INTRODUCTION
Acetazolamide is known to induce bilateral angle closure(1). We report a case of acetazolamide-induced bilateral angle closure documented with ultrasound biomicroscopy (UBM) from its onset to its resolution.
CASE REPORT
A 49-year-old female presented to the emergency department with vomiting and blurred vision while wearing her own glasses. No headache or ocular pain was referred. Past ocular history: hyperopia of +1.50 diopters (d) in both eyes. Current examination: uncorrected visual acuity (VA) was 20/25, with a myopic shift of -1.50 d, in both eyes (OU). Slit-lamp examination showed a flat central and peripheral anterior chamber (Figures 1 and 2, A). The intraocular pressure (IOP) was 15 and 11 mmHg in the right (OD) and left (OS) eyes, respectively, as measured by Goldmann applanation tonometry. Both eyes revealed no visible angle structures using 360° gonioscopy. The undilated ocular fundus showed an optic disc with a cup/disc ratio of 0.2 × 0.2 in both eyes.
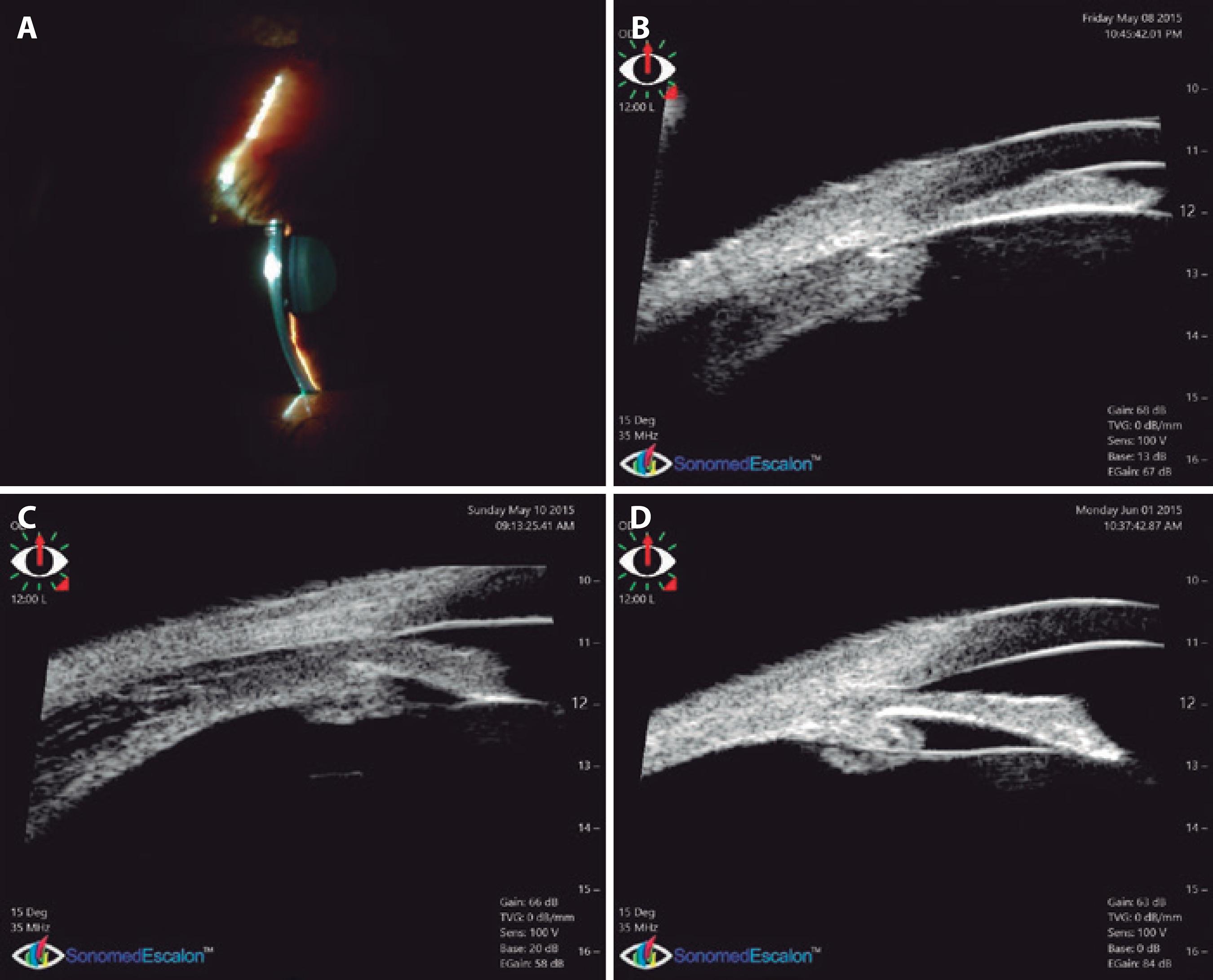
Figure 1 (OD) First day: shallow central and peripheral anterior chamber (A) and UBM showing ciliary detachment and anterior rotation provoking complete iridocorneal apposition (B). Thirty-six hours later: widened angle with mydriatic pupils caused by cycloplegia. Ciliary detachment persists (C). Three weeks later: reattached ciliary body. Angle is wider but still narrow, and with a relative pupillary block configuration (D). All UBM images shown here are from the superior quadrant.

Figure 2 (OS) First day: shallow central and peripheral anterior chamber (A) and UBM showing ciliary detachment and anterior rotation provoking complete iridocorneal apposition (B). Thirty-six hours later: widened angle with mydriatic pupils caused by cycloplegia. Ciliary detachment persists (C). Three weeks later: reattached ciliary body. Angle is wider but still narrow, and with a relative pupillary block configuration (D). All UBM images shown here are from the superior quadrant.
Questioning of the patient revealed that she had taken two tablets of 250 mg of acetazolamide 2 days prior. Five hours later, she started vomiting and, the following day, she developed bilateral blurred vision. She mentioned that 3 weeks prior, she had taken four tablets of 250 mg of this drug to prevent mountain sickness and had experienced a visual improvement after taking the drug. In an attempt to achieve the same visual result, she had decided to take acetazolamide again.
Immersion UBM with a 35-MHz probe (Figures 1 and 2, B) showed bilateral ciliary body effusion and anterior chamber flattening with complete appositional angle closure in all quadrants, which was more evident in OD. Iris contact was complete in OD, whereas OS showed a pupillary block mechanism, with the ciliary body anteriorly rotated to a lesser extent.
Topical therapy with 1% prednisone and 1% cyclopentolate and an intramuscular injection of deposit betamethasone were indicated, together with immediate suppression of acetazolamide.
Thirty-six hours later, the anterior chamber and angle had widened, but UBM demonstrated continued ciliary effusion (Figures 1 and 2, C). A conventional ultrasound exam was performed, which showed a shallow peripheral uveal detachment and the presence of vitreous hyperreflectivity consistent with vitritis. The patient went on a trip overseas and continued her medication.
Three weeks later, upon returning, her VA was 20/20 OU corrected with +1.50, and slit-lamp examination showed OU with a wider anterior chamber, IOP of 12 mmHg, and normal ocular fundus. The results from UBM were consistent with these findings, showing a widened anterior chamber angle and complete resolution of the ciliary effusion (Figures 1 and 2, D). Nevertheless, the anterior chamber angle remained occludable, with a relative pupillary block configuration. Therefore, a bilateral laser peripheral iridotomy was indicated; at this point, steroid and cycloplegic drops were no longer being used by the patient.
DISCUSSION
Some case reports have been published on drug-induced bilateral angle closure or myopia, and most of them are associated with the use of sulfa-derived drugs, such as topiramate and acetazolamide(1).
Acetazolamide is currently used for adjunctive treatment of different medical conditions such as edema caused by congestive heart failure, drug-induced edema, centrencephalic epilepsy, and different types of glaucoma. It is also indicated for the prevention or amelioration of symptoms associated with acute mountain sickness in climbers attempting rapid ascent and in those who are very susceptible to acute mountain sickness despite gradual ascent(2). In reference to the latter, dosing regimes vary greatly depending on the source one consults. The medication label advises a divided daily oral dose of 500-1000 mg(2), whereas the Centers for Disease Control (CDC) Yellow Book(3) and Wilderness Medical Society(4) both suggest a lower twice-daily oral dose of 125 mg for prevention and 250 mg for treatment.
Drug’s mechanism to alter the body’s response to altitude is believed to be produced by metabolic acidosis through increased bicarbonate excretion and minute ventilation resulting in hypoxic pulmonary hypertension(5).
The mechanism by which acetazolamide results in bilateral angle closure is still unclear, although some have postulated an idiosyncratic hypersensitivity reaction in which the blood-ocular barrier may be disrupted. In part, it may be due to local stimulation of prostaglandin E2 synthesis, which in turn causes vasodilation and increased vascular permeability in the anterior uvea(6). This causes rapid-onset bilateral ciliary effusion with forward displacement of the lens-iris diaphragm and thickening of the lens, resulting in myopic shift and anterior chamber shallowing(1,7-9). These signs were observed with UBM in the present case. There are few published cases in which bilateral angle closure induced by acetazolamide were studied with UBM(10,11). This diagnostic tool had already been used to show that topiramate may result in bilateral angle closure with ciliary body effusion(12-14).
Our patient had taken 1 g of acetazolamide (four tablets of 250 mg each) to prevent mountain sickness and, 2 weeks later, had taken another 500 mg (two tablets of 250 mg each). Both doses are within the boundaries of the label’s recommendations; however, the only aim of the second intake of the drug was to overcome her hyperopia without glasses.
We presume that the reduction of the hyperopia in our patient was due to forward displacement of the lens caused by the uptake of acetazolamide. This effect led her to believe that regular use of this drug would benefit her vision. However, further use of the drug triggered another condition, with opposite effects.
Our patient presented with vomiting without headache or ocular pain; which could have been related to gastrointestinal irritation, common with acetazolamide ingestion.
A differential diagnosis is intermediate uveitis because of the presence of vitritis. This condition can also cause uveal effusion and can be improved by cycloplegic and steroid treatment; however, in our case, the onset of the symptoms occurred immediately after the uptake of the drug, the situation resolved soon after its withdrawal, and the patient has remained asymptomatic ever since.
In congruence with published data, the main symptom in our case was an unexpected worsening of vision(8). Conversely, her IOP remained unchanged despite the angle closure, which is not as unusual as it seems, and has been reported in previous cases(15). A possible reason for this lack of change in her IOP may be secretory shutdown caused by carbonic anhydrase inhibition and by the ciliary effusion itself(16).
It is unclear if the acetazolamide cessation alone improved the condition, because we added cycloplegic and steroid treatment, following the recommendations of a paper by van Issum et al.(7) The patient had gone on a trip overseas 2 days after initiating the anti-inflammatory treatment, and therefore, the condition might have resolved at any time before the last UBM examination.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

