

Wilson Takashi Hida1; Antonio Francisco Motta2; Celso Takashi Nakano2; Patrick F. Tzelikis1
DOI: 10.1590/S0004-27492012000600012
ABSTRACT
A 51-year-old woman with age-related cataract had an uneventful phacoemulsification and a Tecnis ZM900 multifocal intraocular lens (IOL) implantation in both eyes. During IOL implantation in the left eye, the optic was unintentionally reversed in the bag and left that way. The refraction surprise was not significant and six months postoperatively the corrected distance visual acuity in both eyes was 20/20 and neither complained of visual discomfort. In conclusion, we found that a reversed-optic Tecnis multifocal IOL in the present case resulted in good final visual acuity without significant differences in aberrations compared to the other eye, and a conservative management can be taken as a safe option.
Keywords: Lens implantation, intraocular; Visual acuity; Case report
RESUMO
Paciente de 51 anos, sexo feminino, apresentando catarata foi submetida a cirurgia de facoemulsificação com implante de lente intraocular (LIO) multifocal Tecnis ZM900 em ambos os olhos (AO). Durante a implantação da LIO no olho esquerdo, a lente foi inadvertidamente implantada invertida e deixada dessa maneira. Seis meses pós-operatório a surpresa refracional não se mostrou significativa e a acuidade visual corrigida era de 20/20 em AO, sem nenhuma queixa de desconforto visual. Em conclusão, no presente caso, o implante de uma LIO Tecnis multifocal invertida resultou em boa acuidade visual final e sem diferenças significativas na aberrometria em comparação ao olho contralateral, tendo sido possível conduzir o caso de maneira conservadora.
Descritores: Implante de lente intraocular; Acuidade visual; Relato de caso
CASE REPORT RELATO DE CASO
Inadvertent implantation of a reversed-optic Tecnis ZM900 multifocal intraocular lens: case report
Implante invertido da lente intraocular Tecnis ZM900 multifocal: relato de caso
Wilson Takashi HidaI,II; Antonio Francisco MottaII; Celso Takashi NakanoII; Patrick F. TzelikisI
IPhysician, Hospital Oftalmológico de Brasília - HOB - Brasília (DF), Brazil
IIPhysician, Universidade de São Paulo - USP - São Paulo (SP), Brazil
ABSTRACT
A 51-year-old woman with age-related cataract had an uneventful phacoemulsification and a Tecnis ZM900 multifocal intraocular lens (IOL) implantation in both eyes. During IOL implantation in the left eye, the optic was unintentionally reversed in the bag and left that way. The refraction surprise was not significant and six months postoperatively the corrected distance visual acuity in both eyes was 20/20 and neither complained of visual discomfort. In conclusion, we found that a reversed-optic Tecnis multifocal IOL in the present case resulted in good final visual acuity without significant differences in aberrations compared to the other eye, and a conservative management can be taken as a safe option.
Keywords: Lens implantation, intraocular/adverse effects; Visual acuity; Case report
RESUMO
Paciente de 51 anos, sexo feminino, apresentando catarata foi submetida a cirurgia de facoemulsificação com implante de lente intraocular (LIO) multifocal Tecnis ZM900 em ambos os olhos (AO). Durante a implantação da LIO no olho esquerdo, a lente foi inadvertidamente implantada invertida e deixada dessa maneira. Seis meses pós-operatório a surpresa refracional não se mostrou significativa e a acuidade visual corrigida era de 20/20 em AO, sem nenhuma queixa de desconforto visual. Em conclusão, no presente caso, o implante de uma LIO Tecnis multifocal invertida resultou em boa acuidade visual final e sem diferenças significativas na aberrometria em comparação ao olho contralateral, tendo sido possível conduzir o caso de maneira conservadora.
Descritores: Implante de lente intraocular/efeitos adversos; Acuidade visual; Relato de caso
INTRODUCTION
With emerging technology, wavefront-corrected intraocular lens (IOLs) will likely be introduced as a means of improving visual quality in pseudophakic eyes(1). An obvious concern about these wavefront-corrected lenses is the required accuracy of position and centration of the lens(2).
Although it has been known that decentration and tilt of the IOL can cause unwanted optical image or dysphotopsia(3), the influence of an reversed-optic (upside down) aspherical multifocal IOL on the optical quality of the eye has never been reported. We describe and compare one patient that received inadvertently an implantation of a Tecnis ZM900 multifocal IOL in an opposite-side in 1 eye and the same IOL in the corrected position in the fellow eye.
CASE REPORT
A 51-year-old woman presented with blurred vision caused by a cataract in both eyes and requested cataract surgery. In February 2007, uneventful phacoemulsification was performed initially in the OD with implantation of a +23.50 D Tecnis multifocal ZM900 IOL under topical anesthesia through a 2.7 mm superior clear corneal incision. The targeted postoperative refractive error was 0.0 D. One week later, cataract surgery was performed in the OS using a similar procedure with implantation of a +24.00 D Tecnis multifocal ZM900 IOL under topical anesthesia. However, during IOL implantation in the OS, the IOL rapidly unfolded into the capsular bag and the optic was unintentionally reversed in the bag. It was left that way because the patient was no longer collaborative, started to feel pain and the pupil diameter was getting smaller. One month postoperatively, the uncorrected distance visual acuity (UCVA) was 20/20 in the right eye with a refraction of +0.50 -0.50 x 135 and 20/50 in the left eye with a refraction of -0.75 -0.50 x 110. The refraction in the OS gradually developed regression in the myopic shift and the OD was stable from 1 month to 6 months. Six months postoperatively, the UCVA was 20/20 in both eyes with a refraction of +0.25 -0.50 x 140 in the right eye and -0.25 -0.25 x 110 in the left eye. The uncorrected near visual acuity (UNVA) at 35 cm was 20/20 (J1) in both eyes, and the uncorrected intermediate visual acuity (UIVA) at 80 cm was 20/40 (J5) in the OD and 20/25 (J2) in the OS (Table 1). The corneas were clear and the anterior chamber quiet bilaterally.
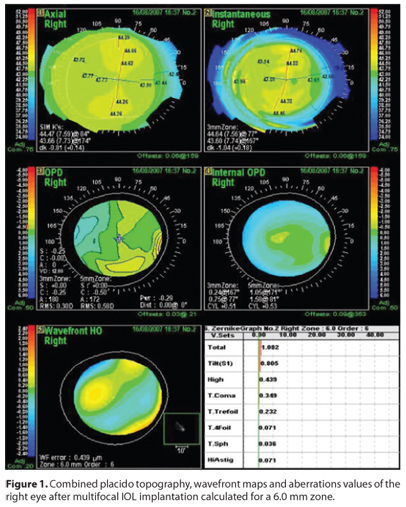
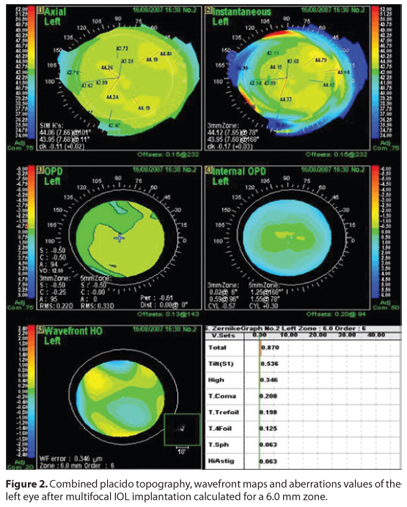
Wavefront analysis was performed 6 months postoperatively with OPD-scan (Nidek Co. , Ltd. , Gamagori, Japan). Total-eye wavefront analysis revealed moderate negative spherical aberration in both eyes with RMS values of 0.036 and 0.063 in the right and left eye, respectively. Postoperative wavefront maps with Zernike modes and aberrations values are shown in figures 1 and 2. Figure 3 shows modulation transfer function (MTF) measurements of both eyes with similar performance levels to each other.
The patient did not report visual discomfort and was satisfied with the amount of improvement in her vision in both eyes. Despite a myopic shift was expected due to the anterior effective lens position this seemed not to worsen postoperative refraction and UCVA in this case. Three and a half years later, the UCVA dropped from 20/20 to 20/40 in the left eye as a result of posterior capsule opacification and an Nd:YAG posterior capsulotomy was performed without complications.
DISCUSSION
Along with the corneal optics, the geometry and positioning of the IOL contribute to the eye's optical quality(4,5). The literature offers little information related to the inadvertent implantation of a reversed-optic posterior chamber IOL and no information related to a reversed-optic multifocal IOL. A survey of members of the American Society of Cataract and Refractive Surgeons (ASCRS) evaluating the complications requiring explantation of or secondary intervention with foldable IOLs over the past calendar year found that aberrations, glare and optical phenomena remained the most common reason for multifocal IOL explantation, followed by incorrect IOL power, and dislocation or decentration(2).
One possible complication related to reversed-optic IOL implantation is capsular block syndrome (CBS)(6). Another complication is the refractive consequences of implanting a reversed-optic IOL. The refractive change with a reversed-optic IOL depends on the IOL design(7). Haptic angulation seems to be an important determinant for refractive change. Reversing the optic also reverses the orientation of the haptics; instead of angling forward and displacing the optic toward the retina, the haptics angle backward, shifting the optic toward the cornea. Halpern and Gallagher(8) conducted a retrospective study in which they evaluated the refractive consequences of inadvertently implanting a reversed-optic AMO SI-40NB IOL and found no significant differences between the reversed and nonreversed IOLs. The SI-40NB is a three-piece posterior chamber IOL with a biconvex silicone optic and polymethyl methacrylate haptics extruded at a 100 anterior angulation.
In the present case, the IOL implanted was the Tecnis ZM900. The Tecnis ZM900 multifocal IOL is a second-generation silicone diffractive 3-piece lens, with a biconvex square-edged 6.0 mm optic and a 60 haptic angulation. The spherical equivalent refraction with the Tecnis reversed-optic IOL in our patient was -1.00 D at 1 month and the regression of the myopic shift was 0.50 D after 6 months of follow-up. Halpern and Gallagher(8) compared the mean refraction surprises for reversed and nonreversed SI-40NB IOL and they differed by less than 1.0 D. The Tecnis ZM900 possess haptics with smaller degrees of angulation than the SI-40NB IOL, therefore, refractive error surprises are supposed to be even smaller than for the SI-40NB IOL.
The wavefront measurement of a reversed-optic IOL has never been reported. Using a standardized 6.0 mm pupil diameter for aberrations and objective quality-vision measurements (MTF), our case report found that a reversed-optic IOL produce at most a minimal change compared to the nonreversed IOL; therefore, a surgical reposition was not required.
The final position of a reversed IOL is not well understood since there are few reports of this. A reversed, anteriorly dislocated IOL optic will move backward and settle near the line of the lens equator as the anterior and posterior capsule coalesce. Despite further comparative studies are required, in an accidental reversed-optic IOL implantation, a conservative management can be taken as a safe option depending on the IOL type.
REFERENCES
1. Tzelikis PF, Akaishi L, Trindade FC, Boteon JE. Spherical aberration and contrast sensitivity in eyes implanted with aspheric and spherical intraocular lenses: a comparative study. Am J Ophthalmol. 2008;145(5):827-33.
2. Mamalis N, Brubaker J, Davis D, Espandar L, Werner L. Complications of foldable intraocular lenses requiring explantation or secondary intervention-2007 survey update. J Cataract Refract Surg. 2008;34(9):1584-91.
3. Kosaki J, Tanihara H, Yasuda A, Nagata M. Tilt and decentration of the implanted posterior chamber intraocular lens. J Cataract Refract Surg. 1991;17(5):592-5.
4. Barbero S, Marcos S, Jiménez-Alfaro I. Optical aberrations of intraocular lenses measured in vivo and in vitro. J Opt Soc Am A Opt Image Sci Vis. 2003;20(10):1841-51.
5. Packer M, Chu YR, Waltz KL, Donnenfeld ED, Wallace RB 3rd, Featherstone K, et al. Evaluation of the aspheric tecnis multifocal intraocular lens: one-year results from the first cohort of food and drug administration clinical trial. Am J Ophthalmol. 2010; 149(4):577-84.e1.
6. Xiao Y, Wang YH, Fu ZY. Capsular block syndrome caused by a reversed-optic intraocular lens. J Cataract Refract Surg. 2004;30(5):1130-2.
7. Nawa Y, Tsuji H, Ueda T, Okamoto M, Kojima M, Hara Y. Long-term observation of the refraction with a reversed-optic posterior chamber intraocular lens. J Cataract Refract Surg. 2004;30(5):1133-5.
8. Halpern BL, Gallagher SP. Refractive error consequences of reversed-optic AMO SI-40NB intraocular lens. Ophthalmology. 1999;106(5):901-3.
 Correspondence address:
Correspondence address:
Patrick F. Tzelikis
SQN 203 - Bloco G - Apto. 405
Brasília (DF) - 70833-070 - Brazil
E-mail: [email protected]
Submitted for publication: August 27, 2012
Accepted for publication: October 14, 2012
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: W.T.Hida, None; A.F.Motta, None; C.T.Nakano, None; P.F.Tzelikis, None.
Study carried out at Hospital Oftalmológico de Brasília and the Department of Ophthalmology, Universidade de São Paulo - USP.