

Luciane Bugmann Moreira1; Ricardo Augustho Canto Bardal2; Leila Roberta Crisigiovanni
DOI: 10.1590/S0004-27492013000400004
ABSTRACT
PURPOSE: Evaluate contact lenses fitting after intracorneal ring implantation for keratoconus, its visual acuity and comfort. METHODS: Retrospective study of patients undergoing contact lenses fitting, after intracorneal ring for keratoconus. The criterion for contact lens fitting was unsatisfactory visual acuity with spectacle correction as referred by the patients. All patients were intolerants to contact lenses prior to intracorneal implantation. Visual acuity analysis was done by conversion of Snellen to logMAR scales. The comfort was evaluated according subjective questioning of good, medium or poor comfort. RESULTS: Nineteen patients were included in the study. Two patients (10.5%) did not achieved good comfort with contact lenses and underwent penetrating keratoplasties. All the others 17 patients showed good or medium comfort. Four rigid gas-permeable contact lenses were fitted, one piggyback approach, 3 toric soft contact lenses, 2 soft lenses specially design for keratoconus and 7 disposable soft lenses. The average visual acuity improved from 0.77 ± 0.37 to 0.19 ± 0.13 logMAR units after contact lenses fitting. CONCLUSION: Contact lens fitting after intracorneal ring is possible, provides good comfort, improves visual acuity, and therefore, may postpone the need for penetrating keratoplasty.
Keywords: Contact lenses; Corneal stroma; Prostheses and implants; Keratoconus Visual acuity; Adaptation, ocular
RESUMO
OBJETIVOS: Avaliar a adaptação de lentes de contato após implante de anel intracorneano para ceratocone perante a acuidade visual e o conforto. Local: Hospital de Olhos do Paraná, Curitiba, Paraná. MÉTODOS: Estudo retrospectivo de pacientes submetidos à adaptação de lentes de contato após implante de anel intracorneano em pacientes com ceratocone. A impossibilidade do uso de lentes de contato foi usada como critério para indicação de implante de anel intracorneano, sendo a adaptação de lentes de contato reservada aos pacientes com acuidade visual menor que o desejado após o implante. A acuidade visual foi considerada segundo a correlação entre a tabela de Snellen e a tabela de logMAR. O conforto foi avaliado segundo o questionamento subjetivo entre lentes confortáveis, conforto moderado e lentes desconfortáveis. RESULTADOS: Foram incluídos 19 pacientes no estudo. Apenas 2 pacientes (10,5%) não alcançaram um conforto adequado com as lentes de contato, sendo encaminhados para transplante de córnea. Nos outros 17 pacientes foram adaptadas: 4 lentes de contato rígidas gás-permeáveis, 1 sistema à cavaleiro, 3 lentes de contato gelatinosas tóricas, 2 lentes para ceratocone e 7 lentes gelatinosas descartáveis. A acuidade visual média melhorou de 0,7 ± 0,3 para 0,2 ± 0,1 unidades logMAR após a adaptação das lentes de contato. CONCLUSÃO: Adaptação de lentes de contato após anel intracorneano é possível, resulta em bom conforto e melhora da acuidade visual. Todas lentes de contato gelatinosas adaptadas demonstraram-se confortáveis. Esta adaptação pode ser útil aos pacientes que desejem adiar o transplante de córnea.
Descritores: Lentes de contato; Substância própria; Próteses e implantes; Ceratocone; Acuidade visual; Adaptação ocular
ORIGINAL ARTICLE ARTIGO ORIGINAL
Contact lenses fitting after intracorneal ring segments implantation in keratoconus
Adaptação de lentes de contato após implante de anel intracorneano no ceratocone
Luciane Bugmann MoreiraI; Ricardo Augustho Canto BardalII; Leila Roberta CrisigiovanniIII
IPhysician, Faculdade Evangélica de Medicina do Paraná - Curitiba (PR), Brasil
IIPhysician, Hospital Universitário Evangélico de Curitiba - Curitiba (PR), Brasil
IIIPhysician, Curitiba (PR), Brasil
ABSTRACT
PURPOSE: Evaluate contact lenses fitting after intracorneal ring implantation for keratoconus, its visual acuity and comfort.
METHODS: Retrospective study of patients undergoing contact lenses fitting, after intracorneal ring for keratoconus. The criterion for contact lens fitting was unsatisfactory visual acuity with spectacle correction as referred by the patients. All patients were intolerants to contact lenses prior to intracorneal implantation. Visual acuity analysis was done by conversion of Snellen to logMAR scales. The comfort was evaluated according subjective questioning of good, medium or poor comfort.
RESULTS: Nineteen patients were included in the study. Two patients (10.5%) did not achieved good comfort with contact lenses and underwent penetrating keratoplasties. All the others 17 patients showed good or medium comfort. Four rigid gas-permeable contact lenses were fitted, one piggyback approach, 3 toric soft contact lenses, 2 soft lenses specially design for keratoconus and 7 disposable soft lenses. The average visual acuity improved from 0.77 ± 0.37 to 0.19 ± 0.13 logMAR units after contact lenses fitting.
CONCLUSION: Contact lens fitting after intracorneal ring is possible, provides good comfort, improves visual acuity, and therefore, may postpone the need for penetrating keratoplasty.
Keywords: Contact lenses; Corneal stroma; Prostheses and implants; Keratoconus Visual acuity; Adaptation, ocular
RESUMO
OBJETIVOS: Avaliar a adaptação de lentes de contato após implante de anel intracorneano para ceratocone perante a acuidade visual e o conforto. Local: Hospital de Olhos do Paraná, Curitiba, Paraná.
MÉTODOS: Estudo retrospectivo de pacientes submetidos à adaptação de lentes de contato após implante de anel intracorneano em pacientes com ceratocone. A impossibilidade do uso de lentes de contato foi usada como critério para indicação de implante de anel intracorneano, sendo a adaptação de lentes de contato reservada aos pacientes com acuidade visual menor que o desejado após o implante. A acuidade visual foi considerada segundo a correlação entre a tabela de Snellen e a tabela de logMAR. O conforto foi avaliado segundo o questionamento subjetivo entre lentes confortáveis, conforto moderado e lentes desconfortáveis.
RESULTADOS: Foram incluídos 19 pacientes no estudo. Apenas 2 pacientes (10,5%) não alcançaram um conforto adequado com as lentes de contato, sendo encaminhados para transplante de córnea. Nos outros 17 pacientes foram adaptadas: 4 lentes de contato rígidas gás-permeáveis, 1 sistema à cavaleiro, 3 lentes de contato gelatinosas tóricas, 2 lentes para ceratocone e 7 lentes gelatinosas descartáveis. A acuidade visual média melhorou de 0,7 ± 0,3 para 0,2 ± 0,1 unidades logMAR após a adaptação das lentes de contato.
CONCLUSÃO: Adaptação de lentes de contato após anel intracorneano é possível, resulta em bom conforto e melhora da acuidade visual. Todas lentes de contato gelatinosas adaptadas demonstraram-se confortáveis. Esta adaptação pode ser útil aos pacientes que desejem adiar o transplante de córnea.
Descritores: Lentes de contato; Substância própria; Próteses e implantes; Ceratocone; Acuidade visual; Adaptação ocular
INTRODUCTION
Keratoconus is an eye condition where the cornea becomes thinner and starts to protrude, forming an irregular cone-like shape(1). This ectasia normally begins at puberty and progressively leads to different degrees of visual impairment varying according to the stage of the disease(2). At the beginning may be asymptomatic, however, with the evolution it induces a low visual acuity or image distortion and may be associated with photophobia, glare and ocular itching(3).
The treatment of keratoconus is customized and depends on the severity of the disease, ocular sensitivity and psychosocial aspects of the patient(4,5). For visual improvement can be used: glasses, soft contact lenses, rigid gas permeable (RGP) contact lenses, intracorneal rings segments (ICRS) implantation, lamellar keratoplasty, penetrating keratoplasty and the photorefractive keratectomy (PRK) associated with crosslinking(2,6-8).
Spectacles provide good visual acuity (VA) only in the early stages of the disease, in more regular corneas(2). With the progression of the astigmatism, RGP contact lenses become more effective to improve vision(9). Many lens designs and methods can be used for this purpose. Multicurve sets with specific parameters designed for keratoconic corneas have many curves progressively flatter to align with the cornea as best as possible are the most used. However, there are other options as aspheric contact lens that vault the apex of the cone and align the more normal peripheral cornea, hybrid contact lenses manufactured by combining a highly oxygen-permeable rigid center with a soft peripheral skirt, scleral and semi-scleral lenses with a large diameter. Custom soft contact lenses specially designed can correct mild-to-moderate keratoconus also can be used. Piggyback fit is a method fitting a RGP lens over a soft lens and has been used successfully in patients with difficulties in adapting RGP lenses(10,11).
Surgical treatment is reserved for cases when contact lenses can no longer be fitted, become intolerable or do not provide good visual acuity(12). Alternative surgical techniques, such as the implantation of ICRS have been developed to try to avoid or postpone penetrating keratoplasties(13).
Intracorneal ring segments are intended to change the corneal curvature, improving visual acuity with absence of endothelial rejection; however, some patients may remain with residual ammetropias, requiring optical correction(14). In this context, the adaptation of contact lenses after implantation of ICRS becomes an option to improve visual acuity of patients who are not satisfied(9).The same lens designs and methods used for keratoconus can be used for this purpose.
The prevalence of the disease in the population, the technical difficulty to fit contact lenses after ICRS(15), and the lack of scientific articles in the literature about the subject stimulated this research.
The purpose of this work is to evaluate visual acuity and comfort of contact lenses fitting after ICRS implantation for keratoconus.
METHODS
Retrospective study with analysis of medical records of patients who underwent contact lenses fitting after ICRS for keratoconus held at Hospital de Olhos do Paraná, located in Curitiba, Paraná, Brazil.
The study was reviewed and approved by the Ethics and Research Committee of the Positivo University.
The inclusion criterion for contact lens fitting was unsatisfactory visual acuity with spectacle correction as referred by the patients.
Complete eye exam was performed, followed by corneal topography by (EyeSys Technologies®, Dallas, USA).
Visual acuity analysis was done by conversion of Snellen to logMAR scales(16). Student t-test was used to compare visual acuity. Spectacle-corrected visual acuity was considered prior to ICRS implantation, considering that all patients were intolerant to contact lenses prior to surgery. Uncorrected visual acuity was considered after ICRS implantation and before contact lens fitting, as well as after contact lens fitting.
Analysis of comfort was done by a subjective parameter, being judged by the patient and classified in: good, moderate or poor comfort.
RESULTS
A total of 19 patients were included in the study, being 9 men and 10 women, age ranged from 18 to 41 years old (mean of 27 years old).
The analysis of visual acuity from each patient can be found in table 1. Average visual acuity before ICRS implantation was 1.26 ± 0.63 logMAR and improved to 0.77 ± 0.37 logMAR after ICRS implantation and before the adaptation of contact lenses (p<0.001). Further improvement was observed after contact lens fitting over the ICRS up to 0.19 ± 0.13 logMAR (p<0.001).

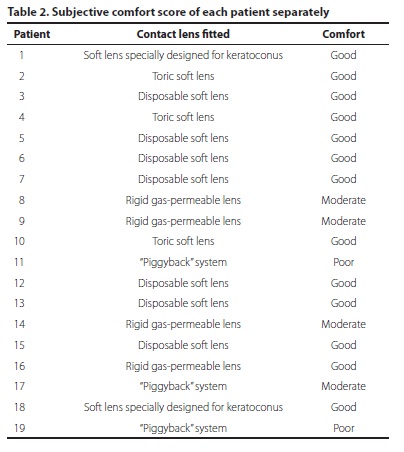
Table 2 shows the 19 contact lenses adapted, 12 (63%) were soft and 7 (37%) were rigid gas-permeable lenses. Analyzing the comfort reported by patients, 13 of them refered good comfort (68.5%), being 12 soft lenses and one RGP lens users; 4 (21%) patients had moderate comfort with the lenses tested, 3 lenses of these were RGP and one with a piggyback fit; and 2 (10.5%) patients, who needed piggyback fit, judged poor comfort and were referred to undergo corneal transplant.
DISCUSSION
The present study analyzes a series of 19 cases, being able to show percentages, different from the literature that shows only isolated case reports(17-20).
The visual acuity improvement observed in this series is compatible with already published studies. This clearly demonstrates the role of contact lens in the improvement of visual acuity of these patients, however the data found in the literature do not allow to estimate by which time interval this accuracy is maintained.
Evaluating the comfort performance through a subjective range, it was observed that most of the patients (68.5%) obtained a good comfortable with proposals lenses, showing that contact lens fitting after intracorneal ring is feasible and with good acceptance by patients.
Making an analogy of this information with others studies on quality of life in patients with keratoconus, we can assume that the patient using lenses associated with corneal ring improves not only your vision but also your quality of life(5).
Analyzing the lenses data, it was found that all soft lenses reached a good comfort and only one RGP lens adapted reached the same. It goes in accordance with data found in the literature that refer higher comfort for soft lenses(21).
For 7 cases soft contacts did not reach good visual acuity and needed a rigid gas permeable lens fitting, however the RGP lens demonstrated a worse comfort. In an attempt to give more comfort, we tried the piggyback fitting in 3 patients. Despite the attempt, 2 patients continued their poor comfort and were referred to undergo corneal transplant. Piggyback fitting was well tolerated in a prior published case report(18).
CONCLUSION
Contact lenses fitting after intracorneal rings segments implantation is possible and provides good comfort with improvement of visual acuity. For those patients studied, soft lenses had better acceptance in comparison with the other lenses tested.
REFERENCES
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophtalmol. 1984;28(4):293-322.
2. Kanski JJ, Menon J. Oftalmologia clínica: uma abordagem sistemática. Rio de Janeiro: Elsevier; 2004.
3. Kara-José N, Bechara SJ. Ceratocone. In: Newton KJ, Belfort Jr R. organizadores. Córnea clínica - cirúrgica. São Paulo: Roca; 1996. p.359-66.
4. Buxton JN, Keatles RH, Hoefle FB. The contact lens correction of keratoconus. In: Dabezies OH Jr. The CLAO guide to basic science and clinical practice. Orlando: Grune & Statton; 1984. p.55.1-14.
5. Moreira LB, Alchieri JC, Belfort R Jr., Moreira H. Aspectos psicossociais do paciente com ceratocone. Arq Bras Oftalmol. 2007;70(2):317-22.
6. Keating A, Pineda R 2nd, Colby K. Corneal cross linking for keratoconus. Semin Ophthalmol. 2010;25(5-6):249-55.
7. Renesto AC, Sartori M, Campos M. [Cross-linking and intrastomal corneal ring segment]. Arq Bras Oftalmol. 2011;74(1):67-74. Portuguese.
8. Espandar L, Meyer J. Keratoconus: overview and update on treatment. Middle East Afr J Ophthalmol. 2010;17(1):15-20.
9. Coral-Ghanem C, Alves MR. [Fitting Monocurve and Bicurve (Soper-McGuire design) rigid gas-permeable contact lenses in keratoconus patients: a prospective randomized comparative clinical trial]. Arq Bras Oftalmol. 2008;71(3):328-36. Portuguese.
10. Yamazaki ES, da Silva VC, Morimtsu V, Sobrinho M, Fukushima N, Lipener C. [Keratoconus special soft contact lens fitting]. Arq Bras Oftalmol. 2006;69(4):557-60. Portuguese.
11. Gomes JP, Lani LA, Juliano YG, Pedro EA, Anbar R. Uso da topografia de córnea na adaptação de lente de contato rígida gás-permeável em pacientes portadores de ceratocone: descrição de técnica e resultados preliminares. Arq Bras Oftalmol. 2002; 65(5):519-23.
12. Mascaro VL, Scarpi MJ, Hofling-Lima AL, Sousa LB. Transplante de córnea em ceratocone: avaliação dos resultados e complicações obtidos por cirurgiões experientes e em treinamento. Arq Bras Oftalmol. 2007;70(3):395-405.
13. Moreira H, Oliveira CS, Godoy G, Wahab SA. Anel intracorneano de Ferrara em ceratocone. Arq Bras Oftalmol. 2002;65(1):59-63.
14. Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26(8):1117-22. Comment in: J Cataract Refract Surg. 2000; 26(8):1099-100. J Cataract Refract Surg. 2001;27(3):341.
15. Cunha PF, Alves EA, Silva FB, Cunha GH. Estudo das modificações oculares induzidas pelo implante estromal do anel de Ferrara em portadores de ceratocone. Arq Bras Oftalmol. 2003;66(4):417-22.
16. Johnson GJ, Minassian DC, Weale RA, editors. The epidemiology of eye diseases. London: Chapman & Hall; 2003.
17. Hladun L, Harris M. Contact lens fitting over intrastromal corneal rings in a keratoconic patient. Optometry. 2004;75(1):48-54.
18. Smith K, Carrell J. High-Dk. piggyback contact lenses over intacs for keratoconus: a case report. Eye Contact Lens. 2008;34(4):238-41.
19. Uçakhan OO, Kanpolat A, Ozdemir O. Contact lens fitting for keratoconus after Intacs placement. Eye Contact Lens. 2006;32(2):75-7.
20. Dalton K, Sorbara L. Fitting an MSD (mini scleral design) rigid contact lens in advanced keratoconus with INTACS. Cont Lens Anterior Eye. 2011;34(6):274-81.
21. Leal F, Lipener C, Chalita MR, Uras R, Campos M, Hofling-Lima AL. Lente de contato de material híbrido em pacientes com ceratocone e astigmatismo miópico composto. Arq Bras Oftalmol. 2007;70(2):247-54.
 Correspondence address:
Correspondence address:
Ricardo Augustho Canto Bardal.
Hospital Universitário Evangélico de Curitiba.
Rua Brigadeiro Franco, 125 - Apto. 42
Curitiba (PR) - 80430-210 - Brazil
E-mail: [email protected]
Submitted for publication: December 21, 2012
Accepted for publication: May 8, 2013
Study carried out at Hospital Universitário Evangélico de Curitiba - Curitiba (PR), Brasil.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: L.B.Moreira, None; R.A.C.Bardal, None; L.R.Crisgiovanni, None.