

Abrahão Rocha Lucena1; Jório Almino de Alencar Arrais Mota2; Descartes Rolim de Lucena; Sabine de Lucena Martins Ferreira; Newton Leitão de Andrade3
DOI: 10.1590/S0004-27492013000600003
ABSTRACT
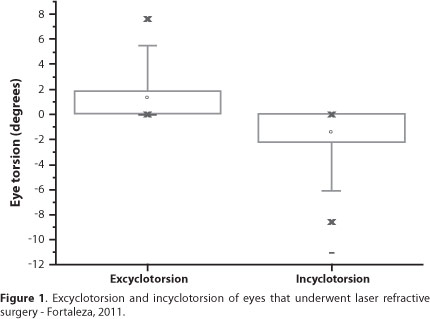
PURPOSE: The aim of this study was to verify the presence of cyclotorsion in eyes that underwent laser refractive surgery. METHODS: This was a comparative observational study, which analyzed the medical records of 61 patients (104 eyes) who underwent laser refractive surgery and compared the axis of astigmatism of the sitting and the supine positions. Regarding the gender, 37.5% were male and 62.5% were female. The age ranged from 20 to 54 years old, with the median of 29 years. The lowest degree of astigmatism was -0.75 cylinder diopters (DC) and the highest was -6.50 DC, with a mean of -3.06 ± 1.16 DC. First, the axis of astigmatism of the seated patient was captured by the Schwind's ORK-CAM. In a second moment, inside the operating room, the axis of astigmatism of the patient in supine position was captured by the laser equipment's own camera (Schwind Amaris®), which was then compared with the previous measure. The incyclotorsion was defined by a minus sign (-) and the excyclotorsion, by a plus sign (+). RESULTS: The maximum excyclotorsion was +7.7 and the maximum incyclotorsion was -11.0 degrees. The mean torsion (excyclo or incyclo) was 2.74 (56.7%), with a standard deviation of 2.30 degrees. There was no statistically significant change (p=0.985) in the axis of astigmatism between patients sitting versus supine. CONCLUSION: There was clinically significant cyclotorsion in 36.5% of the eyes submitted to laser correction.
Keywords: Astigmatism; Refractive surgical procedures; Torsion abnormality; Keratomileusis, laser in situ; Eye movement; Optical rotation
RESUMO
OBJETIVO: Verificar a presença de ciclotorção em olhos submetidos à cirurgia refrativa a laser. MÉTODOS: Realizou-se um estudo observacional comparativo, feito pela avaliação dos prontuários de 61 indivíduos (104 olhos) submetidos à cirurgia refrativa a laser, para comparar a orientação do astigmatismo ocular na posição sentada e em decúbito dorsal. Foram computados 37,5% de homens com idade variando de 20 a 54 anos, com mediana de 29 anos. O menor grau de astigmatismo avaliado foi de -0,75 e o maior de -6,50, com média de -3,06 ± 1,16 dioptrias cilíndricas (DC). A captação da orientação (eixo) do astigmatismo foi feita no primeiro momento (sentado) pelo aparelho ORK-CAM da empresa Schwind. Em um segundo momento (decúbito dorsal), na sala de cirurgia, o eixo foi captado pela câmera do próprio laser (Schwind Amaris®) para então comparar o eixo nos dois momentos. A inciclotorção foi identificada por um sinal negativo (-) e a exciclotorção por um sinal positivo (+). RESULTADOS: A exciclotorção máxima foi de +7,7 e a inciclotorção máxima de -11,0 graus. A média de torção (exciclo ou inciclo) foi de 2,74 (56,7%), com desvio padrão de 2,30 graus. Não houve variação estatisticamente significativa (p=0,985) no eixo do astigmatismo entre os indivíduos sentados versus decúbito dorsal. CONCLUSÃO: Houve ciclotorção clinicamente significativa em 36,5% dos olhos submetidos à cirurgia refrativa a laser.
Descritores: Astigmatismo; Procedimentos cirúrgicos refrativos; Anormalidade torcional; Ceratomileuse assistida por excimer laser in situ; Movimentos oculares; Rotação ocular
ORIGINAL ARTICLE
Cyclotorsion measurement in laser refractive surgery
Medida da ciclotorção em cirurgia refrativa a laser
Abrahão Rocha LucenaI; Jório Almino de Alencar Arrais MotaII; Descartes Rolim de LucenaIII; Sabine de Lucena Martins FerreiraIII; Newton Leitão de AndradeIV
IPhysician, Medical School of Ribeirão Preto, Universidade de São Paulo - Ribeirão Preto (SP), Brazil. Ceará School of Ophthalmology - Fortaleza (CE), Brazil
IIMedical student, Universidade Federal do Ceará - Fortaleza (CE), Brazil
IIIPhysician, Ceará School of Ophthalmology - Fortaleza (CE), Brazil
IVPhysician, Eye Hospital Leiria Andrade - Fortaleza (CE), Brazil
ABSTRACT
PURPOSE: The aim of this study was to verify the presence of cyclotorsion in eyes that underwent laser refractive surgery.
METHODS: This was a comparative observational study, which analyzed the medical records of 61 patients (104 eyes) who underwent laser refractive surgery and compared the axis of astigmatism of the sitting and the supine positions. Regarding the gender, 37.5% were male and 62.5% were female. The age ranged from 20 to 54 years old, with the median of 29 years. The lowest degree of astigmatism was -0.75 cylinder diopters (DC) and the highest was -6.50 DC, with a mean of -3.06 ± 1.16 DC. First, the axis of astigmatism of the seated patient was captured by the Schwind's ORK-CAM. In a second moment, inside the operating room, the axis of astigmatism of the patient in supine position was captured by the laser equipment's own camera (Schwind Amaris®), which was then compared with the previous measure. The incyclotorsion was defined by a minus sign (-) and the excyclotorsion, by a plus sign (+).
RESULTS: The maximum excyclotorsion was +7.7 and the maximum incyclotorsion was -11.0 degrees. The mean torsion (excyclo or incyclo) was 2.74 (56.7%), with a standard deviation of 2.30 degrees. There was no statistically significant change (p=0.985) in the axis of astigmatism between patients sitting versus supine.
CONCLUSION: There was clinically significant cyclotorsion in 36.5% of the eyes submitted to laser correction.
Keywords: Astigmatism; Refractive surgical procedures; Torsion abnormality; Keratomileusis, laser in situ; Eye movement; Optical rotation
RESUMO
OBJETIVO: Verificar a presença de ciclotorção em olhos submetidos à cirurgia refrativa a laser.
MÉTODOS: Realizou-se um estudo observacional comparativo, feito pela avaliação dos prontuários de 61 indivíduos (104 olhos) submetidos à cirurgia refrativa a laser, para comparar a orientação do astigmatismo ocular na posição sentada e em decúbito dorsal. Foram computados 37,5% de homens com idade variando de 20 a 54 anos, com mediana de 29 anos. O menor grau de astigmatismo avaliado foi de -0,75 e o maior de -6,50, com média de -3,06 ± 1,16 dioptrias cilíndricas (DC). A captação da orientação (eixo) do astigmatismo foi feita no primeiro momento (sentado) pelo aparelho ORK-CAM da empresa Schwind. Em um segundo momento (decúbito dorsal), na sala de cirurgia, o eixo foi captado pela câmera do próprio laser (Schwind Amaris®) para então comparar o eixo nos dois momentos. A inciclotorção foi identificada por um sinal negativo (-) e a exciclotorção por um sinal positivo (+).
RESULTADOS: A exciclotorção máxima foi de +7,7 e a inciclotorção máxima de -11,0 graus. A média de torção (exciclo ou inciclo) foi de 2,74 (56,7%), com desvio padrão de 2,30 graus. Não houve variação estatisticamente significativa (p=0,985) no eixo do astigmatismo entre os indivíduos sentados versus decúbito dorsal.
CONCLUSÃO: Houve ciclotorção clinicamente significativa em 36,5% dos olhos submetidos à cirurgia refrativa a laser.
Descritores: Astigmatismo; Procedimentos cirúrgicos refrativos; Anormalidade torcional; Ceratomileuse assistida por excimer laser in situ; Movimentos oculares; Rotação ocular
INTRODUCTION
Astigmatism is a common refractive error that generates multiple focal points over the retina. It's frequently caused by an asymmetry in the corneal curvature. When the two corneal meridians are at right angle, the ametropia can be corrected with spectacles (regular astigmatism). When there are irregularities in the meridians or they are not at right angle, it's called irregular astigmatism, and does not allow correction with spectacles(1).
Mild torsional alignment errors in the astigmatism axis (greater than 3°), can lead to a clinically significant reduction in the efficiency of the laser treatment in eyes with moderate to high astigmatism(2).
The torsional movements are defined as: a) excycloversion - when the upper pole of the eye rotates to the temporal side; b) incycloversion - when the upper pole of the eye rotates to the nasal side(3). The inferior oblique and inferior rectus muscles are responsible for the excycloversion and the superior oblique and superior rectus muscles are responsible for the incycloversion. These movements occur when we tilt our head over the shoulder or when we lay down(4).
The cyclotorsion needs to be taken into account when a corneal laser eye correction is to be done. For that an image of the seated patient's iris is photographed and compared to the same eye while in the supine position at the surgical procedure table.
To determine cyclotorsion in eyes undergoing laser refractive surgery.
METHODS
Through the evaluation of the medical records of 61 patients (104 eyes) who underwent laser refractive surgery in a reference center in the city of Fortaleza - Brazil, we performed a comparative observational study where the astigmatism axis of those individuals were recorded at two moments (pre and intraoperative), thus evaluating the eye cyclotorsion and the resulting change in the astigmatism axis to be treated.
The measures were performed in 104 eyes of 61 patients; 39 (37.5%) males. The age ranged from 20 to 54 years (median of 29 years). The lowest evaluated degree of astigmatism was -0.75 cylinder diopters (DC) and the highest was -6.50 DC (mean of -3.06 ± 1.16 D).
The first measure was performed with the patient sitting with the chin and the forehead fixed in reference to the clinical equipment (ORK-CAM, Schwind). The individual was asked to look at a primary direction of sight, while the side camera of the ORK-CAM automatically captured the image of the iris. Subsequently, the individual was moved to the operating room, now in supine position, for a second image capture of the iris with the own camera of the laser equipment (Schwind Amaris®). A memory card containing the first capture was inserted shortly after, allowing the comparison between the two images and the calculation of the cyclotorsion. The incyclotorsion was defined by a minus sign (-) and the excyclotorsion by a plus sign (+).
Data such as age and sex of the patients were also collected, as well as the degree of the astigmatism.
The study included all the available medical records where the cyclotorsion was necessary. In our service, this procedure is adopted in individuals with astigmatism greater or equal to 2 DC.
For statistical analysis, we used the software Statistical Package for Social Sciences (SPSS) version 15.0. If the parametric data distribution were symmetrical, the Student's t-test (paired samples) was applied; otherwise the Wilcoxon test was used instead. The statistical significance level was set to 0.05. In the symmetric distribution, the mean was used as a measure of central tendency; in other conditions, the median was chosen. In order to verify bivariate correlation between nonparametric data, the Spearman test was used.
RESULTS
The maximum excyclotorsion was +7.7 and the maximum incyclotorsion was -11.0 degrees (Figure 1). The mean torsion (excyclo or incyclo) was 2.74 (56.7%) with a standard deviation of 2.30 degrees. There was no statistically significant change (p=0.985) in the astigmatism axis among individuals sitting versus individuals in supine position.
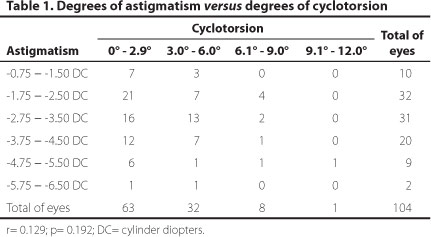
In the table 1, the astigmatism degree was separated at intervals, according to the cyclotorsion. Sixty-three (60.6%) eyes showed cyclotorsion (incyclo or excyclotorsion) between 0° and 2.9°, 32 (30.8%) eyes showed twist of between 3° and 6.0° and nine (8.6%) eyes equal to or greater than 6.1°. No correlation was observed between the astigmatism degree and the amount of cyclotorsion (r=0.109/p=0.269).
DISCUSSION
Degrees of astigmatism ranging from -0.75 to -6.50 D were treated, according to the selection criteria of each surgeon. Even without finding a statistically significant change (p=0.985) in the cyclotorsion axis of astigmatism in supine position versus primary direction of sight, a distinction should be made between what is statistically significant and what is clinically meaningful.
Small errors of alignment in the axis of astigmatism can lead to a reduction of the efficiency of laser correction(2). A rotation of 3o between the programed and the treated axis could generate a reduction of 10.0% in the efficiency of the procedure. A rotation of 7o could reduce the efficiency in 25.0%. If the rotation were 30o, the surgical effect would be zero. Additionally, the postoperative astigmatism would be greater than the preoperative one(5-7).
The higher was the astigmatism, the greater would be the visual impact of the change of its axis position during cyclotorsion(5). According to table 1, from 41 (39.4%) eyes presenting with cyclotorsion equal or greater than 3o, 38 (92.6%) had astigmatism equal or greater than -1.75 DC and 26 (63.4%) had astigmatism equal or greater than -2.75 DC. Therefore, even without observing a statistically significant difference (p=0.985) between the astigmatism axis with the patient seated versus supine position, the cyclotorsion had clinical importance (≥3o) in 38 (36.5%) eyes with astigmatism equal or greater than -1.75 DC.
CONCLUSION
Cyclotorsion was clinically significant in 36.5% of eyes that underwent laser refractive surgery.
REFERENCES
1. Ventura LO, Barros EB, Arruda Júnior JR. Sinais e sintomas das ametropias. Astigmatismo. In: Shor P, Uras R, Veitzman S. Óptica, refração e visão subnormal. Rio de Janeiro: Cultura médica; Conselho Brasileiro de Oftalmologia 2008. p.213-4. (Série oftalmologia brasileira).
2. Kwitko S, Belfort Jr. Correção cirúrgica do astigmatismo. In: Belfort Jr. R, Kara-José N, editores. Córnea clínica cirúrgica. São Paulo: Roca; 1996. p.559-73.
3. Bicas HE. Oculomotricidade e seus fundamentos. Arq Bras Oftalmol. 2001;66(5):687-700.
4. Rocha GJ, Siqueira Bisneto O, Moreira H. Estudo dos movimentos torcionais em cirurgia refrativa. Arq Bras Oftalmol. 2005;68(6):769-72.
5. Swami AU, Steinert RF, Osborne WE, White AA. Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol. 2002;133(4):561-2.
6. Helena MC. Análise vetorial do astigmatismo. In: Alves MR, Chamon W, Nosé W, editores. Cirurgia refrativa. Rio de Janeiro: Cultura Médica; 2003. p.15-9.
7. Alpins NA, Goggin M. Practical astigmatism analysis for refractive outcomes in cataract and refractive surgery. Surv Ophthalmol. 2004;49(1):109-22.
 Correspondence:
Correspondence:
Abrahão da Rocha Lucena
Av. Oliveira Paiva, 1.599 - Fortaleza (CE)
60822-131 - Brazil
E-mail: [email protected]">[email protected]
Submitted for publication: May 10, 2013
Accepted for publication: July 30, 2013
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: A.R.Lucena, None; J.A.A.A.Mota, None; D.R.Lucena, None; S.L.M.Ferreira, None; N.L.Andrade.
Study carried out at Ceará School of Ophthalmology (data collected in Visionlaser) - Brasil.