

Fabio Lavinsky1; Noah Avni-Zauberman1; Irina S Barequet1
DOI: 10.1590/S0004-27492013000300009
ABSTRACT
PURPOSES: Microbial keratitis is commonly diagnosed worldwide, and continues to cause significant ocular morbidity, requiring prompt and appropriate treatment. The objective of this study is to describe the clinical characteristics and outcomes of patients with presumed microbial keratitis admitted to The Goldschleger Eye Institute, Sheba Medical Center, Tel Aviv University, Tel Hashomer, Israel. METHODS: A cross-sectional study was conducted, in which the medical records of patients with presumed microbial keratitis admitted during a period of 3 years were reviewed. RESULTS: Keratitis was diagnosed in 276 patients (51% males and 48.9% females). The mean age was 39.29 ± 22.30 years. The hospital length of stay ranged from 1 to 65 days (mean 5.69 ± 5.508). Fortified antibiotics were still used at discharge in 72% of the cases. Overall visual acuity improved significantly from the time of admission to the 1st-week follow up visit showing a p<0.001 on the Wilcoxon signed ranks test. Contact lens wearing was present in 36.1% of the patients, although there was no significant relation with severity of the presentation and visual outcome (p>0.05). The degree of hypopyon and cells in the anterior chamber was significantly related to the hospital length of stay (r Spearman=0.31; p<0.001 and r Spearman=0.21; p<.001, respectively) as well as to a worse visual outcome (r Spearman=0.32; p<0.01 and r Spearman=0.18; p=0.01, respectively). Of all patients, 2.3% required an urgent therapeutic penetrating keratoplasty, and 1% underwent evisceration. There was no enucleation. CONCLUSION: Treating keratitis aggressively and assuring patient compliance is imperative for a good final visual outcome. Inpatient treatment may have a positive impact on this outcome.
Keywords: Cornea; Keratitis; Eye infection, bacterial; Eye infection, fungal; Prognosis; Cross-sectional studies; Tertiary healthcare; Israel
RESUMO
OBJETIVOS: Ceratite microbiana é comumente diagnosticada em todo mundo e ainda continua a causar uma significante morbidade ocular. É necessário tratá-la de forma imediata e apropriada. O objetivo deste estudo é descrever as características clínicas e os desfechos dos pacientes com ceratite microbiana presumida que foram internados no Goldschlager Eye Institute, Sheba Medical Center, Tel Aviv University, Israel. MÉTODOS: Um estudo transversal foi realizado onde arquivos hospitalares dos pacientes internados com ceratite microbiana presumida durante um periodo de três anos foram analisados e revisados. RESULTADOS: Ceratite foi diagnosticada em 276 pacientes (51% masculinos e 48,9% femininos). A média de idade foi 39,29 ± 22,30 anos. A duração da internação foi de 1 a 65 dias (média 5,69 ± 5,508). Antibióticos fortificados permaneceram usados na alta em 72% dos casos. A acuidade visual do seguimento da primeira semana após a alta em relação a internação melhorou na media de forma estatisticamente significativa (p<0,001 usando Wilcoxon signed ranks test). O uso de lentes de contato estava presente em 36,1% dos pacientes, porém não houve relação estatisticamente significativa entre a gravidade da apresentação clínica e a acuidade visual nestes pacientes (p>0,05). O grau de hipópio e células na câmara anterior foram estatisticamente significativos em relação ao tempo de internação (r Spearman=0,0.31; p<0,001 and r Spearman=0,21; p<0,001, respectivamente) e para a acuidade visual (r Spearman=0,32; p<0,01 e r Spearman=0,18; p=0,01, respectivamente). De todos os pacientes, apenas 2,3% necessitaram ceratoplastia penetrante urgente e 1% necessitaram evisceração. Não houve enucleações. CONCLUSÕES: Tratar a ceratite de forma agressiva e garantir a aderência do paciente ao tratamento é imperativo para o bom resultado visual final. O tratamento internado pode ter um impacto positivo neste desfecho.
Descritores: Córnea; Ceratite; Infecções oculares bacterianas; Infecções oculares fúngicas; Prognóstico; Estudos transversais; Atenção terciária à saúde; Israel
ORIGINAL ARTICLE ARTIGO ORIGINAL
Clinical characteristics and outcomes of patients admitted with presumed microbial keratitis to a tertiary medical center in Israel
Características clínicas e desfechos dos pacientes internados com diagnóstico de ceratite microbiana em um centro terciário em Israel
Fabio Lavinsky; Noah Avni-Zauberman; Irina S Barequet
Physician, Goldschleger Eye Institute, Sheba Medical Center, Tel Aviv University Sackler, Faculty of Medicine, Tel Hashomer, Israel
ABSTRACT
PURPOSES: Microbial keratitis is commonly diagnosed worldwide, and continues to cause significant ocular morbidity, requiring prompt and appropriate treatment. The objective of this study is to describe the clinical characteristics and outcomes of patients with presumed microbial keratitis admitted to The Goldschleger Eye Institute, Sheba Medical Center, Tel Aviv University, Tel Hashomer, Israel.
METHODS: A cross-sectional study was conducted, in which the medical records of patients with presumed microbial keratitis admitted during a period of 3 years were reviewed.
RESULTS: Keratitis was diagnosed in 276 patients (51% males and 48.9% females). The mean age was 39.29 ± 22.30 years. The hospital length of stay ranged from 1 to 65 days (mean 5.69 ± 5.508). Fortified antibiotics were still used at discharge in 72% of the cases. Overall visual acuity improved significantly from the time of admission to the 1st-week follow up visit showing a p<0.001 on the Wilcoxon signed ranks test. Contact lens wearing was present in 36.1% of the patients, although there was no significant relation with severity of the presentation and visual outcome (p>0.05). The degree of hypopyon and cells in the anterior chamber was significantly related to the hospital length of stay (r Spearman=0.31; p<0.001 and r Spearman=0.21; p<.001, respectively) as well as to a worse visual outcome (r Spearman=0.32; p<0.01 and r Spearman=0.18; p=0.01, respectively). Of all patients, 2.3% required an urgent therapeutic penetrating keratoplasty, and 1% underwent evisceration. There was no enucleation.
CONCLUSION: Treating keratitis aggressively and assuring patient compliance is imperative for a good final visual outcome. Inpatient treatment may have a positive impact on this outcome.
Keywords: Cornea; Keratitis/diagnosis; Eye infection, bacterial; Eye infection, fungal; Prognosis; Cross-sectional studies; Tertiary healthcare; Israel
RESUMO
OBJETIVOS: Ceratite microbiana é comumente diagnosticada em todo mundo e ainda continua a causar uma significante morbidade ocular. É necessário tratá-la de forma imediata e apropriada. O objetivo deste estudo é descrever as características clínicas e os desfechos dos pacientes com ceratite microbiana presumida que foram internados no Goldschlager Eye Institute, Sheba Medical Center, Tel Aviv University, Israel.
MÉTODOS: Um estudo transversal foi realizado onde arquivos hospitalares dos pacientes internados com ceratite microbiana presumida durante um periodo de três anos foram analisados e revisados.
RESULTADOS: Ceratite foi diagnosticada em 276 pacientes (51% masculinos e 48,9% femininos). A média de idade foi 39,29 ± 22,30 anos. A duração da internação foi de 1 a 65 dias (média 5,69 ± 5,508). Antibióticos fortificados permaneceram usados na alta em 72% dos casos. A acuidade visual do seguimento da primeira semana após a alta em relação a internação melhorou na media de forma estatisticamente significativa (p<0,001 usando Wilcoxon signed ranks test). O uso de lentes de contato estava presente em 36,1% dos pacientes, porém não houve relação estatisticamente significativa entre a gravidade da apresentação clínica e a acuidade visual nestes pacientes (p>0,05). O grau de hipópio e células na câmara anterior foram estatisticamente significativos em relação ao tempo de internação (r Spearman=0,0.31; p<0,001 and r Spearman=0,21; p<0,001, respectivamente) e para a acuidade visual (r Spearman=0,32; p<0,01 e r Spearman=0,18; p=0,01, respectivamente). De todos os pacientes, apenas 2,3% necessitaram ceratoplastia penetrante urgente e 1% necessitaram evisceração. Não houve enucleações.
CONCLUSÕES: Tratar a ceratite de forma agressiva e garantir a aderência do paciente ao tratamento é imperativo para o bom resultado visual final. O tratamento internado pode ter um impacto positivo neste desfecho.
Descritores: Córnea; Ceratite/diagnóstico; Infecções oculares bacterianas; Infecções oculares fúngicas; Prognóstico; Estudos transversais; Atenção terciária à saúde; Israel
INTRODUCTION
Microbial keratitis is commonly diagnosed worldwide, and continues to cause significant ocular morbidity, requiring prompt and appropriate treatment(1,2). A large retrospective cohort recently reported an incidence of ulcerative keratitis of 27.6/100,000 person- years (95% confidence interval, 24.6-30.9)(3).
Predisposing factors for microbial keratitis described in the literature, include: previous ocular surgery, contact lens use, trauma and metal foreign body, surgical sutures, ocular surface disease, topical corticosteroid use, herpetic keratitis, lid misalignment, and systemic diseases such as diabetes and smoking(4-16). Predictive factors for outcome such as initial visual acuity at admission have not been widely described in previous studies.
Previous reports describe a variability of etiological agents in different centers around the world(2,4,5,7,8,13,14,16). Empirical, broadspectrum treatment of keratitis is a strategy selected by many ophthalmologists(17-21). However the increased resistence of the causative microorganism to currently available anti-infective drugs requires ongoing assessment of the trends of clinical and microbiological evaluation of the patients(22).
An earlier survey from a decade ago of the causative agents of ophthalmic infections in an Israeli ophthalmology service showed that coagulase-positive staphylococcus was the most common isolate from corneal ulcers (33.3%)(23). The combination of warm and humid climate along with the popularity of the contact lens wear may predispose to unique features of microbial keratitis in this region. Therefore, in the current study, we analyzed the demographic and clinical characteristics, the risk factors and the clinical outcomes of patients with keratitis admitted to our department that serves as primary, secondary and tertiary center.
METHODS
In this cross-sectional study, records of all patients admitted to our department with a diagnosis of keratitis over a period of 24 months were analyzed. The department serves as a primary, secondary and tertiary referral center. The admitting policy includes hospitalization when the infiltrate is more severe than very mild. Patients are discharged when the infiltrate is responding to treatment, the epithelial defect is closed, and there is no anterior chamber reaction.
Cases were excluded from the analysis if no follow-up visit was registered on the records. The review of the charts was authorized by the hospital directory. The legislation rules of the ethical committee at our institution did not require at that time approval for retrospective data analysis. Data was abstracted for age, gender, hospital length of stay, and season of admission. Predisposing factors such as contact lens use, previous ocular surgery, trauma and foreign body were also recorded. Visual acuity was measured with Snellen charts with the best correction obtained with spectacles or pinhole. The size of the infiltrate was ranked from 1 to 3, where 1 corresponds to an infiltrate of up to 1 mm of diameter, 2 refers to 1 to 2 mm and 3 means over 2 mm. Anterior chamber reaction was measured according to standard parameters of the ophthalmological practice. Cells and flare were measured in a 1-4 scale and hypopyon was measured in millimeters. In addition, the microbiological profile was accessed: the results of cultures of patients that underwent scrapings were analyzed and their relationship with visual outcome was assessed and compared with the population that has not undergone scrapings. The initial antibiotic treatment was also reviewed. The fact that patients are discharged with the same criteria validates the analysis performed using visual acuity at the 7-day post-discharge follow-up visit as an outcome.
The following risk factors for keratitis were analyzed: previous systemic diseases, previous ocular diseases, previous ocular surgeries, wearing of contact lenses, trauma and foreign body.
The statistical analysis was performed using the SPSSTM software. The statistical methods used were the chi-square test, univariate analysis of variance (ANOVA), the Wilcoxon signed ranks test and Spearman's rho.
RESULTS
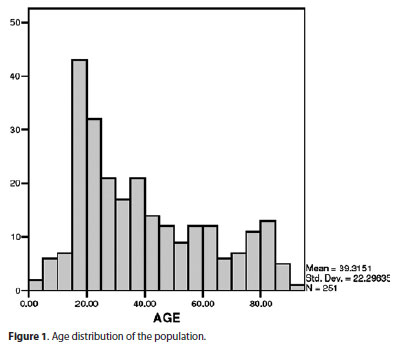
The review of the charts of patients admitted with the diagnosis of keratitis identified 276 patients (51% males and 48.9% females). The mean age was 39.29 ± 22.30 years, with a wide range between one month old and 92 years old (Figure 1).
The hospital length of stay ranged from 1 to 65 days (mean 5.69 ± 5.508). The discharge criteria were healed epithelial defect, decreased inflammation or infection signs and absence of anterior chamber reaction. Fortified antibiotics were continued after discharge in 72% of the cases.
The mean visual acuity at admission was 0.60 logMAR (n=272). The mean visual acuity at the first follow-up visit at the outpatient clinic was 0.42 logMAR (n=223). Comparison of visual acuity of the patients that had assessments both at admission and follow-up visit showed a statically significant improvement. (p=0.0001 Wilcoxon signed ranks test).
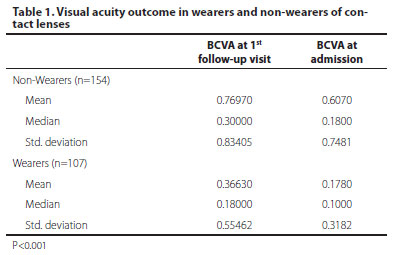
The use of contact lenses was noted in 110 patients (36.1%), their average age was 25.9 years-old (range 0-75 years-old) and 61.46% were females. The inpatient admission period was longer in non-contact lens wearers with a median of 5 days versus 4 days in contact lens wearers (p<0.003 Mann-Whitney test). The presence of anterior chamber reaction (fibrin, cells and hypopyon) was not significantly associated with contact lens wearing. The 7 day post-discharge visual acuity was better in wearers than in non-wearers (p<0.001) (Table 1).
Assessment of age as a prognostic factor showed that patients over 34 years old had a significantly longer hospital stay as well as a worse visual acuity at the 7-day post-discharge follow-up visit (p=0.001 Mann-Whitney test).
There were also 28 (9.2%) cases of keratitis associated with foreign bodies and 31 (11.2%) cases related to previous intraocular surgeries. This latter group had a worse clinical course than the former. The patients were older (mean age 68.9) and their hospital length of stay was longer (mean 8.7 days). The improvement of the mean visual acuity was significantly lower than in the overall population: 1.62 logMAR at admission to 1.47 logMAR at the first follow-up against 0.43 logMAR and 0.25 logMAR in the overall population (p<0.01 on the Mann-Whitney and Wilcoxon tests).
The size of the infiltrate at admission was 149 (48.9%) in grade 1 (up to 1 mm), 46 (15.1%) in grade 2 (from 1 to 2 mm), and 50 (16.4%) in category 3 (over 2 mm). In 19.6% of the cases records did not clearly defined the grade of the infiltrate. Patients with large infiltrates (grade 3) had a worse visual acuity both at presentation and at the 7-day follow-up visit compared with the other categories (p<0.0001Spearman's rho).
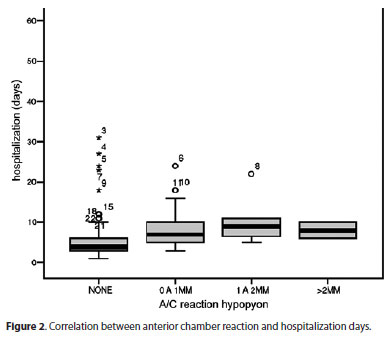
Anterior chamber reaction was frequently noted at admission: 41.6% of the cases had cells (>+1), 19.8%. had fibrin and 11.1% had hypopyon. The amount of cells and the measurement of hypopyon were related to a worse prognosis. There was a statiscally significantly relationship between length of hospitalization and visual acuity with positive inflammatory signs at admission. (p=0.001) (Figure 2).
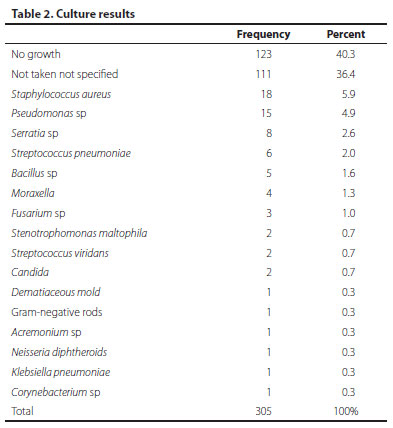
Cultures were obtained from 194 cases. In 111 (36.6%) cases antibiotic treatment was used prior to admission. After admission, patients were initially treated empirically and changes were made accordingly. The most frequent antibiotic regimen included combination of fortified antibiotics such as cefazolin (50 mg/mL) with gentamicin (13.6 mg/mL) (23%) or vancomycin (33 mg/mL) with ceftazidime (40 mg/mL) (29.2%).
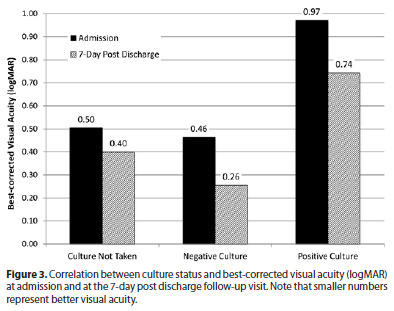
From the cultures taken (194 cases), only 36% (n=71) were positive. The microbiological profile of our population is shown in table 2. Patients with positive cultures had a significantly worse baseline visual acuity as compared with cases with negative cultures and with the group which cultures were not taken (p<0.0001)
The improvement of visual acuity at the 7-day post discharge follow-up visit was statistically significantly smaller in the positive-culture group as compared with the negative-culture group and with the no-culture group (p<0.0001) (Figure 3). The hospital length of stay of the positive-culture patients was longer: mean 7.37 days (p=0.001).
The rate of urgent surgical intervention was low: tarsorrhaphy in 3.7% (n=10), therapeutic penetrating keratoplasty (PK) in 2.3% (n=7), vitrectomy due to endophthalmitis in 1% (n=3) and evisceration in 1% (n=3).
The impact of previous ocular surgeries such as PK, extracapsular cataract extraction (ECCE) or combined PK + ECCE (n=31) was evaluated. The mean age of this group was higher as compared the non-previous surgery group (68.96 years ± 20.0 versus 39.29 years ± 22.3 years, respectively).Their mean visual acuity at admission and at the 7-post discharge follow-up visit were statistically significantly worse in the previous surgery group (1.62 logMAR and 1.47 logMAR respectively) than in the non-previous surgery group (0.43 logMAR and 0.25 logMAR respectively respectively). (p<0.01 Mann-Whitney and Wilcoxon signed ranks tests). The rate of positive cultures were higher in the previous surgery group (61%) as compared with patiens that have not undergone surgery. The rate of urgent surgical intervention was significantly higher in the previous surgery group (30%) as compared with the non-previous surgery group (8.7%) (p<0.01). The most common urgent surgical intervention in the previous surgery group was the need for urgent PK (14%) against 0.4% in the non-previous surgery group (p<0.01).
DISCUSSION
Microbial keratitis is an ophthalmological emergency that requires immediate treatment. Our study evalueted characteristics and outcomes of 276 consecutive patients admitted with a diagnosis of presumed keratitis. The early diagnosis and the intensive inpatient treatment may have resulted into the overall clinical and visual improvement seen in our population.
Daniell et al.(18) described different strategies for approaching patients diagnosed with presumed microbial keratitis. Patients with small peripheral lesions could be treated empirically with topical fluorquinolones, whereas the ones with central larger lesions should undergo scrapings for culture and topical quinolone associated with a cephalosporin should be started. In our department, taking cultures and the initial treatment were based on the clinical judgment of the attending ophthalmologist who examined the patient at the emergency ward.
Some authors(22) studied a model to determine the impact of minimal inhibitory concentration (MIC) on the clinical outcome. It included patients who received monotherapy with a fluoroquinolone who had no subsequent change in their treatment and whose ulcers healed without surgical intervention. He found significant linear associations between clinical outcome and MIC for Pseudomonas spp. (P=0.047), Staphylococcus aureus (P=0.04), and Enterobacteriaceae (P=0.045), but not for Streptococcus spp. (P=0.85) and coagulase-negative staphylococci (CNS) (P=0.88).
In the population we studied, 36.6% were already using some kind of topical treatment that failed. The treatment approach was the use of fortified topical antibiotics given every hour at the beginning, which included either cefazolin and gentamicin or vancomycin and ceftazidime. Treatment modifications were made according to culture results and clinical outcome on a case by case basis. Hospitalization assured treatment compliance until stabilization and may be related to the good visual outcome and low complication rate seen in our population.
The risk factors in our population are compatible with the ones described in the literature. Contact lens wearing was the major predisposing condition in our population (36%), comparable with the prevalence found in an Australian study (33.7%)(10) and in a Taiwanese study (44.3%)(2).
In our study, contact lens wearers had a significantly better final visual outcome. This fact may be due to their younger age and to early ophthalmological examination performed in this population.
Age and clinical presentation influenced the hospital length of stay. Patients older than 34 years stayed longer (mean of 6.88 days against 4.56 days of younger patients) and their final visual acuity was also significantly worse than those patients under 34 years old. Parmar et al., showed that the elderly tend to have more severe presentations of keratitis with a worse outcome, suggesting that this may be due to the lower immunocompetence of this age group(12). The high prevalence of patients aged 18 to 21 years in our study group may be due to the referrals from the military medical corps to our tertiary center. The recruits and soldiers can seek medical attention promptly, thus their clinical presentation is usually mild.
The best-corrected visual acuity (BCVA) measured at admission improved significantly compared with the one measured at the first follow-up visit, 1 week after discharge with a closed ulcer and no anterior chamber reaction. Other studies showed overall visual loss(2,4,7).
By analyzing the clinical characteristics at presentation we found that ulcers larger than 2 mm and with hypopyon greater than 1 mm were significantly related to worse visual acuity at admission and at the first follow-up visit. The hospital length of stay was longer in the presence of those findings. This underlines that seeking an ophthalmologist as soon as symptoms appear has a tremendous impact on the final visual outcome and on the public health expenses on hospitalization and antibiotic treatment. However, other authors(9) demonstrated in their study of an Australian population that the cost to treat was significantly associated only with clinical severity and type of pathogen, not with delay in presentation.
In our series, cultures were obtained in194 of the patients admitted (70.3%). The reasons for not obtaining cultures by scrapings included: uncooperative patients, ulcers that are peripheral and small and without anterior chamber reaction, keratitis may be treated empirically. The UK ofloxacin study suggested that the microbiological investigation of ulcers smaller than 2 mm is probably not worthwhile(24).
Another study from a Nepalese population by Feilmeir et al., demonstrated that microorganisms were grown from 40% of the corneal scrapings. Pure bacterial cultures were obtained from 39% of the positive scrapings and pure fungal cultures were obtained from 61%(25).
The most prevalent microorganism in our cultures was coagulase-positive Staphylococcus (25.3% of positive cultures), followed by Pseudomonas (21.1%). These results were compatible with the study of the Israeli microbiological profile of ocular infections also showed that coagulase-positive Staphylococcus was also the most prevalent agent in corneal isolates(23).
Patients with positive cultures (35%) had a longer hospital stay (mean of 7.37 days) and a worse visual prognosis.
Previous ocular surgery has been described as a predisposing factor for microbial keratitis(2,26). In our population, patients with previous ECCE, PK or combined surgery were older and had a significantly worse visual acuity either at admission or at the 7-day follow up visit. The rate of positive cultures was significantly higher in this group (61%), and Gram-positive bacteria were the most common etiologic agents isolated from the scrapings. Moreover, the need of secondary intervention such as urgent PK or evisceration was significantly higher in this subgroup. However, Green et al.(27) demonstrated in a longitudinal study that there is a trend towards decreased incidence of keratitis in patients with previous surgeries.
CONCLUSION
There are some limitations to our study. The data is based on retrospective charts analyzing only patients with keratitis that were addmited to the ward. The decision to admit the patient was based on clinical appearance, on previous treatment failure in the community and on the evaluation of patient's possible limitations to comply with the treatment, therefore some mild cases may not have included. The ones discharged at the emergency room were not included. There are some patients that missed the follow-up and were also excluded from the analysis. Adittional prospective controlled studies in this geographic area are needed to confirm our results.
Nevertheless, this present study has a large number of patients studied is able to demonstrate clinical trends such as microbial keratitis must be treated aggressively and promptly to achieve a good visual outcome. Furthermore, age, anterior chamber cells and hypopyon, positive cultures and previous surgery were risk factors related to lengthier hospitalization and a worse BCVA at the 7-day follow-up visit.
REFERENCES
1. Blanton CL, Rapuano CJ, Cohen EJ, Laibson PR. Initial treatment of microbial keratitis. CLAO J. 1996;22(2):136-40. Comment in: CLAO J. 1996;22(4):222.
2. Fong CF, Tseng CH, Hu FR, Wang IJ, Chen WL, Hou YC. Clinical characteristics of microbial keratitis in a university hospital in Taiwan. Am J Ophthalmol. 2004;137(2):329-36.
3. Jeng BH, Gritz DC, Kumar AB, Holsclaw DS, Porco TC, Smith SD, et al. Epidemiology of ulcerative keratitis in Northern California. Arch Ophthalmol [Internet]. 2010 [cited 2012 Jul 21];128(8):1022-8. Available from: http://archopht.jamanetwork.com/article.aspx?articleid=426096
4. al-Samarrai AR, Sunba MS. Bacterial corneal ulcers among Arabs in Kuwait. Ophthalmic Res. 1989;21(3):278-84.
5. Carmichael TR, Wolpert M, Koornhof HJ. Corneal ulceration at an urban African hospital. Br J Ophthalmol. 1985;69(12):920-6.
6. Cheung J, Slomovic AR. Microbial etiology and predisposing factors among patients hospitalized for corneal ulceration. Can J Ophthalmol. 1995;30(5):251-5.
7. Hagan M, Wright E, Newman M, Dolin P, Johnson G. Causes of suppurative keratitis in Ghana. Br J Ophthalmol [Internet]. 1995 [cited 2010 Jun 2];79(11):1024-8. Available from: http://bjo.bmj.com/content/79/11/1024.long
8. Katz NN, Wadud SA, Ayazuddin M. Corneal ulcer disease in Bangladesh. Ann Ophthalmol. 1983;15(9):834-6.
9. Keay L, Edwards K, Brian G, Stapleton F. Surveillance of contact lens related microbial keratitis in Australia and New Zealand: multi-source case-capture and cost-effectiveness. Ophthalmic Epidemiol. 2007;14(6):343-50.
10. Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113(1):109-16. Comment in: Ophthalmology. 2006;113(11):2115-6; author reply 2116.
11. Kunimoto DY, Sharma S, Garg P, Gopinathan U, Miller D, Rao GN. Corneal ulceration in the elderly in Hyderabad, south India. Br J Ophthalmol [Internet]. 2000[cited 2011 Mar 19];84(1):54-9. Available from: http://bjo.bmj.com/content/84/1/54.long
12. Parmar P, Salman A, Kalavathy CM, Kaliamurthy J, Thomas PA, Jesudasan CA. Microbial keratitis at extremes of age. Cornea. 2006;25(2):153-8.
13. Upadhyay MP, Karmacharya PC, Koirala S, Tuladhar NR, Bryan LE, Smolin G, et al. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991;111(1):92-9.
14. van der Meulen IJ, van Rooij J, Nieuwendaal CP, Van Cleijnenbreugel H, Geerards AJ, Remeijer L. Age-related risk factors, culture outcomes, and prognosis in patients admitted with infectious keratitis to two Dutch tertiary referral centers. Cornea. 2008;27(5):539-44.
15. Varaprasathan G, Miller K, Lietman T, Whitcher JP, Cevallos V, Okumoto M, et al. Trends in the etiology of infectious corneal ulcers at the F. I. Proctor Foundation. Cornea. 2004;23(4):360-4.
16. Wong T, Ormonde S, Gamble G, McGhee CN. Severe infective keratitis leading to hospital admission in New Zealand. Br J Ophthalmol [Internet]. 2003[cited 2012 Dec 21]; 87(9):1103-8. Available from: http://bjo.bmj.com/content/87/9/1103.long
17. Bharathi MJ, Ramakrishnan R, Meenakshi R, Mittal S, Shivakumar C, Srinivasan M. Microbiological diagnosis of infective keratitis: comparative evaluation of direct microscopy and culture results. Br J Ophthalmol [Internet]. 2006[cited 2011 Feb 12]; 90(10):1271-6. Available from: http://bjo.bmj.com/content/90/10/1271.long
18. Daniell M, Mills R, Morlet N. Microbial keratitis: what's the preferred initial therapy? Br J Ophthalmol. 2003;87(9):1167. Comment in: Br J Ophthalmol. 2003; 87(9):1167-9. Br J Opthalmol. 2003;87(9):1172-4. Br J Ophthalmol. 2003;87(9):1169-72.
19. Jones DB. Decision-making in the management of microbial keratitis. Ophthalmology. 1981;88(8):814-20.
20. Pharmakakis NM, Andrikopoulos GK, Papadopoulos GE, Petropoulos IK, Kolonitsiou FI, Koliopoulos JX. Does identification of the causal organism of corneal ulcers influence the outcome? Eur J Ophthalmol. 2003;13(1):11-7.
21. Rao NA. A laboratory approach to rapid diagnosis of ocular infections and prospects for the future. Am J Ophthalmol. 1989;107(3):283-91.
22. Kaye S, Tuft S, Neal T, Tole D, Leeming J, Figueiredo F, et al. Bacterial susceptibility to topical antimicrobials and clinical outcome in bacterial keratitis. Invest Ophthalmol Vis Sci [Internet]. 2010[cited 2012 Oct 21];51(1):362-8. Comment in: Invest Ophthalmol Vis Sci. 2010;51(12):6902-3; author reply 6903. Available from: http://www.iovs.org/content/51/1/362.long
23. Mezer E, Gelfand YA, Lotan R, Tamir A, Miller B. Bacteriological profile of ophthalmic infections in an Israeli hospital. Eur J Ophthalmol. 1999;9(2):120-4.
24. Ofloxacin monotherapy for the primary treatment of microbial keratitis: a double-masked, randomized, controlled trial with conventional dual therapy. The Ofloxacin Study Group. Ophthalmology. 1997;104(11):1902-9.
25. Feilmeier MR, Sivaraman KR, Oliva M, Tabin GC, Gurung R. Etiologic diagnosis of corneal ulceration at a tertiary eye center in Kathmandu, Nepal. Cornea. 2010;29(12):1380-5.
26. Llovet F, de Rojas V, Interlandi E, Martin C, Cobo-Soriano R, Ortega-Usobiaga J, et al. Infectious keratitis in 204 586 LASIK procedures. Ophthalmology. 2010;117(2):232-8 e1-4. Comment in: Ophthalmology. 2011;118(2):425; author reply 425.e1
27. Green M, Apel A, Stapleton F. A longitudinal study of trends in keratitis in Australia. Cornea. 2008;27(1):33-9.
 Correspondence address:
Correspondence address:
Fabio Lavinsky
Rua Quintino Bocaiúva, 673 - 3º andar
Porto Alegre (RS) - 90440-051 - Brazil
E-mail: [email protected]
Submitted for publication: May 21, 2012
Accepted for publication: May 29, 2013
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: F.Lavinsky, None; N.Avni-Zauberman, None; I.S.Barequet, None.
Study carried out at Goldschleger Eye Institute, Sheba Medical Center, Tel Aviv University Sackler, Faculty of Medicine, Tel Hashomer, Israel.