

Marcelo Carvalho Ventura1; Virgínia Vilar Sampaio1; Bruna Vieira Ventura1; Liana Oliveira Ventura1; Walton Nosé3
DOI: 10.1590/S0004-27492013000400011
ABSTRACT
PURPOSE: To report the visual outcomes and complications of congenital cataract surgery with primary intraocular lens implantation in microphthalmic eyes of children younger than 4 years of age. METHODS:This retrospective interventional case series included 14 microphthalmic eyes from 10 children who underwent congenital cataract surgery with primary intraocular lens implantation younger than 4 years of age. Seven patients had bilateral cataracts (11 eyes met the study's inclusion criteria) and 3 patients had unilateral cataract. Patients' medical charts were reviewed to obtain information regarding the preoperative and postoperative ophthalmological examination. Main outcome measures were intraocular pressure (IOP), best-corrected visual acuity, and intraoperative and postoperative complications. RESULTS: Mean age at the time of surgery was 21.7 ± 2.9 months. Mean ocular axial length was 19.2 ± 0.9 mm. Mean preoperative IOP was 9.7 ± 1.7 mmHg and 10.3 ± 3.1 mmHg on final follow-up (P=0.18). There were no intraoperative complications. Two (15.4%) eyes developed secondary visual axis opacification, of which only one needed to be reoperated due to significantly decreased vision (0.5 logMAR). Preoperative and postoperative best-corrected visual acuity was 2.09 ± 0.97 logMAR and 0.38 ± 0.08 logMAR in bilateral cases and 1.83 ± 1.04 logMAR and 0.42 ± 0.13 logMAR in unilateral cases, respectively. CONCLUSION: Primary intraocular lens implantation in congenital cataract surgery in microphthalmic eyes resulted in a significant best-corrected visual acuity improvement with no intraoperative complications and minimal postoperative complications.
Keywords: Cataract; Cataract extraction; Microphthalmos; Visual Acuity; Intraocular lenses; Postoperative complications
RESUMO
OBJETIVOS: Relatar os resultados visuais e as complicações da cirurgia de catarata congênita com implante primário de lente intraocular em olhos microftálmicos de crianças menores de 4 anos. MÉTODOS: Esta série de casos retrospectiva incluiu 14 olhos microftálmicos de 10 crianças menores de 4 anos que foram submetidas à cirurgia de catarata congênita com implante primário de lente intraocular. Sete pacientes tinham catarata bilateral (11 foram incluídos no estudo) e 3 tinham catarata unilateral. Os prontuários dos pacientes foram revisados para se obter informação sobre o exame oftalmológico pré- e pós-operatório. As principais variáveis analisadas foram pressão intraocular, acuidade visual com melhor correção e complicações intra- e pós-operatórias. RESULTADOS: A média da idade dos pacientes na época da cirurgia foi de 21,7 ± 2,9 meses. O diâmetro antero-posterior médio foi de 19,2 ± 0,9 mm. A pressão intraocular média pré-operatória foi 9,7 ± 1,7 mmHg e 10,3 ± 3,1 mmHg no último exame de acompanhamento pós-operatório (P=0,18). Não houve complicações intraoperatórias. Dois (15,4%) olhos desenvolveram opacificação secundária do eixo visual, dos quais um foi reoperado devido à baixa visual significativa (0,5 logMAR). AV pré- e pós-operatórias foram 2,09 ± 0,97 logMAR e 0,38 ± 0,08 logMAR em casos de catarata congênita bilateral e 1,83 ± 1,04 logMAR e 0,42 ± 0,13 logMAR em casos unilaterais, respectivamente. CONCLUSÃO: O implante primário de lente intraocular em cirurgia de catarata congênita em olhos microftálmicos resultou em uma melhora significativa da acuidade visual com nenhuma complicação intraoperatória e com pouca complicação no pós-operatório.
Descritores: Catarata; Extração de catarata; Microftalmia; Acuidade visual; Lente intraocular; Complicações pós-operatórias
ORIGINAL ARTICLE ARTIGO ORIGINAL
Congenital cataract surgery with intraocular lens implantation in microphthalmic eyes: visual outcomes and complications
Cirurgia de catarata congênita com implante de lente intraocular em olhos microftálmicos: resultados visuais e complicações
Marcelo Carvalho VenturaI,II; Virgínia Vilar SampaioI; Bruna Vieira VenturaI; Liana Oliveira VenturaI,II; Walton NoséIII
IPhysician, Department of Congenital Cataract, Fundação Altino Ventura - FAV - Recife, Brazil
IIPhysician, Department of Congenital Cataract, Hospital de Olhos de Pernambuco - HOPE - Recife, Brazil
IIIPhysician, Department of Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São Paulo, Brazil
ABSTRACT
PURPOSE: To report the visual outcomes and complications of congenital cataract surgery with primary intraocular lens implantation in microphthalmic eyes of children younger than 4 years of age.
METHODS:This retrospective interventional case series included 14 microphthalmic eyes from 10 children who underwent congenital cataract surgery with primary intraocular lens implantation younger than 4 years of age. Seven patients had bilateral cataracts (11 eyes met the study's inclusion criteria) and 3 patients had unilateral cataract. Patients' medical charts were reviewed to obtain information regarding the preoperative and postoperative ophthalmological examination. Main outcome measures were intraocular pressure (IOP), best-corrected visual acuity, and intraoperative and postoperative complications.
RESULTS: Mean age at the time of surgery was 21.7 ± 2.9 months. Mean ocular axial length was 19.2 ± 0.9 mm. Mean preoperative IOP was 9.7 ± 1.7 mmHg and 10.3 ± 3.1 mmHg on final follow-up (P=0.18). There were no intraoperative complications. Two (15.4%) eyes developed secondary visual axis opacification, of which only one needed to be reoperated due to significantly decreased vision (0.5 logMAR). Preoperative and postoperative best-corrected visual acuity was 2.09 ± 0.97 logMAR and 0.38 ± 0.08 logMAR in bilateral cases and 1.83 ± 1.04 logMAR and 0.42 ± 0.13 logMAR in unilateral cases, respectively.
CONCLUSION: Primary intraocular lens implantation in congenital cataract surgery in microphthalmic eyes resulted in a significant best-corrected visual acuity improvement with no intraoperative complications and minimal postoperative complications.
Keywords: Cataract/congenital; Cataract extraction/adverse effects; Microphthalmos; Visual Acuity/physiology; Intraocular lenses; Postoperative complications
RESUMO
OBJETIVOS: Relatar os resultados visuais e as complicações da cirurgia de catarata congênita com implante primário de lente intraocular em olhos microftálmicos de crianças menores de 4 anos.
MÉTODOS: Esta série de casos retrospectiva incluiu 14 olhos microftálmicos de 10 crianças menores de 4 anos que foram submetidas à cirurgia de catarata congênita com implante primário de lente intraocular. Sete pacientes tinham catarata bilateral (11 foram incluídos no estudo) e 3 tinham catarata unilateral. Os prontuários dos pacientes foram revisados para se obter informação sobre o exame oftalmológico pré- e pós-operatório. As principais variáveis analisadas foram pressão intraocular, acuidade visual com melhor correção e complicações intra- e pós-operatórias.
RESULTADOS: A média da idade dos pacientes na época da cirurgia foi de 21,7 ± 2,9 meses. O diâmetro antero-posterior médio foi de 19,2 ± 0,9 mm. A pressão intraocular média pré-operatória foi 9,7 ± 1,7 mmHg e 10,3 ± 3,1 mmHg no último exame de acompanhamento pós-operatório (P=0,18). Não houve complicações intraoperatórias. Dois (15,4%) olhos desenvolveram opacificação secundária do eixo visual, dos quais um foi reoperado devido à baixa visual significativa (0,5 logMAR). AV pré- e pós-operatórias foram 2,09 ± 0,97 logMAR e 0,38 ± 0,08 logMAR em casos de catarata congênita bilateral e 1,83 ± 1,04 logMAR e 0,42 ± 0,13 logMAR em casos unilaterais, respectivamente.
CONCLUSÃO: O implante primário de lente intraocular em cirurgia de catarata congênita em olhos microftálmicos resultou em uma melhora significativa da acuidade visual com nenhuma complicação intraoperatória e com pouca complicação no pós-operatório.
Descritores: Catarata/congênito; Extração de catarata/efeitos adversos; Microftalmia; Acuidade visual/fisiologia; Lente intraocular; Complicações pós-operatórias
INTRODUCTION
Congenital cataract is the cause of 24.8% to 29.3% of the avoidable blindness in children(1), with a prevalence varying from 1.2 to 6.0 cases per 10,000 children(2). Microphthalmos has been identified in 7.2% to 16.9% of these patients(3,4). The visual prognosis of a child with infantile cataract is related to ocular characteristics, early diagnosis and surgical treatment, associated with visual rehabilitation(5).
Advances in surgical techniques have resulted in a decrease in the incidence of complications(5). Many authors support early primary intraocular lens (IOL) implantation in the first year of life for aphakia correction in children(5,6). The goal is to decrease amblyopia and strabismus(7). Although IOL implantation is possible even in very young children, in microphthalmic eyes there are more technical difficulties(8). However, the visual prognosis of microphthalmic eyes with congenital cataract that are left aphakic is generally poor(8,9).
The purpose of the present study is to describe the visual outcomes and complications in microphthalmic eyes of children operated for unilateral or bilateral congenital cataracts with primary IOL implantation younger than 4 years of age.
METHODS
This retrospective interventional case series was approved by the Ethics Committee of the Fundação Altino Ventura (Protocol 071/09) and followed the tenets of the Declaration of Helsinki. Patients' guardians received an explanation concerning the surgical treatment and gave oral informed consent for the surgery before the procedure.
The study comprised of eyes from children younger than 4 years of age with microphthalmos, who underwent congenital cataract surgery with IOL implantation at the Altino Ventura Foundation, in Recife, Brazil, between 2005 and 2010. Microphthalmos was defined as an eye with an axial length more than 2 standard deviations smaller than the normal for that age group(10). Infants with other associated ocular abnormalities that could compromise vision, such as ocular trauma, corneal leucoma, congenital glaucoma, aniridia, persistent hyperplastic primary vitreous, chorioretinal coloboma, and chorioretinal scars, were not included. Minimum follow-up time was 6 months. Ten patients met the criteria and were included in this study.
The patients' medical charts were reviewed to obtain information regarding the preoperative ophthalmological examination, which included the measurement of the best-corrected visual acuity (BCVA), ocular extrinsic motility assessment, biomicroscopy (in cooperative patients) or inspection (in non-cooperative patients), retinoscopy under cycloplegia, and fundoscopy. Teller Acuity Cards and Lea Hyvarinen Chart were used to measure BCVA. Ocular alignment was measured using alternate cover testing. When this exam was not feasible, Krimsky test was performed.
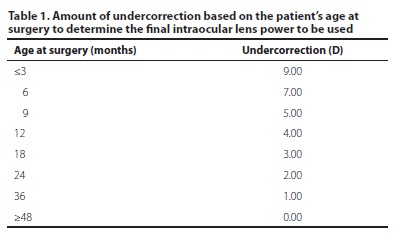
Preoperative intraocular pressure (IOP) measured with a calibrated Perkins applanation tonometer and central corneal thickness (CCT) were attained from the medical charts. These measurements had been taken before surgery, under general anesthesia. All surgeries were performed by one surgeon (M.C.V.) with a vast experience in congenital cataract surgery. A standardized surgical technique was implemented, which included phacoaspiration, posterior capsulorhexis, endocapsular tension ring implantation (endocapsular tension ring of 10/12 mm; Visiontech Medical Optics Ltda, Belo Horizonte, Brazil), anterior vitrectomy and primary IOL implantation. In all patients, a foldable, hydrophobic acrylic Type 7B IOL (Alcon, Fort Worth, USA) was placed in the capsular bag. This lens has an optical diameter of 5.5 mm and a total diameter of 12.5 mm. The IOL power was calculated based on a protocol created by one of the authors (M.C.V.)(5). The goal of this protocol is emmetropia at 4 years of age. Briefly, the IOL power is first calculated using an A-scan (DGH 4000B, DGH Technology, Inc., Exton, USA) and the Holliday II formula. Depending on the age of the child at surgery, a specific amount of undercorrection determines the final power of the IOL that will be placed (Table 1). If the child is pseudophakic in the fellow eye or has unilateral cataract, the refraction of the fellow eye is also taken into consideration to avoid anisometropias.
All patients used postoperative topical moxifloxacin 0.5% (Vigamox; Alcon Laboratories, São Paulo, São Paulo, Brazil) 4 times a day for 10 days; tropicamide 1% (Mydriacyl; Alcon Laboratories, São Paulo, São Paulo, Brazil) diluted 1:1 with artificial tears twice daily for 10 days; betaxolol 0.5% (Presmin; Latinofarma Indústrias Farmacêuticas Ltda., Cotia, São Paulo, Brazil) twice a day for 15 days; prednisolone acetate 1% (Oftpred; Latinofarma Indústrias Farmacêuticas Ltda) every 6 hours daily for a week, tapered over the next 4 weeks; and 1 mg/kg/day of prednisolone syrup (Prelone; Achè Laboratórios Farmacêuticos S.A., Guarulhos, São Paulo, Brazil) for 15 days, half the dose on the third week, and one fourth of the dose on the fourth week.
Patients returned for follow-up examinations on the 1st, 15th, 30th, 90th and 180th postoperative day, and every 6 months thereafter, unless amblyopia treatment required more frequent visits. On the 1st day, patients were examined by inspection. On the 15th day, patients were submitted to cycloplegic refraction. On the other visits, evaluation consisted of BCVA, ocular extrinsic motility, and slit lamp and fundus examination. BCVA and ocular extrinsic motility were tested as previously described. In addition, during these other visits, the children were examined under anesthesia to measure IOP, using a calibrated Perkins applanation tonometer.
Treatment for amblyopia was prescribed, which consisted of refractive error correction, patching of the dominant eye, and visual stimulation. The spectacles had an overcorrection of +2.00 D in babies to provide near point correction. When the patient started walking, a Kriptok bifocal lens with a +3.00 D for near was prescribed(5). A visual success in the congenital cataract treatment was defined as a BCVA on last follow-up equal or better than 0.5 logarithm of the minimum angle of resolution (logMAR)(11).
Statistical analysis was performed using SPSS for windows (version 12.0, SPSS, Inc.). For statistical analysis, BCVA was converted to logMAR. The results of the qualitative variables were expressed by their absolute and relative frequencies. The results of the quantitative variables were expressed by their minimum and maximum value, means, and standard deviation (SD). Normality was checked using the Kolmogorov-Smirnov test. The Spearman correlation test was used to verify the correlation between preoperative and postoperative IOP. P values <0.05 were used to reject the null hypothesis.
RESULTS
Fourteen microphthalmic eyes from 10 patients submitted to congenital cataract surgery with primary IOL implantation were included in this study. Five (50.0%) patients were male and 5 (50.0%) were female. Seven (70.0%) patients had bilateral cataracts. Of these 14 eyes, 11 met the criteria to be included in the study. The other 3 eyes were excluded because 1 had a normal axial length for their age, 1 was operated at age 6, and the third eye had a small posterior polar cataract that was not compromising the red reflex and, thus, was not operated. Three patients had unilateral cataract. The mean age at surgery was 21.7 ± 2.9 months (range, 9 to 44 months). At the time of surgery, the mean ocular axial length was 19.2 ± 0.9 mm (range, 17.5 to 20.6 mm). The mean follow-up was 38.5 ± 3.1 months (range, 23 to 48 months).
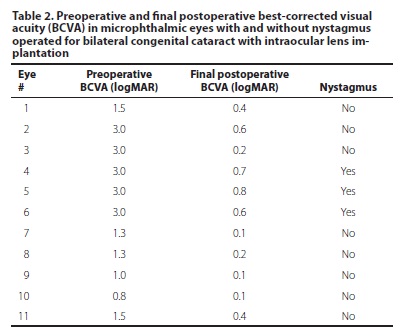
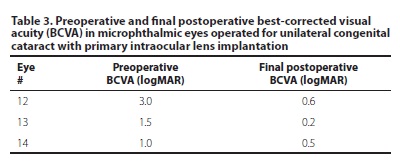
There were no surgical complications. Two eyes (15.4%) had secondary opacification of the visual axis at 6 and 8 months after the surgery (eyes #10 and #14 on tables 2 and 3, respectively). One of these eyes maintained good BCVA (0.1 logMAR) despite opacification. The other underwent further pars plana anterior vitrectomy due to significantly decreased vision (0.5 logMAR).
The central corneal thickness prior to surgery was 568.1 ± 51.5 µm (range, 493 to 644 µm). The preoperative and final postoperative mean IOP were 9.7 ± 1.7 mmHg (range, 8 to 12 mmHg) and 10.3 ± 3.1 mmHg (range, 7 to 18 mmHg), respectively. There was no significant difference in IOP before and after surgery (rho=0.06; P=0.87). Fundoscopy was normal in all patients during follow-up. There were no cases of postoperative glaucoma.
None of the patients had strabismus. Two patients (3 eyes) with bilateral congenital cataracts had preoperative nystagmus. Their mean age at surgery was 14.3 ± 3.1 months (range, 11 to 17 months). Mean preoperative BCVA was 2.09 ± 0.97 logMAR and 1.83 ± 1.04 logMAR in bilateral and unilateral cases, respectively. The mean final BCVA in patients with bilateral congenital cataracts was 0.38 ± 0.08 logMAR, including the patients with nystagmus. When evaluated separately, patients without nystagmus had a mean final BCVA of 0.23 ± 0.07 logMAR versus 0.7 ± 0.05 logMAR in the patients with nystagmus (Table 2). The mean final BCVA in patients with unilateral congenital cataracts was 0.42 ± 0.13 logMAR (Table 3).
DISCUSSION
The studied sample comprised of 14 eyes with congenital cataracts and simple microphthalmos, meaning that their axial length was small, but otherwise normal(12). They were submitted to congenital cataract surgery with primary IOL implantation younger than 4 years of age. Two eyes (15.4%) had secondary opacification of the visual axis, of which 1 required reoperation due to low vision. Previous studies in microphthalmic(1) and non-microphthalmic(13) eyes operated for congenital cataract with IOL implantation had similar rates of secondary opacification. However, others report higher incidences(14-16): Astle et al.(14), reported reopacification in 37.3% of non-microphthalmic eyes in children operated younger than 4 years of age. Many factors determine the occurrence of secondary visual axis opacification and it is known that younger children develop secondary opacifications more often(14). Acrylic IOLs are more biocompatible than poly(methyl methacrylate) (PMMA) and reduce the formation of secondary membranes(17). In addition, it has been previously reported that anterior limbic incision has a 1.66 lower risk for secondary visual axis opacification when compared to pars plicata incision(8). As we previously described(5), we use an endocapsular tension ring in infantile cataract surgery to expand the capsular bag in all its circumference to provide a stable capsular bag in despite of the implantation of a three-piece IOL with 12.5 mm of total diameter in a child's eye. This expansion and stability maintains a circular and central capsulorhexis, with the IOL functioning as a physical barrier between the posterior chamber and the vitreous cavity. We postulate that this may contribute to decrease secondary visual axis opacification(5).
Our patients' mean CCT before surgery was 568.1 ± 51.5 µm, which is slightly thicker than what has been previously described for normal children younger than 2 years of age(18). Some authros(19) reported that the Perkins tonometer is more accurate when CCT is approximately 560 to 580 µm. In the present study, no significant IOP elevation or cup-to-disc ratio alteration was verified during the follow-up period, although glaucoma is a common complication after congenital cataract surgery(14) and microphthalmos is an additional risk factor for its development.
Our patients with nystagmus had a mean age at surgery of 14.3 ± 3.1 months. Children with dense bilateral congenital cataract should ideally be operated before the development of nystagmus, which occurs in many cases after 10 weeks of age(20). Nystagmus is a predictive factor for poor visual acuity(5,9); however, the visual acuity of our patients with nystagmus improved after surgery, supporting the findings of previous papers(21,22). Yet, as expected, the improvement was not as great as in bilateral cases without nystagmus or unilateral cases. In addition, the improvement was less than what was described by Rabiah et al.(23), who reported visual results after surgery better than 0.33 in 46% of 95 patients with bilateral congenital cataract and nystagmus. These authors postulated that their better results could be due to a selection bias: the possibility of mild, non-deep-amblyogenic cataract, or the presence of developmental instead of congenital cataract(23).
In the present study, preoperative BCVA and BCVA on final follow-up visit were measured in all bilateral cases (10 eyes). Visual success was accomplished in 6 eyes (60%), which is within the range described in bilateral congenital cataract cases with primary IOL implantation in eyes without microphthalmos (33 to 85% of success)(11,24,25). Visual results in unilateral cases are generally worse than in bilateral cases(24,26,27). Our 3 cases of unilateral cataracts had a mean final BCVA of 0.42 ± 0.13, in contrast to 0.38 ± 0.08 achieved in the bilateral cases when including the eyes with nystagmus, and 0.23 ± 0.07 when excluding these eyes. Our results in unilateral cataracts are similar to a previous study, in which patients without microphthalmos achieved a mean visual acuity on last follow-up visit of 0.43(28), and better than another in which the BCVA achieved in non-microphthalmic eyes was of 0.91(29).
The results of the present study should be viewed in light of the study's limitation. This study was limited by its small sample, a result of the uncommon incidence of children with congenital cataract and microphthalmos. In addition, a longer follow-up period may reveal the development of glaucoma in some of these eyes(30).
CONCLUSION
The present study suggests that primary IOL implantation in congenital cataract surgery in microphthalmic eyes of children younger than 4 years of age can be a safe and successful treatment option for aphakia, improving visual function in unilateral and bilateral cases. However, patients have to be selected carefully and the surgery should be performed by an anterior segment surgeon familiar with the posterior segment and with broad experience in congenital cataract surgery.
REFERENCES
1. Gilbert C, Foster A. Childhood blindness in the context of VISION 2020 - The right to sight. Bull World Health Organ. 2001;79(3):227-32.
2. Lambert SR, Drack AV. Infantile cataracts. Surv Ophthalmol. 1996;40(6):427-58.
3. Kitadai SP. Frequência da microftalmia associada à catarata congênita, sua frequência etiológica e o resultado visual pós-cirúrgico [Tese]. São Paulo: Universidade Federal de São Paulo; 1999.
4. Oliveira ML, Di Giovanni ME, Porfírio Neto Jr F, Tartarella MB. Catarata congênita: aspectos diagnósticos, clínicos e cirúrgicos em pacientes submetidos a lensectomia. Arq Bras Oftalmol. 2004;67(6):921-6.
5. Ventura MC, Ventura LO, Endriss D. Congenital cataract surgery. In: Garg A, Alio JL, editors. Surgical techniques in ophthalmology: cataract surgery. 5 ed. New Deli: Jayppe Brothers Medical Publishers; 2010. p.12-9.
6. Maia NC, Lima AL, Baikoff G. Avaliação da eficácia da facectomia com implante de lente intra-ocular na infância. Arq Bras Oftalmol. 2005;68(6):735-41.
7. Birch EE, Swanson WH, Stager DR, Wood M, Everett M. Outcome after very early treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci [Internet]. 1993[cited 2010 Jul 21];34(13):3687-99. Available from: http://www.iovs.org/content/34/13/3687.long
8. Vasavada VA, Dixit NV, Ravat FA, Praveen MR, Shah SR, Vasada V, et al. Intraoperative performance and postoperative outcomes of cataract surgery in infant eyes with microphthalmos. J Cataract Refract Surg. 2009;35(3):519-28. Comment in: J Cataract Refract Surg. 2009;35(10):1844; author reply 1844-5.
9. Brito PR, Veitzman S. Causas de cegueira e baixa visão em crianças. Arq Bras Oftalmol. 2000;63(1):49-54.
10. Sampaolesi R. Ecometria ocular en el diagnostico de glaucoma congenito. In: Sampaolesi R. Ultrasonidos en oftalmologia. Buenos Aires: Editorial Medica Panamericana; 1984. p.461-89.
11. Crouch ER Jr, Pressman SH, Crouch ER. Posterior chamber intraocular lenses: long-term results in pediatric cataract patients. J Pediatr Ophthalmol Strabismus. 1995; 32(4):210-8.
12. Elder MJ. Aetiology of severe visual impairment and blindness in microphthalmos. Br J Ophthalmol. 1994;78(5):332-4.
13. Watts P, Abdolell M, Levin AV. Complications in infants undergoing surgery for congenital cataract in the first 12 weeks of life: is early surgery better? J AAPOS. 2003; 7(2):81-5.
14. Astle WF, Alewenah O, Ingram AD, Paszuk A. Surgical outcomes of primary foldable intraocular lens implantation in children: understanding posterior opacification and the absence of glaucoma. J Cataract Refract Surg. 2009;35(7):1216-22.
15. Trivedi RH, Wilson ME Jr, Bartholomew LR, Lal G, Peterseim MM. Opacification of the visual axis after cataract surgery and single acrylic intraocular lens implantation in the first year of life. J AAPOS. 2004;8(2):156-64.
16. Lu Y, Ji Y, Luo Y, Jiang Y, Wang M, Chen X. Visual results and complications of primary intraocular lens implantation in infants aged 6 to 12 months. Graefes Arch Clin Exp Ophthalmol. 2010;248(5):681-6.
17. Argento C, Badoza D, Ugrin C. Optic capture of the AcrySof intraocular lens in pediatric cataract surgery. J Cataract Refract Surg. 2001;27(10):1638-42.
18. Hussein MA, Paysse EA, Bell NP, Coats DK, Brady McCreery KM, Koch DD, et al. Corneal thickness in children. Am J Ophthalmol. 2004;138(5):744-8.
19. Whitacre MM, Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993;115(5):592-6.
20. Rogers GL, Tishler CL, Tsou BH, Hertle RW, Fellows RR. Visual acuities in infants with congenital cataracts operated on prior to 6 months of age. Arch Ophthalmol. 1981;99(6): 999-1003.
21. Gelbart SS, Hoyt CS, Jastrebski G, Marg E. Long-term visual results in bilateral congenital cataracts. Am J Ophthalmol. 1982;93(5):615-21.
22. Robb RM, Petersen RA. Outcome of treatment for bilateral congenital cataracts. Ophthalmic Surg. 1992;23(10):650-6.
23. Rabiah PK, Smith SD, Awad AH, Al-garni A, Al-mesfer SA, Al-turkmani S. Results of surgery for bilateral cataract associated with sensory nystagmus in children. Am J Ophthalmol. 2002;134(4):586-91.
24. Lesueur LC, Arné JL, Chapotot EC, Thouvenin D, Malecaze F. Visual outcome after paediatric cataract surgery: is age a major factor? Br J Ophthalmol [Internet]. 1998[cited 2010 Jan 2];82(9):1022-5. Available from: http://bjo.bmj.com/content/82/9/1022.long
25. Ondrácek O, Lokaj M. Visual outcome after congenital cataract surgery. Long-term clinical results. Scripta Med (Brno). 2003;76(2):95-102.
26. You C, Wu X, Zhang Y, Dai Y, Huang Y, Xie L. Visual impairment and delay in presentation for surgery in chinese pediatric patients with cataract. Ophthalmology. 2011; 118(1):17-23.
27. Chak M, Wade A, Rahi JS; British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British Congenital Cataract Study. Invest Ophthalmol Vis Sci [Internet]. 2006[cited 2010 Mar 19]; 47(10):4262-9. Available from: http://www.iovs.org/content/47/10/4262.long
28. Autrata R, Rehurek J, Vodicková K. Visual results after primary intraocular lens implantation or contact lens correction for aphakia in the first year of age. Ophthalmologica. 2005;219(2):72-9.
29. Hussin HM, Markham R. Long-term visual function outcomes of congenital cataract surgery with intraocular lens implantation in children under 5 years of age. Eur J Ophthalmol. 2009;19(5):754-61.
30. Wilson ME, Peterseim MW, Englert JA, Lall-Trail JK, Elliott LA. Pseudophakia and polypseudophakia in the first year of life. J AAPOS. 2001;5(4):238-45.
 Correspondence address:
Correspondence address:
Marcelo C. Ventura.
Fundação Altino Ventura - FAV.
Rua da Soledade, 170 - Recife (PE) - 50070-040 - Brazil
E-mail: [email protected]
Submitted for publication: April 2, 2013
Accepted for publication: May 24, 2013
Study carried out at Fundação Altino Ventura - FAV.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: M.C.Ventura, None; V.V.Sampaio, None; B.V.Ventura, None; L.O.Ventura, None; W.Nosé, None.
This study was approved by the Ethics Committee of the Fundação Altino Ventura (Protocol 071/09).