the iris. Current evidence shows that intracameral lidocaine as a supplement in topical anesthesia induces significant reduction in pain perception during surgery when compared with topical anesthesia alone. In addition, intracameral lidocaine keeps the pupil dilated during the surgery(25,26).
Satisfaction cannot be rated as an objective indicator of the quality of anesthetic care; nevertheless, patient-reported satisfaction provides the best access to the outcomes based on patient perspective(10,27-29). The results of the present study indicate a high level of satisfaction with the investigated anesthetic approach at both assessed postoperative time points, and a significantly higher level of satisfaction was observed eight hours after surgery.
The anesthetic procedure employed proved to be effective in the control of pain, as most participants reported no pain in the immediate postoperative period, which is consistent with results from previous studies.
The skills and abilities of surgeons to perform cataract surgery over a short period of time is one of the factors relevant for the feasibility and applicability of the anesthetic procedure employed in the present study(2,19). Indeed, in the present study, the average surgical time was fast (11.2 minutes, standard deviation=3.34 minutes).
CONCLUSION
Patients that received topical anesthesia supplemented by intracameral lidocaine combined with sedation for phacoemulsification cataract surgery reported adequate level of satisfaction with the anesthetic choice. Furthermore, the patients exhibited hemodynamic parameter stability and pain control.
REFERENCES
1. Fichman RA. The clear-corneal incision and astigmatism strategies. In: Fine IH, Fichman RA, Grabow HB, editors. Clear-corneal cataract surgery and topical anesthesia. Thorofare, NJ: Slack; 1993. p.72-6.
2. Malik A, Fletcher EC, Chong V, Dasan J. Local anesthesia for cataract surgery. J Cataract Refract Surg. 2010;36(1):133-52. Comment in: J Cataract Refract Surg. 2010;36(7):1243; author reply 1243-4.
3. Fung D, Cohen MM, Stewart S, Daves A. What determines patient satisfaction with cataract care under topical local anesthesia and monitored sedation in a community hospital setting? Anesth Analg. 2005;100(6):1644-50. Comment in: Anesth Analg. 2006;102(1):327-8.
4. Capuzzo M, Gilli G, Paparella L, Gritti G, Gambi D, Bianconi M, et al. Factors predictive of patient satisfaction with anesthesia. Anesth Analg. 2007;105(2):435-42.
5. Fasolo A, Capuzzo C, Fornea M, Frigo AC, Monterosso C, Zampini A, et al. Health status and patient satisfaction after corneal grafts: results from the corneal transplant epidemiological study. J Ophthalmol. 2012;2012:230641.
6. Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, Loge JH, Fainssinger R, Aass N, Kaasa S; European Palliative Care Research Collaborative (EPCRC). Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073-93.
7. Gaszynski T, Jakubiak J, Wóniak K, Trafidó T, Ratajczyk P, Gaszýski W. . Anestezjol Intens Ter. 2011;43(4):214-9. Polish.
8. Dexter F, Aker J, Wright J. Development of a measure of patient satisfaction with monitored anesthesia care: the Iowa Satisfaction with Anesthesia Scale. Anesthesiology. 1997;87(4):865-73.
9. Fung D, Cohen M, Stewart S, Davies A. Can the Iowa Satisfaction with Anesthesia Scale be used to measure patient satisfaction with cataract care under topical local anesthesia and monitored sedation at a community hospital? Anesth Analg. 2005;100(6):1637-43.
10. Dexter F, Candiotti KA. Multicenter assessment of the Iowa Satisfaction with Anesthesia Scale, an instrument that measures patient satisfaction with monitored anesthesia care. Anesth Analg. 2011;113(2):364-8.
11. Leaming DV. Practice styles and preferences of ASCRS members-2003 survey. J Cataract Refract Surg. 2004;30(4):892-900.
12. Gupta SK, Kumar A, Agarwal S. Cataract surgery under topical anesthesia using 2% lignocaine jelly and intracameral lignocaine: is manual incision cataract surgery comparable to clear corneal phacoemulsification? Indian J Ophthalmol. 2010;58(6): 537-40. Comment in: Indian J Ophthalmol. 2012;60(2):157.
13. Navaleza JS, Pendse SJ, Blecher MH. Choosing anesthesia for cataract surgery. Ophthalmol Clin North Am. 2006;19(2):233-7.
14. Jonas JB, Pakdaman B, Saunder G. Cataract surgery under systemic anticoagulant therapy with coumarin. Eur J Ophthalmol. 2006;16(1):30-2.
15. Gemma M, Gioia L, Dedola E, Basta B, Bianchi I, Fasce F, et al. Anesthesiologist intervention during cataract surgery under topical or peribulbar anesthesia: a propensity model comparison. Eur J Ophthalmol. 2010;20(4):687-93.
16. Habib NE, Mandour NM, Balmer HG. Effect of midazolam on anxiety level and pain perception in cataract surgery with topical anesthesia. J Cataract Refract Surg. 2004; 30(2):437-43.
17. Barequet IS, Soriano ES, Green WR, O'Brien TP. Provision of anesthesia with single application of lidocaine 2% gel. J Cataract Refract Surg. 1999;25(5):626-31.
18. Koch PS. Efficacy of lidocaine 2% jelly as a topical agent in cataract surgery. J Cataract Refract Surg. 1999;25(5):632-4. Comment in: J Cataract Refract Surg. 1999;25(12):1561.
19. Kalyanasundaram TS, Hasan M. Corneal-wetting property of lignocaine 2% jelly. J Cataract Refract Surg. 2002;28(8):1444-5.
20. Gills JP, Cherchio M, Raanan MG. Unpreserved lidocaine to control discomfort during cataract surgery using topical anesthesia. J Cataract Refract Surg, 1997;23(4): 545-50.
21. Crandall AS. Anesthesia modalities for cataract surgery. Curr Opin Ophthalmol. 2001; 12(1):9-11.
22. Cass GD. Choices of local anesthetics for ocular surgery. Ophthalmol Clin North Am. 2006;19(2):203-7.
23. Koch PS. Anterior chamber irrigation with unpreserved lidocaine 1% for anesthesia during cataract surgery. J Cataract Refract Surg. 1997;23(4):551-4. Comment in: J Cataract Refract Surg. 1997;23(10):1434-5.
24. Tan CS, Fam HB, Heng WJ, Lee HM, Saw SM, Au Eong KG. Analgesic effect of supplemental intracameral lidocaine during phacoemulsification under topical anaesthesia: a randomised controlled trial. Br J Ophthalmol. 2011;95(6):837-41.
25. Gutarra Villavicencio RP, Paulin Huerta JM, Chavez Mondragón E, Garzon M, Bustos M, Salas Perez S, et al. Dilatacion pupilar con lidocaina intracameral a 1% en pacientes sometidos a cirugía de catarata. Arch Oftal B Aires . 2011 ;82(1):10-5. Available from: http://www.sao.org.ar/files/archivos-oftalmologia/volumen-82-nro-1/02-dilatacion_pupilar_con_lidocaina_intracameral.pdf
26. Ezra DG, Allan BD. Topical anesthesia alone versus topical anesthesia and intracameral lidocaine in phacoemulsification. Cochrane Database Syst Rev. 2007;(3):CD005276.
27. Capuzzo M, Alvisi R. Is it possible to measure and improve patient satisfaction with anesthesia? Anesthesiol Clin. 2008;26(4):613-26.
28. Bollinger KE, Langston RH. What can patients expect from cataract surgery? Cleve Clin J Med. 2008;75(3):193-200.
29. Benn J, Arnold G, Wei I, Riley C, Aleva F. Using quality indicators in anaesthesia: feeding back data to improve care. Br J Anaesth. 2012;109(1):80-91.
 Correspondence:
Correspondence:
Manuela Bezerril Cipião Fernandes
Rua José Vilar, 300/1300 - Fortaleza (CE)
60125-000 - Brazil
E-mail:[email protected]
Submitted for publication: April 15, 2013
Accepted for publication: August 21, 2013
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: M.B.C.Fernandes, None; R.V.F.Souza, None; G.C. Vasconcelos, None; K.G.Ribeiro, None; B.B.Andrade, None; C.R.Fernandes, None.
Study was conducted in Center of Ophthalmology of Ceará - Fortaleza (CE), Brasil.
Institution whose Research Ethics Committee assessed the study: Assis Chateaubriand Teaching Maternity Hospital (protocol 80/11).