

Ricardo Yuji Abe1; Roberto Damian Pacheco Pinto1; João Felipe Leite Bonfitto2; Rodrigo Pessoa Cavalcanti Lira3; Carlos Eduardo Leite Arieta3
DOI: 10.1590/S0004-27492012000600013
ABSTRACT
A 33-year-old woman complained of unilateral eyelid edema and blurred vision. Initial ophthalmic examination disclosed anterior chamber reaction with keratic precipitates on the cornea, without posterior abnormalities. Anterior uveitis was treated. Despite that, patient showed rapidly progressive unilateral vision loss with optic nerve swelling. Systemic workup was inconclusive, as well as cranial magnetic resonance imaging and cerebrospinal fluid examination. Based on the hypothesis of optic neuritis, intravenous methylprednisolone pulse was performed with no success. During the following days, the patient presented pericardial effusion and cardiac tamponade, progressing to death. Necropsy was performed and diagnosis of extranodal natural killers/T-cell lymphoma, nasal type with ocular involvement was confirmed by immunohistochemistry.
Keywords: Eye neoplasms; Lymphoma T-Cell; Nose neoplasms; Vision disorders; Uveitis; Optic neuritis; Killer cells; natural; Immunohistochemistry; Humans; Male; Adult; Case report
RESUMO
Paciente feminina de 33 anos apresentando edema palpebral unilateral com baixa acuidade visual. Ao exame oftalmológico inicial apresentava reação de câmara anterior com precipitados ceráticos corneano, sem alterações no fundo de olho. Foi instituído tratamento para uveíte anterior e solicitado exames sistêmicos para investigação. Após alguns dias, paciente apresentou piora da acuidade visual, com edema de disco óptico unilateral. Sendo então solicitada ressonância nuclear magnética de crânio. Ambos exames de imagem e investigação sistêmica foram inconclusivos. Em vista da piora progressiva da acuidade visual e sob hipótese diagnóstica de neurite óptica, foi iniciado pulso intravenoso de metilprednisolona por 3 dias sem sucesso. A paciente apresentou dos dias seguintes, derrame pericárdico e tamponamento cardíaco, evoluindo para óbito. A necrópsia confirmou o diagnóstico de linfoma extranodal de células T e natural killers do tipo nasal com envolvimento ocular, através de imunoistoquímica.
Descritores: Neoplasias oculares; Linfoma de células T; Neoplasias nasaisl; Transtornos da visãol; Uveites; Neurite óptica; Células matadoras naturaisl; Imunoistoquímica; Humanos; Feminino; Adulto; Relato de caso
CASE REPORT RELATO DE CASO
Ocular masquerade syndrome associated with extranodal nasal natural killer/T-cell lymphoma: case report
Síndrome ocular mascarada associada ao linfoma extranodal nasal natural killer/células T: relato de caso
Ricardo Yuji AbeI; Roberto Damian Pacheco PintoI; João Felipe Leite BonfittoII; Rodrigo Pessoa Cavalcanti LiraIII; Carlos Eduardo Leite ArietaIII
IPhysician, Departamento de Oftalmologia, Hospital de Clínicas, Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
IIPhysician, Departamento de Patologia Clínica, Hospital de Clínicas, Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
IIIProfessor, Departamento de Oftalmologia, Hospital de Clínicas, Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil.
ABSTRACT
A 33-year-old woman complained of unilateral eyelid edema and blurred vision. Initial ophthalmic examination disclosed anterior chamber reaction with keratic precipitates on the cornea, without posterior abnormalities. Anterior uveitis was treated. Despite that, patient showed rapidly progressive unilateral vision loss with optic nerve swelling. Systemic workup was inconclusive, as well as cranial magnetic resonance imaging and cerebrospinal fluid examination. Based on the hypothesis of optic neuritis, intravenous methylprednisolone pulse was performed with no success. During the following days, the patient presented pericardial effusion and cardiac tamponade, progressing to death. Necropsy was performed and diagnosis of extranodal natural killers/T-cell lymphoma, nasal type with ocular involvement was confirmed by immunohistochemistry.
Keywords: Eye neoplasms; Lymphoma T-Cell; Nose neoplasms/complications; Vision disorders/etiology; Uveitis; Optic neuritis; Killer cells, natural/pathology; Immunohistochemistry; Humans; Male; Adult; Case report
RESUMO
Paciente feminina de 33 anos apresentando edema palpebral unilateral com baixa acuidade visual. Ao exame oftalmológico inicial apresentava reação de câmara anterior com precipitados ceráticos corneano, sem alterações no fundo de olho. Foi instituído tratamento para uveíte anterior e solicitado exames sistêmicos para investigação. Após alguns dias, paciente apresentou piora da acuidade visual, com edema de disco óptico unilateral. Sendo então solicitada ressonância nuclear magnética de crânio. Ambos exames de imagem e investigação sistêmica foram inconclusivos. Em vista da piora progressiva da acuidade visual e sob hipótese diagnóstica de neurite óptica, foi iniciado pulso intravenoso de metilprednisolona por 3 dias sem sucesso. A paciente apresentou dos dias seguintes, derrame pericárdico e tamponamento cardíaco, evoluindo para óbito. A necrópsia confirmou o diagnóstico de linfoma extranodal de células T e natural killers do tipo nasal com envolvimento ocular, através de imunoistoquímica.
Descritores: Neoplasias oculares; Linfoma de células T; Neoplasias nasais/complicações; Transtornos da visão/etiologia; Uveites; Neurite óptica; Células matadoras naturais/patologia; Imunoistoquímica; Humanos; Feminino; Adulto; Relato de caso
INTRODUCTION
Ocular masquerade syndrome (OMS) is a group of diseases that occurs with ocular inflammation and is often misdiagnosed as chronic uveitis(1,2). Non-Hodgkin lymphoma (NHL) is a malignant neoplasm derived from a clonal proliferation of B or T/NK lymphocytes. It is a heterogeneous group of different subtypes that can arise both in lymph nodes and in extranodal tissues(3).
Ocular involvement by NHL is a rare condition, constituting less than 1% of all lymphomas(3,4). Metastatic NHL lesions presenting as ocular inflammation have been reported as the initial presenting feature(5). Under the World Health Organization (WHO) classification, extranodal nasal natural killer/T-cell lymphoma (NKTL) is a form of lymphoma derived from natural killer (NK) cells and/or cytotoxic T-lymphocytes that typically involves the nasal cavity and paranasal sinuses(6). It is a common disease among Oriental, Native American, and Hispanic patients and is associated with the Epstein-Barr virus (EBV)(7). Furthermore, lymphomas expressing NK-cell markers are known to have a highly aggressive behavior and a poorer prognosis than B-cell lymphoma or T-cell lymphoma(8).
We present the clinical, morphologic, immunohistochemical and molecular features of a NKTL case report with ocular involvement.
CASE REPORT
A 33-year-old white woman complained of blurred vision and dimness of vision in the right eye, over a period of two months. She also complained about bilateral eyelid swelling, pain and photofobia in the right eye (OD). She was referred from another service, where she was treated for viral conjunctivitis. Her past ocular and systemic histories were unremarkable. Physical examination of the face revealed bilateral symmetric palpebral edema and minimal erythema on the right upper eyelid with no exophthalmos. Snellen's testing revealed best-corrected acuity of 20/100 in OD and 20/40 in the left eye (OS). Slit lamp biomicroscopy of OD showed mild ciliary injection with inferior mutton-fat keratic precipitates on the cornea, anterior chamber reaction (ACR) with 3+ cells and no flare. The anterior segment evaluation of OS was normal. Ocular motility was normal in both eyes. The intraocular pressure was 14 mmHg in OD and 15 mmHg in OS. Dilated fundus examination was performed and no abnormalities were found.
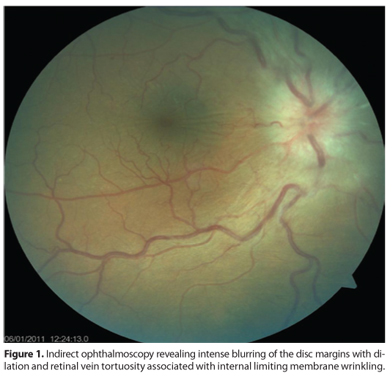
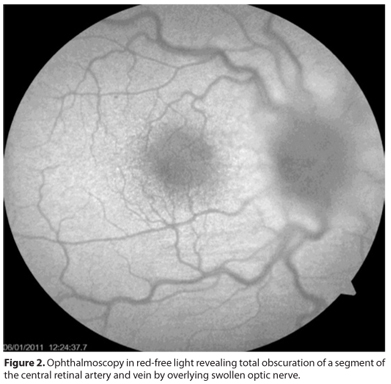
Systemic workup included: complete blood counting with differential classification, rheumatoid factor, antinuclear antibody, sedimentation rate, human immunodeficiency virus test, venereal disease research laboratory test, anticardiolipin antibody, chest and sacroiliac radiographies and Toxoplasma gondii and cytomegalovirus serologies. As anterior uveitis was diagnosed, the patient began treatment using 1% prednisolone eye drop 4 times a day and 1% atropine sulfate, b.i.d. , while we waited for the exam results. One week later, laboratory investigation failed to find a systemic disease and the patient got worse, with visual acuity of counting fingers at 1 meter in OD. The ACR of OD revealed 1+ cell, and fundus examination revealed diffuse optic disc swelling with no hemorrhages or abnormal vasculature, with no macular abnormalities (Figures 1 and 2). Cranial magnetic resonance imaging was performed and a sample of the cerebrospinal fluid was obtained. Both exams revealed no abnormalities, except from thickening of the right sphenoid sinus.
After two days, the patient returned with severe vision loss on OD (no light perception) and 20/40 in OS, with asymmetric palpebral edema, worse in the right upper eyelid. The ACR of OD was absent. Based on the hypothesis of optic neuritis, patient underwent intravenous pulse therapy of methylprednisolone (250 mg 6/6 hrs for 3 days) and, despite treatment, she remained with the same visual acuity. In the following two days, her systemic condition progressively deteriorated. She presented dyspnea and dry cough in the infirmary. Echocardiogram revealed moderate pericardial effusion and, during pericardiocentesis, the patient evolved to a cardiopulmonary arrest secondary to cardiac tamponade and died. The necropsy revealed a cardiac tamponade secondary to massive myocardial infiltration by an extranodal natural killer/T cell lymphoma, nasal type. Other organs infiltrated by the cancer were: skin, uterus, right optic nerve and adjacent soft tissues, small bowel and spleen.
DISCUSSION
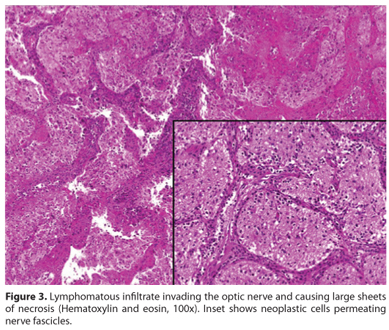
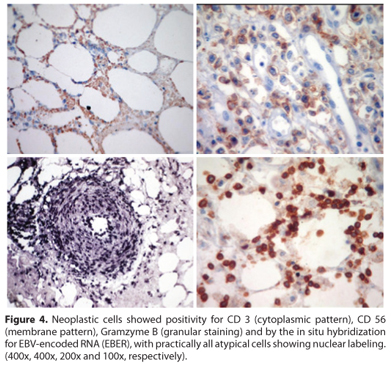
NKTL is a predominantly extranodal lymphoma characterized by vascular damage and destruction, prominent necrosis, cytotoxic phenotype and association with Epstein-Barr virus (EBV)(6). It occurs more often in male adults. The very strong association with EBV suggests a probable pathogenic role of the virus, and the disease can occur in the setting of immunosuppression. The upper aerodigestive tract is most commonly involved, with the nasal cavity being the prototypic site of involvement. In our case, the disease was seen inside the orbit, with the lymphomatous infiltrate permeating the right eye extraocular soft tissues and sclera and invading the optic nerve, causing large sheets of necrosis (Figure 3). Extranasal sites were also present and included the skin, lungs, gastrointestinal tract, uterus, spleen and the heart. The marked involvement of the latter was assumed as the immediate cause of the patient death. Microscopic evaluation revealed the atypical small and medium-sized neoplastic cells with an angiocentric and angiodestructive growth pattern. By immunohistochemistry, neoplastic cells showed expressions of CD 3 (a T-cell marker), CD 56 (a neural cell-adhesion molecule) and cytotoxic molecules (gramzyme B), a typical immunophenotype for this entity. There was positivity for CD 30 (a member of the tumor necrosis factor superfamily), as it is described in occasional cases. Finally, the lack of expression of ALK 1 and B-cell markers, and the positive result by the in situ hybridization for EBV encoded RNA (EBER) allowed us to confirm the diagnosis of disseminated NKTL (Figure 4)(6).
Some authors(9,10) did report a case of histologically confirmed nasal NKTL with intraocular involvement, as well as Yoo et al. ,(11). In a large series of 24 cases with primary nasal and paranasal sinus NKTL, six patients suffered from vision threatening complications of uveitis/vitritis and orbital involvement, including one with rhegmatogenous retinal detachment and one with macular hole(12). Therefore, ocular complications were relatively high (25%) and required ophthalmic treatment. Our patient presented with ocular prior to systemic manifestations, with advanced systemic disease. Therefore, baseline and regular ophthalmic assessments are necessary for all nasal and paranasal sinus lymphomas, in particular, NKTL.
REFERENCES
1. Nussenblatt RB, Whitcup SM. Uveitis: fundamentals and clinical practice. 3rd ed. St. Louis, MO: CV Mosby; 2004. p. 409-19.
2. Theodore FH. Conjunctival carcinoma masquerading as chronic conjunctivitis. Eye Ear Nose Throat Mon. 1967;46(11):1419-20.
3. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. World classification of tumours of haematopoietic and lymphoid tissues. 5th ed. Lyon: IARC Press; 2008.
4. Coupland SE, Damato B. Lymphomas involving the eye and the ocular adnexa. Curr Opin Ophthalmol. 2006;17(6):523-31.
5. Sjo¨ LD. Ophthalmic lymphoma: epidemiology and pathogenesis. Acta Ophthalmologica. 2009;87(Thesis 1):1-20.
6. Fredrick DR, Char DH, Ljung BM, Brinton DA. Solitary intraocular lymphoma as an initial presentation of widespread disease. Arch Ophthalmol. 1989;107(3):395-7.
7. Chan JKC, Jaffe ES, Ralfkiaer E. Extranodal NK/Tcell lymphoma, nasal type. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. World classification of tumours of haematopoietic and lymphoid tissues. 5th ed. Lyon: IARC Press; 2008. p.204-7.
8. Kwong YL, Chan AC, Liang RH. Natural Killer cell lymphoma/leukaemia: pathology and treatment. Hematol Oncol. 1997;15(2):71-9.
9. Jaffe ES, Chan JK, Su IJ, Frizzera G, Mori S, Feller AC, Ho FC. Report of the Workshop on Nasal and Related Extranodal Angiocentric T/ Natural Killer cell lymphomas: definitions, differential diagnosis and epidemiology. Am J Surg Pathol. 1996;20(1):103-11.
10. Cimino L, Chan CC, Shen D, Masini L, Ilariucci F, Masetti M, Asioli S, et al. Ocular involvement in nasal natural kille T-cell lymphoma.Int Ophthalmol. 2009;29(4):275-9.
11. Lee EJ, Kim TW, Heo JW, Yu HG, Chung H. Natural killer/T-cell lymphoma of nasal type with intraocular involvement: case report. .Eur J Ophthalmol. 2010;20(1):215-7.
12. Yoo JH, Kim SY, Jung KB, Lee JJ, Lee SJ. Intraocular involvement of a nasal natural killer T-cell lymphoma: a case report.Korean J Ophthalmol. 2012;26(1):54-7.
13. Hon C, Kwok AK, Shek TW, Chim JC, Au WY. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol. 2002;134(3):406-10.
 Correspondence address:
Correspondence address:
Ricardo Yuji Abe
Rua Castro Alves, 507/221
São Paulo (SP) - 01532-001 - Brazil
E-mail: [email protected]
Submitted for publication: August 9, 2012
Accepted for publication: October 9, 2012
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: R.Y.Abe, None; R.D.P.Pinto, None; J.F.L.Bonfitto, None; R.P.C.Lira, None; C.E.L.Arieta, None.
Study carried out at Universidade Estadual de Campinas - Unicamp.
Project Number: CAAE - 02935612.3.0000.5404