

Lucas Barasnevicius Quagliato1; Kleyton Barella1; José Maria Abreu Neto1; Elizabeth Maria Aparecida Barasnevicius Quagliato2
DOI: 10.1590/S0004-27492013000100014
ABSTRACT
This paper describes a topiramate induced acute bilateral angle-closure glaucoma. This rare adverse effect is an idiosyncratic reaction characterized by uveal effusion and lens forward displacement, leading to increased intraocular pressure and vision loss. We describe a 55 year-old white woman with migraine, spasmodic torticollis and essential tremor, who developed bilateral acute angle-closure glaucoma, one week after starting topiramate 25 mg/day. She was seen at the Ophthalmology Emergency Department of the Fundação João Penido Burnier (Campinas, SP, Brazil) with a 4 hours history of blurry vision, ocular pain and bright flashes vision. Slit lamp examination revealed moderate conjunctival injection and corneal edema, and shallow anterior chambers. Intraocular pressure was 48 mmHg in both eyes. Fundoscopic examination findings were normal. She was treated with timolol, brimonidine, dorzolamide, pilocarpine, prednisone acetate eye drops and acetazolamide. One hour after those measures, as the intraocular pressure was 30 mmHg, she received a manitol intravenous injection and the intraocular pressure normalized. After 24 hours an iridotomy with Yag laser was performed. Topiramate was discontinued and she was totally recovered after one week.
Keywords: Glaucoma, angle closure; Glaucoma, angle closure; Anticonvulsants; Intraocular pressure; Uveal diseases; Case report
RESUMO
Relato de um caso de glaucoma bilateral de ângulo fechado induzido pelo topiramato. Este raro efeito colateral é uma idiosincrasia causada por efusão uveal e deslocamento do cristalino para frente, causando aumento da pressão intraocular e perda visual. Descrevemos o caso de uma paciente de 55 anos com migrânea, torcicolo espasmódico e tremor essencial, que desenvolveu glaucoma bilateral de ângulo fechado uma semana após iniciar o uso de topiramato, 25 mg/dia. A paciente foi atendida no setor de Emergências Oftalmológicas da Fundação Penido Burnier (Campinas, SP, Brasil), com história de 4 horas de embaçamento visual, dor ocular e visão de flashes brilhantes. O exame com lâmpada de fenda revelou injeção conjuntival moderada, edema corneano e câmara anterior rasa em ambos os olhos. A pressão intraocular era de 48 mmHg bilateralmente e a fundoscopia era normal. Foi tratada com colírios de timolol, brimonidina, dorzolamida, pilocarpina e acetato de prednisona e acetazolamida via oral. Uma hora após essas medidas, a pressão intraocular era 30 mmHg, e a paciente recebeu uma injeção intravenosa de manitol, ocorrendo normalização da pressão intraocular após essa medida. Após 24 horas foi realizada iridectomia com Yag laser. O topiramato foi interrompido e ela se recuperou totalmente após uma semana.
Descritores: Glaucoma, ângulo-fechado; Glaucoma, ângulo-fechado; Anticonvulsivantes; Pressão intraocular; Doenças uveais; Relato de caso
CASE REPORT RELATO DE CASO
Topiramate-associated acute, bilateral, angle-closure glaucoma: case report
Glaucoma agudo de ângulo fechado, bilateral, desencadeado pelo topiramato: relato de caso
Lucas Barasnevicius QuagliatoI; Kleyton BarellaI; José Maria Abreu NetoI; Elizabeth Maria Aparecida Barasnevicius QuagliatoII
IPhysician, Fundação João Penido Burnier, Campinas (SP) - Brazil
IIPhysician, Neurology Departament, Universidade Estadual de Campinas, Campinas (SP) - Brazil
ABSTRACT
This paper describes a topiramate induced acute bilateral angle-closure glaucoma. This rare adverse effect is an idiosyncratic reaction characterized by uveal effusion and lens forward displacement, leading to increased intraocular pressure and vision loss. We describe a 55 year-old white woman with migraine, spasmodic torticollis and essential tremor, who developed bilateral acute angle-closure glaucoma, one week after starting topiramate 25 mg/day. She was seen at the Ophthalmology Emergency Department of the Fundação João Penido Burnier (Campinas, SP, Brazil) with a 4 hours history of blurry vision, ocular pain and bright flashes vision. Slit lamp examination revealed moderate conjunctival injection and corneal edema, and shallow anterior chambers. Intraocular pressure was 48 mmHg in both eyes. Fundoscopic examination findings were normal. She was treated with timolol, brimonidine, dorzolamide, pilocarpine, prednisone acetate eye drops and acetazolamide. One hour after those measures, as the intraocular pressure was 30 mmHg, she received a manitol intravenous injection and the intraocular pressure normalized. After 24 hours an iridotomy with Yag laser was performed. Topiramate was discontinued and she was totally recovered after one week.
Keywords: Glaucoma, angle closure/diagnosis; Glaucoma, angle closure/chemically induced; Anticonvulsants/adverse effects; Intraocular pressure; Uveal diseases/chemically induced; Case report
RESUMO
Relato de um caso de glaucoma bilateral de ângulo fechado induzido pelo topiramato. Este raro efeito colateral é uma idiosincrasia causada por efusão uveal e deslocamento do cristalino para frente, causando aumento da pressão intraocular e perda visual. Descrevemos o caso de uma paciente de 55 anos com migrânea, torcicolo espasmódico e tremor essencial, que desenvolveu glaucoma bilateral de ângulo fechado uma semana após iniciar o uso de topiramato, 25 mg/dia. A paciente foi atendida no setor de Emergências Oftalmológicas da Fundação Penido Burnier (Campinas, SP, Brasil), com história de 4 horas de embaçamento visual, dor ocular e visão de flashes brilhantes. O exame com lâmpada de fenda revelou injeção conjuntival moderada, edema corneano e câmara anterior rasa em ambos os olhos. A pressão intraocular era de 48 mmHg bilateralmente e a fundoscopia era normal. Foi tratada com colírios de timolol, brimonidina, dorzolamida, pilocarpina e acetato de prednisona e acetazolamida via oral. Uma hora após essas medidas, a pressão intraocular era 30 mmHg, e a paciente recebeu uma injeção intravenosa de manitol, ocorrendo normalização da pressão intraocular após essa medida. Após 24 horas foi realizada iridectomia com Yag laser. O topiramato foi interrompido e ela se recuperou totalmente após uma semana.
Descritores: Glaucoma, ângulo-fechado/diagnóstico; Glaucoma, ângulo-fechado/quimicamente induzido; Anticonvulsivantes/efeitos adversos; Pressão intraocular; Doenças uveais/induzidas quimicamente; Relato de caso
INTRODUTION
Many systemic action drugs can cause acute glaucoma, but simultaneous bilateral acute angle-closure glaucoma (BAACG) is rare. Topiramate is a sulpha-derivative monosaccharide that is used for treating epilepsy (1996) and migraine (2004), but other indications includes infantile spasms, psychiatric disorders, neuropathic pain, weight reduction, tobacco dependence, essential tremor, and post-herpetic neuralgia(1). Topiramate blocks voltage-gated sodium channels, hyperpolarizes potassium currents, enhances postsynaptic gamma-aminobutyric acid receptor activity, suppresses the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA)/kainate receptor, reduces glutamate excitatory activity and inhibits some carbonic anhydrase isoenzimes(2). This drug is rapidly absorbed after oral intake and is excreted in urine with a half-life of almost 24 hours(1). Adverse ophthalmologic events topiramate-related are rare, and they generally occur during the first treatment month(3). Besides BAACG, other ocular side effects related to topiramate are massive choroidal effusion, ocular inflammatory reactions, unilateral hemianopsia, neuro-ophthalmologic complications and irreversible maculopathy(1,2). The first description of BAACG related to topiramate was published in 2001(4) and a systematic 2012 review described 75 relevant studies concerning topiramate effects on vision. Sixty-five small observational studies described the ophthalmologic side effects in 84 patients(1).
The putative mechanism of acute glaucoma and myopia are related to uveal effusion, that leads to zonula relaxation, causing anterior displacement of the lens-iris diaphragm. As consequence, occurs miopization and reduction of anterior camera deepness. Choroidal detachment is frequently associated. Some authors suggest that acute myopia is due to the anhydrase carbonic inhibition, lens edema and accommodation spasm(5,6).
Topiramate is the leading cause of BAACG in patients under the forties and is a potentially blinding disease. The clinical picture is reversible if diagnosed and treated precociously and the drug is immediately discontinued(4,7-10). The incidence of permanent vision loss in topiramate-associated BAACG is 8.1%(6).
CASE PRESENTATION
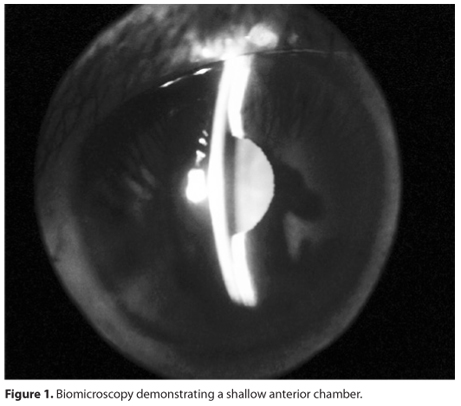
A 55-year-old white woman presented with BAACG, one week after starting topiramate, 25 mg/day, indicated to migraine prevention. She also had spasmodic torticollis and essential tremor. She presented a 4 hours history of sudden blurring of vision, feeling of pressure over the eyes and visual flashes perception. On the initial examination, the best corrected visual acuities were 0.8 and 0.5 on the right eye (OD) and left eye (OS) respectively, with -2.00 in both eyes (BE). The biomicroscopy showed shallow anterior chambers, moderate corneal edema and moderate conjunctival injection (Figure 1). The IOPs were 48 mmHg OU. The gonioscopy with and without compression revealed a 360º bilateral closed angle and a superior 180º synechiae indentation. Fundoscopic examination was normal. After the diagnosis of BAACG topiramate was immediately discontinued. She was treated with topical 0.5% timolol maleate, 0.15% brimonidine tartrate, 2% dorzolamide hydrochloride, 1% prednisolone acetate, 1% pilocarpine and 500 mg acetazolamide orally. After one hour, the IOP was 30 mmHg OU and intravenous 20% mannitol (50 g) was administered. After two hours, the IOP was 18 mmHg in both eyes, the symptoms improved and she was discharged home with prednisolone acetate, pilocarpine, brimonidine tartrate and timolol maleate. By the next morning the patient continued asymptomatic and the visual acuities were 0.8 on the OD and 0.66 on the OS. Biomicroscopy showed shallow anterior chambers and there was no corneal edema. Gonioscopy revealed sinechiae and a superior 180º closed angle and IOP was 16 mmHg. An Yag laser iridotomy was performed OU because there was risk of total angle closure. She was sent home with prednisolone acetate, brimonidine tartrate and timolol maleate. After 48 hours, she returned asymptomatic, and the best corrected visual acuities were 0.8 OU, without myopic shift. The corneal edema disappeared and there was a lens intumescence. Gonioscopy revealed synechiae on 180º inferior OU. Fundoscopy showed a 0.6 X 0.6 excavation bilaterally. Visual fields were full OU. The pachymetry results were 473 µm on the RE and 475 µm on the LE. The optical coherence tomography showed a 0.6 x 0.7 excavation and there was no optical nerve fiber loss OU. The IOP was 12 mmHg in BE, and the iridotomy was patent. The patient was discharged with a brimonidine tartrate and timolol maleate prescription. One month after, she had no symptoms, the visual acuity returned to normal, and the pattern shift visual evoked potentials results were normal.
DISCUSSION
We report the third Brazilian case of BAACG related to topiramate, with a favorable outcome(2,10). Our patient symptoms began one week after initiating topiramate, accordingly to other previous published cases, which visual symptoms initiated during the two initial treatment weeks(6,8). Topiramate dosis related to BAACG was up to 50 mg in almost 50% of the yet described cases, as occurred with this patient(6).
Ophthalmologic evaluation showed increased IOP, shallow anterior chambers, moderate corneal edema and moderate conjunctival injection, signs frequently described in the literature(1,6). This clinical picture was acute and bilateral, as commonly seen in other topiramate-induced glaucoma reports, and can occur at any age(1,2,10). This patient initial treatment was a conventional one for glaucoma, but there was no complete IOP normalization until mannitol intravenous administration. On the next day, the biomicroscopy showed sinechiae and she was treated with a bilateral Yag laser iridotomy because those sinechiae could be present previously and then predispose to a total angle closure recurrence. Laser or surgical peripheral iridotomy was performed on 38% of the BAACG described in the literature, but generally this procedure is not indicated, because as the acute glaucoma is caused by uveal effusion without pupillary block, a peripheral iridotomy can aggravate the glaucoma, putting forward iris and lens(6). An increased IOP, if maintained for long periods, can damage severely the optic nerve and is of paramount importance that the glaucoma etiology could be removed. This case illustrates the importance of recognizing this entity in a non-ophthalmic setting and that intravenous mannitol may be useful in the treatment of the condition when it is not responsive to conventional treatment. Thus, it was possible a complete visual symptoms normalization, leading to recovery of the deepness of the anterior chamber and normalization of IOP.
REFERENCES
1. Abtahi MA, Abtahi SH, Fazei F, Roomizadeh P, Etemadifar M, Jenab K, et al. Topiramate and the vision: a systematic review. Clin Ophthalmol. 2012;6:117-31.
2. Brandão MN, Fernandes IC, Barradas FF, Machado JF, Oliveira MT. Miopia aguda e glaucoma de ângulo fechado associados ao uso de topiramato em paciente jovem: relato de caso. Arq Bras Oftalmol. 2009;72(1):103-5.
3. Cereza G, Pedrós C, Garcia N, Laporte JR. Topiramate in non-approved indications and acute myopia or angle closure glaucoma. Br J Clin Pharmacol. 2005;60(5):578-9.
4. Banta JT, Hoffman K, Budenz DL, Ceballos E, Greenfield DS. Presumed topiramate-induced bilateral acute angle-closure glaucoma. Am J Ophthalmol. 2001;132(1):112-4.
5. Lee GC, Tam CP, Danesh-Meyer HV, Myers JS, Katz LJ. Bilateral angle closure glaucoma induced by sulphonamide-derived medications. Clin Experiment Ophthalmol. 2007; 35(1):55-8.
6. Fraunfelder FW, Fraunfelder FT, Keates EU. Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology. 2004;111(1):109-11.
7. Medeiros FA, Zhang XY, Bernd AS, Weinreb RN. Angle-closure glaucoma associated with ciliary body detachment in patients using topiramate. Arch Ophthalmol. 2003; 121(2):282-5.
8. Sankar PS, Pasquale LR, Grosskreutz CL. Uveal effusion and secondary angle-closure glaucoma associated with topiramate use. Arch Ophthalmol. 2001;119(8):1210-1. Comment in Arch Ophthalmol. 2002;120(8):1108.
9. Lin J, Fosnot J, Edmond J. Bilateral angle closure glaucoma in a child receiving oral topiramate. J AAPOS. 2003;7(1):66-8.
10. Stangler F, Prietsch RF, Fortes Filho JB. Glaucoma agudo bilateral em paciente jovem secundário ao uso de topiramato: relato de caso. Arq Bras Oftalmol. 2007;70(1):133-6.
 Corresponding author:
Corresponding author:
Lucas Barasnevicius Quagliato
Rua Alfredo Calil, 187
Campinas (SP) - 13101-507 - Brazil
E-mail - [email protected]
Submitted for publication: January 16, 2013
Accepted for publication: February 4, 2013
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: L.B.Quagliato, None; K.Barella, None; J.M.Abreu Neto, None; E.M.A.B.Quagliato, None.
Study carried out at Fundação João Penido Burnier, Campinas (SP) - Brazil