INTRODUCTION
The Argentinean-flag sign is a known complication during curvilinear continuous capsulorhexis (CCC) in hypermature or intumescent cataracts characterized by a spontaneous tear in the anterior capsule extending into the periphery as a result of high in tracapsular pressure. This complication can compromise the final visual result by causing lens decentration, tilting, or even aphakia because of the absence of capsule support.
Many techniques have been proposed to prevent the development of this complication, such as use of a small CCC, cortex aspiration using a 27-gauge cannula for the initial puncture, or use of a femtosecond laser to perform CCC. However, none of these methods is capable of preventing this complication during primary posterior curvilinear continuous capsulorhexis (PCCC).
In this paper, we describe a spontaneous posterior capsule tear after the initial puncture during PCCC in a patient with megalocornea scheduled for toric multifocal intraocular lens (IOL) implantation with reverse optic capture to prevent intracapsular IOL rotation.
CASE REPORT
A 53-year-old man presented to our clinic with blurred vision in both eyes. His best corrected visual acuity was 20/25 and 20/30 with -3.50 sphere (sph) -3.50 cylinder (cyl) @ 170º in the oculus dextrus (OD) and -6.00 sph -0.75 cyl @ 160º in the oculus sinister (OS). Slit-lamp examination revealed a large corneal diameter, Descemet's membrane with no sign of tears, a deep anterior chamber depth (ACD), and a 1+ nuclear cataract in the OD and 2+ nuclear cataract in the OS with no signs of phacodonesis or iridodonesis. Gonioscopy revealed an open angle with no abnormalities. Intraocular pressure was 13 mmHg in both eyes. The findings of fundoscopy were unremarkable.
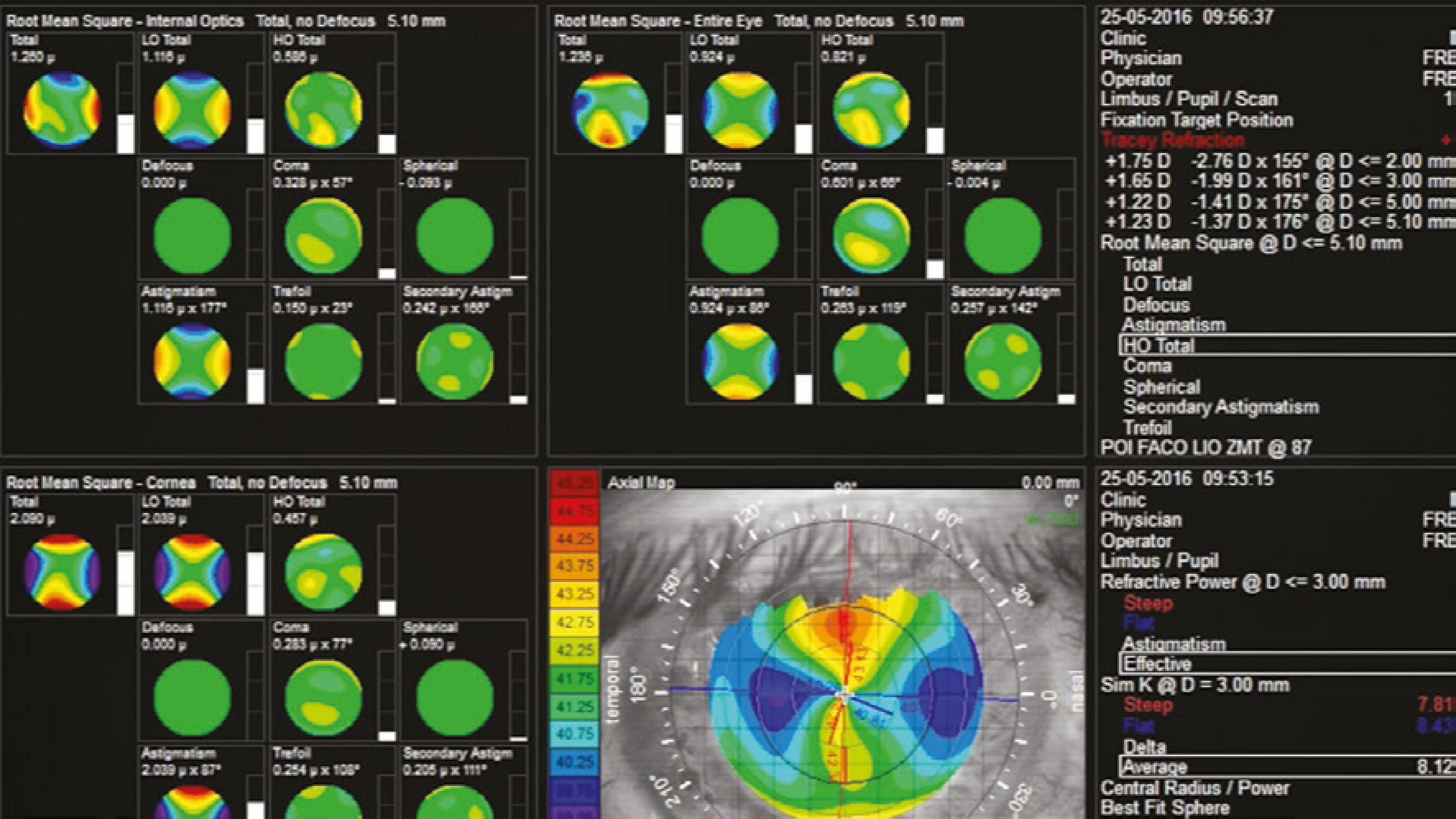
The simulated keratometry readings were 41.02 × 43.56 @ 93º in the OD and 41.61 × 42.5 @ 104º in the OS (iTrace; Tracey Techno logies LLC, Houston, TX, USA). Axial length measured 27.32 mm in the OD and 27.51 mm in the OS; ACD measured 4.12 mm in the OD and 4.18 mm in the OS; and the white-to-white (W-W) diameter was 13.7 mm in the OD and 14 mm in the OS as measured using an IOLMaster® 500 (Carl Zeiss AG, Oberkochen, Germany). The findings of optical coherence tomography of the maculae were normal in both eyes.
After thorough discussion of the oversized capsular bag and possible IOL decentration with the patient, we decided to implant bilateral multifocal IOLs. For the first eye (OS), after performing an uneventful phacoemulsification, we implanted a non-toric +12.0 Tecnis ZMA00 (Abbott Medical Optics Inc., Santa Ana, CA, USA) into the capsular bag with no complications regarding IOL centration. The patient achieved excellent postoperative visual acuity on Day 1 with an uncorrected visual acuity (UCVA) of 20/20 and J1. Regarding the other eye, because of its corneal astigmatism, a Tecnis ZMT300 (Abbott Medical Optics Inc.) toric 13.0 D multifocal IOL was placed at 87º.
Based on the high possibility of lens rotation because of the large capsular bag and single-piece design of the IOL, we planned to perform phacoemulsification with primary PCCC to achieve reverse capture of the IOL optic zone, thus ensuring IOL stability.
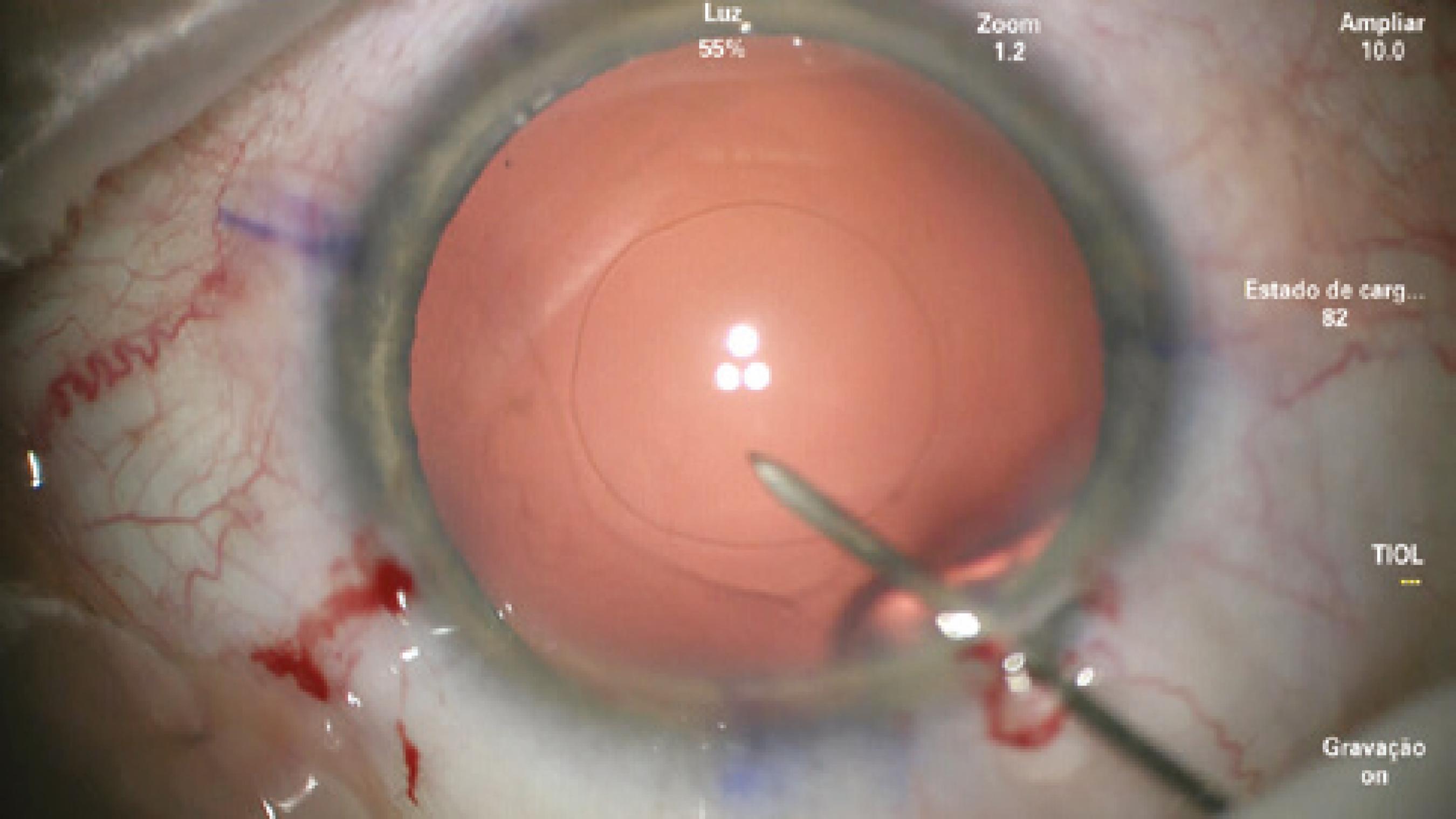
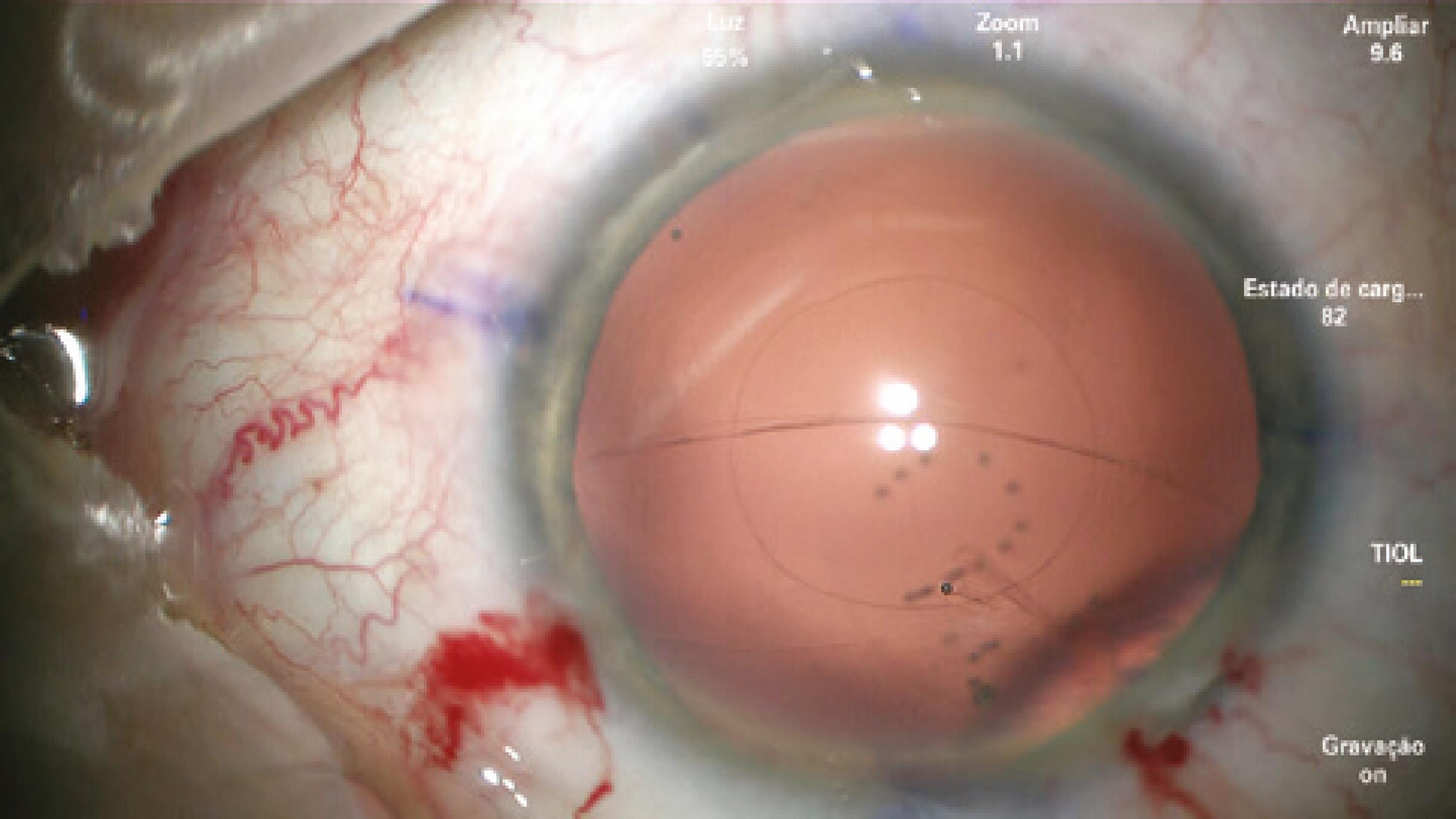
After confirming the 14-mm W-W diameter with calipers, phacoemulsification and cortical aspiration were performed without complications. To perform PCCC, the capsular bag was filled with a cohesive viscoelastic device (ProVisc®; Alcon Laboratories, Inc., Fort Worth, TX, USA). A 27-gauge needle mounted in a dispersive ophthalmic viscosurgical device (OVD; Viscoat®, Alcon Laboratories, Inc.) was used to perform the initial puncture of the central posterior capsule and inject dispersive viscoelastic into Berger's space to avoid rupture of the anterior hyaloid membrane (Figure 1). However, as soon as the posterior capsule was punctured, a tear extended spontaneously to the periphery in a similar fashion to an Argentinean-flag sign in the anterior capsule (Figure 2). Because the eye was well pressurized with a stable anterior chamber, the anterior hyaloid membrane remained intact and no vitreous humor prolapsed. IOL insertion into the capsular bag was performed using a bimanual technique with extreme caution to avoid extending the tear, vitreous humor prolapse, and dropping the IOL into the vitreous cavity.
After gentle sequential maneuvers, the IOL was centered and aligned on the desired axis with satisfactory stability. The OVD in the anterior segment was carefully washed out with light depression of the main incision during irrigation, taking care to preserve anterior chamber stability. A miotic agent was used to bring the pupil down, and a spatula through the side port was used to confirm the absence of vitreous. The incisions were hydrated, and topical antibiotic was instilled.
On Day 1, his UCVA was 20/30 and J2 p, and the IOL was on the correct axis (Figure 3). One week later, the patient was very pleased with his UCVA of 20/25 J2, with a manifest refraction of +0.25 -0.50 @ 10º achieving the same visual acuity because of some degree of amblyopia probably originating from the higher corneal astigmatism in this eye.
DISCUSSION
Capsule extension during capsulotomy can occur at any time during capsulorhexis maneuvers. Usually, it occurs because increased intracapsular pressure directs the vector forces of the capsule tear toward the zonules. This situation can be abrupt, and it is commonly found in hypermature cataracts, leading to the well-known Argentinean-flag sign.
Our patient had megalocornea, which is a developmental anomaly of unknown etiology characterized by enlargement of the cornea to 13 mm or greater. The condition can be associated with anterior megalophthalmos and/or dysgenesis of the iris, lens, and ciliary body, and exhibits X-linked recessive inheritance(1). Fortunately, the zonules were intact and no capsular bag abnormalities, which can make toric alignment a real challenge, were found besides the large corneal size.
The main factors leading to postoperative IOL rotation away from the intended vertical meridian are eyes with an axial length greater than 25 mm and with-the-rule astigmatism(2). Many techniques have been described to avoid this rotation or realign the IOL, such as insertion of a regular capsular tension ring (CTR) and/or Henderson's CTR to increase the area of contact within the IOL haptic and optic zone by stretching the posterior capsule or even suturing the IOL to a CTR, or PCCC to achieve reverse optic capture performed manually or using a femtosecond laser(3-6). In our case, another option was to insert the IOL inside the capsular bag and capture just the optic anteriorly, leaving the haptics inside the bag; however, because of the increased chance of pigment-dispersion glaucoma secondary to chafing between the posterior surface of the iris and the square edge of the IOL optic, we decided against this procedure(7).
Because of the large W-W diameter of 14 mm, the IOL diameter of 13 mm, and the intended axis of 87º, we decided to perform PCCC with reverse optic capture as described by Gimbel(4) for correct IOL alignment and centration instead of using CTRs because, in most patients with megalocornea, the CTR alone is insufficient. To perform PCCC, the anterior chamber must be stable and the posterior capsule concave after the initial puncture to create a small tear; dispersive viscoelastic must be injected into Berger's space to protect the anterior hyaloid membrane; and once the tear is created, Utrata forceps must be used to create a circular opening.
In our opinion, the cause of posterior capsule extension during the primary PCCC, although inverse, was the same the that encountered in eyes with the Argentinean-flag sign: the capsular bag was overfilled within cohesive viscoelastic, leading to an extremely concave posterior capsule and extending the intentional tear immediately after the initial puncture toward the periphery, similarly to an Argentinean-flag sign. To our knowledge, this finding has never been demonstrated before.
In summary, when planning a PCCC, the surgeon must consider the possibility of this complication, which can be avoided by using a small amount of cohesive viscoelastic to induce minimal distention of the posterior capsule. Avoiding overfilling the capsular bag may prevent peripheral extension of the tear.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

