INTRODUCTION
Central serous chorioretinopathy (CSC) is a disease characterized by detachment of the serous retinal pigment epithelium (RPE), typically in the macular region, and that is associated with fluid extravasation into the subretinal space(1). The disease mainly affects middle-aged men, although women are also commonly affected(2). Classified into acute and chronic types, the more common acute type usually has a benign course with spontaneous resolution and good final visual acuity(1). However, persistent complaints of metamorphopsia or of changes in color perception have been observed after CSC has resolved(3). These changes may be explained by injury to the ellipsoid band, demonstrated by optical coherence tomography (OCT), but the damage may also be imperceptible(4). Given that OCT alone provides limited resolution for detailed photoreceptor assessment, it is necessary to use more sensitive methods, like adaptive optics, which can compensate for optical aberrations and individually assess the photoreceptors(4,5). Herein, we report our experience using adaptive optics to assess a patient with persistent mild visual alterations in the left eye four years after resolution of CSC.
CASE REPORT
A 47-year-old white woman was seen at the Retina and Vitreous Sector of our hospital in 2012 with symptoms of metamorphopsia and central scotoma in the left eye (oculus sinister ; OS). She had no comorbidities, but reported that she was going through a period of intense emotional stress at the time. Her best-corrected visual acuity (BCVA) was 20/20 for the right eye (oculus dexter , OD; +0.5 D, sphere); by contrast, the BCVA for OS was 20/80 (+0.75 D, sphere). OCT revealed serous retinal detachment in OS (Figure 1), so a diagnosis of CSC was made and the patient's condition was observed. After three months of persistent signs and symptoms, we then started therapy with 250 mg acetazolamide tablets to be taken orally every 8 h for 20 days, and applied focal laser to the OS macular region using a PUREPOINT® Laser (Alcon, USA) set to 100 mW, 50 ms duration, and 33 firings. One month after treatment, clinical improvement was observed, and resolution of serous detachment was confirmed by OCT.
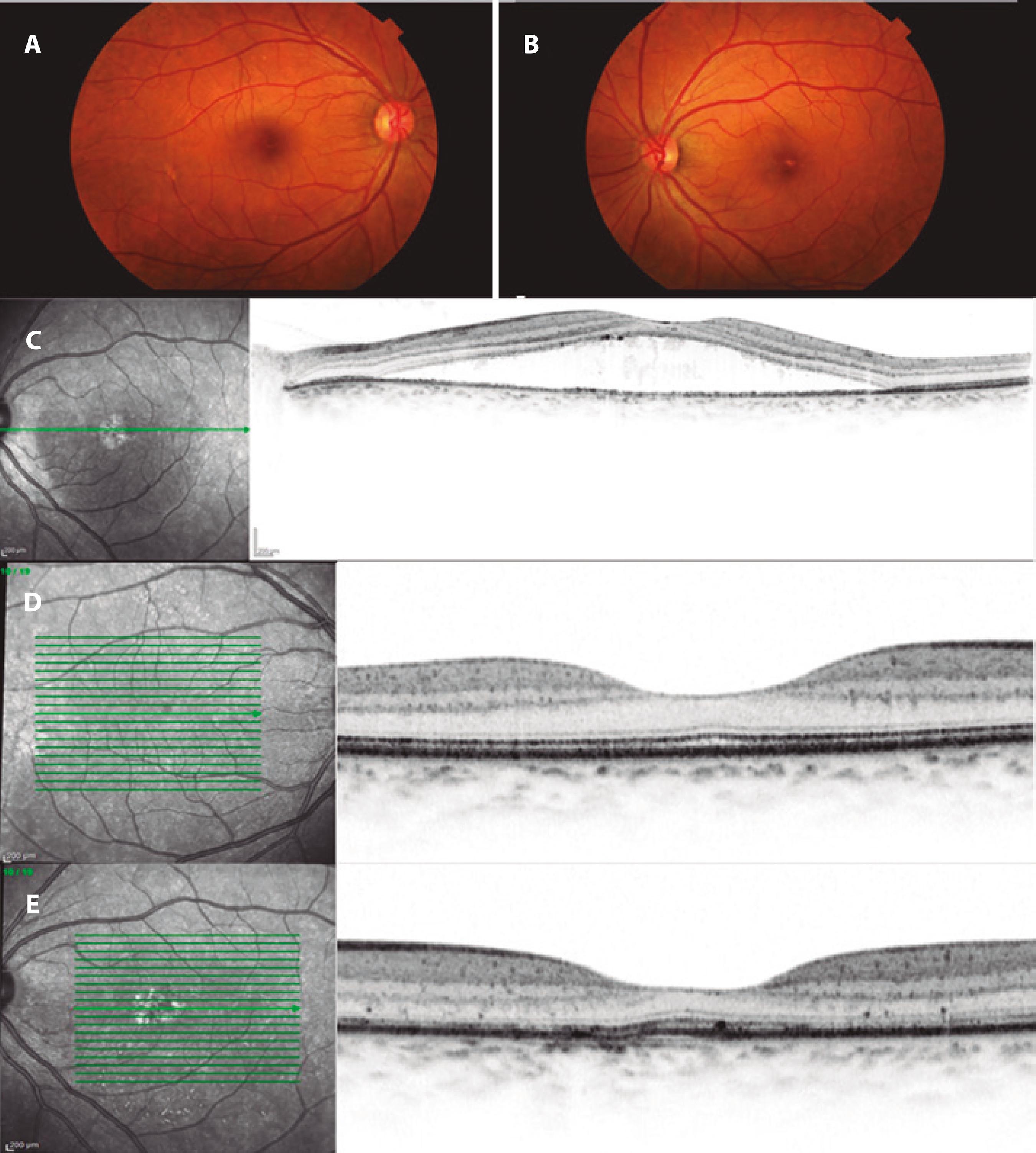
Figure 1 Retinography in OD (A) and OS (B). Yellowish lesions can be seen in the foveal topography of OS. The OCT of OS for the new case (C) shows separation of the photoreceptor layer of the RPE by foveal topography. A recent OCT of OD (D) is normal and in OS (E) there are marks of focal laser in the inferior macular area (infrared) and irregularities of the outer limiting membrane and Bruch/RPE complex in the selected section. OCT= optical coherence tomography; OD= oculus dexter; OS= oculus sinister; RPE= retinal pigment epithelium.
Although the patient suffered no new episodes during follow up, she continued to complain of diminished visual acuity in OS. Objectively, her BCVA was 20/20 in OD (+1.5 D sphere) and 20/25 in OS (+1.0 D sphere). Biomicroscopy revealed transparent corneas, trophic irises, transparent crystalline lenses, and intraocular pressures of 12 mmHg in both eyes. Posterior pole fundoscopy was also within normal limits in OD, but macular topography showed some areas with white and yellowish spots in OS (Figure 1). Therefore, OCT was done. This showed a normal OD with preserved foveal depression, an intact inner layer, and an intact outer layer. Although foveal depression was preserved, and the inner and outer layers were intact in OS, there were some irregular areas on the outer limiting membrane, as well as discrete elevations in both the RPE and Bruch's membrane (Figure 1). In OS, the laser marks in the macular and inferior macular regions were also evident in infrared.
We then performed assessment by adaptive optics using an RTX-1(tm) Adaptive Optics Retinal Camera (Imagine Eyes, Orsay, France), based on non-coherence of current illuminated by 850 nm central illumi nation, a wavelength with a 4° × 4° image field (1.2 × 1.2 mm on the retina), and a focus interval of 600 mm. Thus, high-resolution images were obtained of the cones. The images were processed using the software provided by CK V.0.1 and AOdetect V.0.1 (Imagine Eyes, France).
The adaptive optics analysis revealed mean cone densities of 16,121 and of 8,694 in the central regions of OD and OS, respectively (reference value: 20,000 to 30,000). The mean intercellular spacing was 8.65 µm in OD and 11.07 µm in OS (reference value: 15 to 20 µm). The greatest proportion of neighboring cells (Voronoi polygons) was six in both eyes (reference value, six), of which 40.2% were in OD and 35.8% were in OS (Figures 2 and 3).
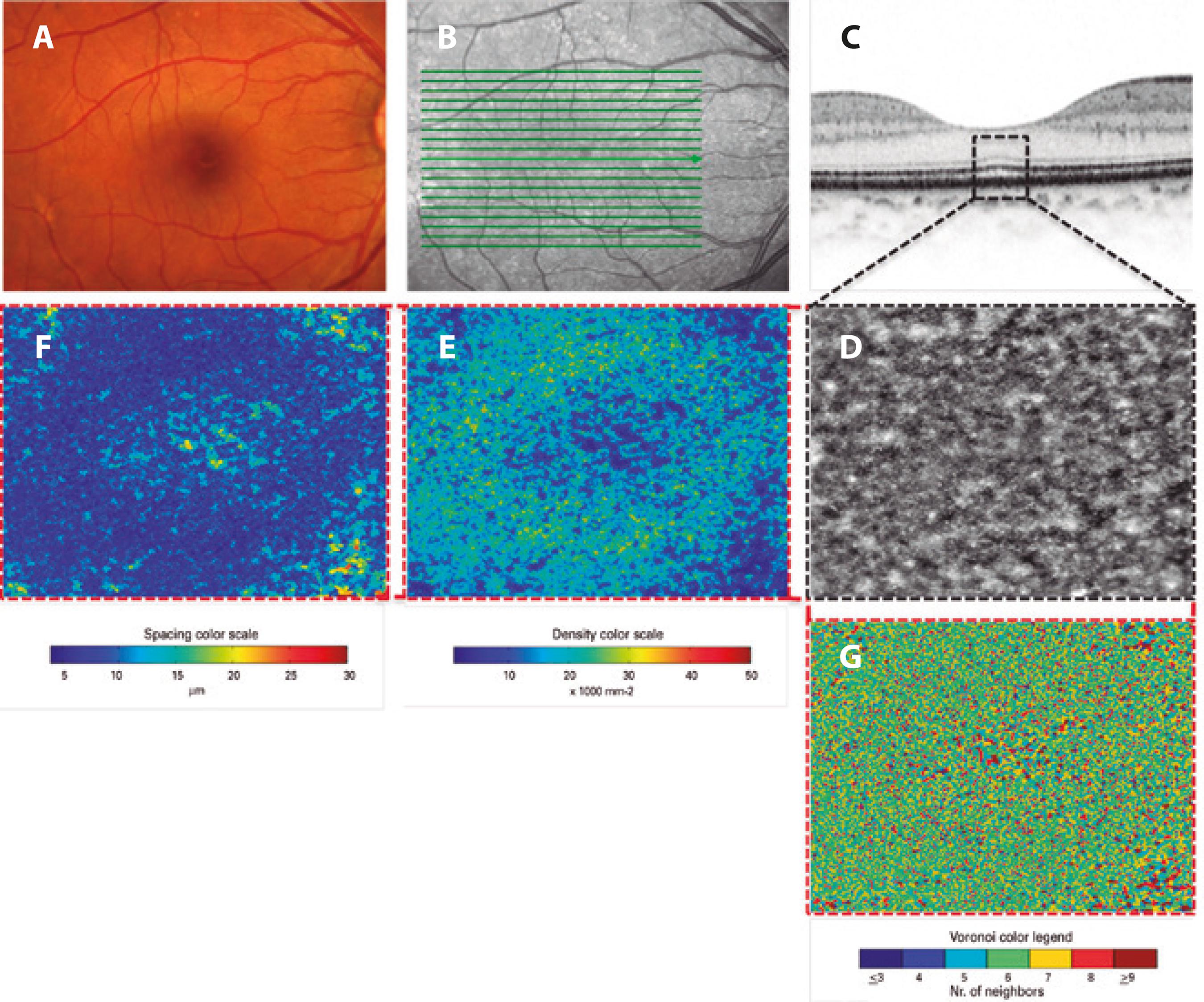
Figure 2 Imaging in OD. Retinography (A), infrared photograph (B), enlarged section obtained by OCT (C), enlarged central area obtained by adaptive optics (D). Also, density mosaics (E), spacing (F), and closeness (G). A near normal pattern of distribution, density, and closeness can be seen. Abbreviations: OCT, Optical coherence tomography; OD, oculus dexter; OS, oculus sinister.
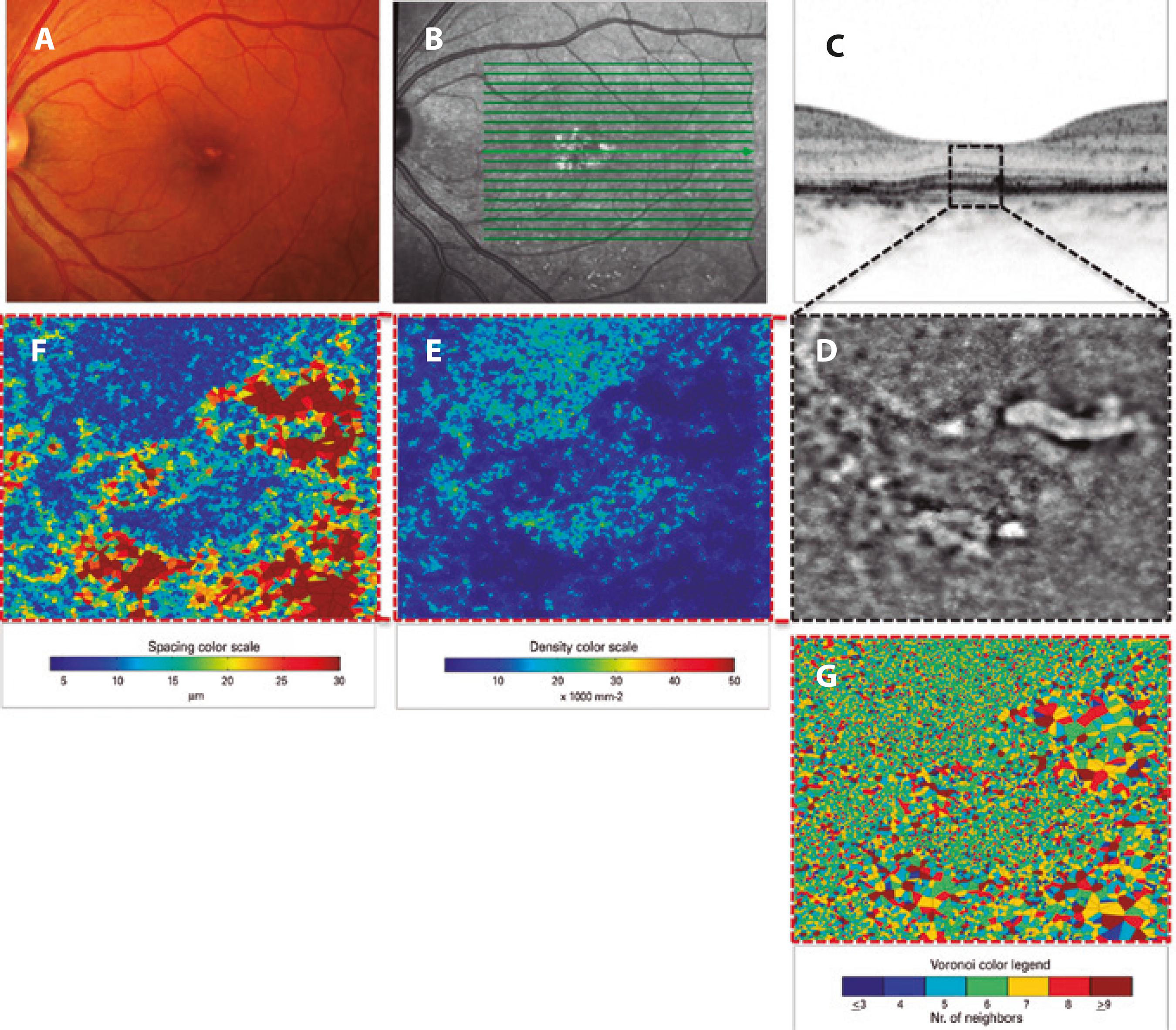
Figure 3 Imaging in OS. Retinography (A), infrared photograph (B), enlarged section obtained by OCT (C), and enlarged central area obtained by adaptive optics (D). Also, density mosaics (E), spacing (F), and closeness (G). Compared with OD imaging (Figure 2), there is a more irregular cone mosaic, and there are areas of reduced density and increased spacing, with a worse pattern of photoreceptor closeness. This suggests a loss of cones after CSC. CSC= central serous chorioretinopathy; OCT= optical coherence tomography; OD= oculus dexter; OS= oculus sinister.
DISCUSSION
Even though the morphological findings and visual acuity of the patient were within normal limits, her photoreceptor density and the spacing between photoreceptors were below the expected reference values. However, this does not mean that there was a cone deficiency in her eyes, because adaptive optics only detects part of the internal segment of the photoreceptor forming the mosaic. In addition, variations in the cone mosaic may occur due to physiological changes in reflectance caused by differences in the phases of photoreceptor phototransduction, axial length, or even circadian rhythm(6).
Comparison of the two eyes showed that not only were there clearly lower density and lower spacing in OS but that there were also changes in the mosaic pattern of the photoreceptors. This suggested that the resolved CSC caused changes in the cones, even after satisfactory clinical recovery. Ooto et al.(7) reported similar results in a case series of patients with CSC, and observed that there was a direct relationship between the intensity of photoreceptor changes measured by adaptive optics and the final BCVA.
In the present case, we showed that adaptive optics can provide additional data and reveal changes that might otherwise be missed if using OCT alone. Adaptive optics may represent a new assessment tool for use in the treatment and follow-up of patients with CSC or other macular diseases.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

