INTRODUCTION
Solitary fibrous tumor (SFT) is a rare mesenchymal spindle-cell tumor that can be found at various sites, such as the liver, nasal cavity, orbit, thyroid, meninges, skin, and kidney. However, the most common site of SFTs is the intra-thoracic region(1-4). Although it can affect the orbital region, SFT of the lacrimal gland and lacrimal fossa have rarely been observed and described(3-5). SFT commonly affects middle-aged adults, with equal distribution between genders. SFTs are well circumscribed, and their variably pattern-less spindle-cell lesions and immunopositivity for CD34 led the World Health Orga nization to redefine orbital SFTs using the same nomenclature for hemangiopericytoma, giant-cell angiofibroma, and fibrous histio cytoma of the orbit(6-10). Here, we describe the first case in Brazilian literature of lacrimal gland SFT mimicking pleomorphic adenoma in a 38-year-old woman, and we have demonstrated that a specific immunohistochemical (IHC) marker, signal transducer and activator of transcription 6 (STAT6), distinguishes SFTs from other tumors that mimic it histologically(8).
CASE REPORT
A 38-year-old woman presented with swelling in the left superolateral aspect of the orbit (lacrimal gland region) and an S-shaped ptosis for the past 4 years. There was gradual increase in lesion size over time. She had no history of trauma and had no ocular complaints. External examination revealed a palpable tumor in the orbit, specifically in the lacrimal gland. During examination, the mass was soft and did not appear to be attached to the periorbital rim. There was no proptosis. The Valsalva test was negative, and extraocular motility was normal (Figures 1A and 1B). Magnetic resonance imaging (MRI) revealed an extraconal solid nodule with defined, precise limits in the left lacrimal gland and intense heterogeneous enhancement by contrast, measuring about 2 × 2 × 1.4 cm (Figures 1C and 1D).
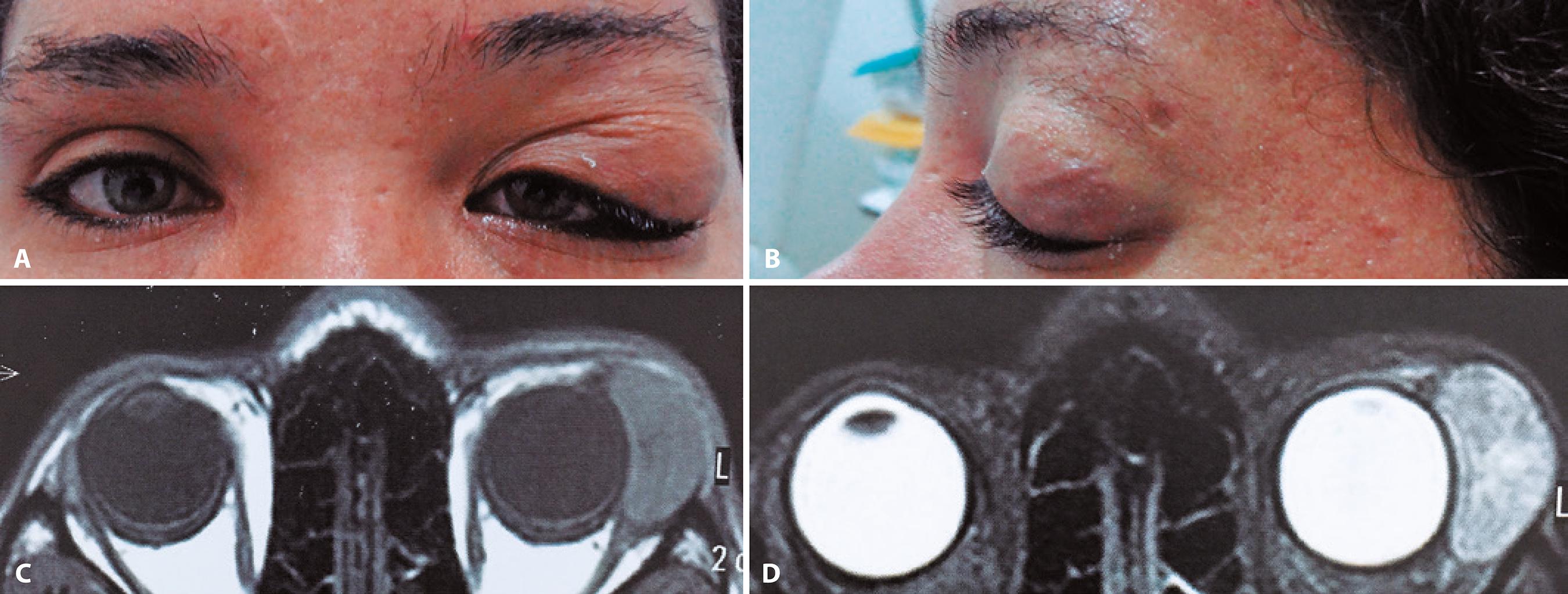
Figure 1 A) Tumor in superolateral region of the orbit, as determined via lacrimal gland topography. B) Side view. C and D: MRI revealed an extraconal solid nodule with defined limits in the left lacrimal gland, with intense heterogeneous enhancement by contrast, measuring about 2 × 2 × 1.4 cm, suggestive of pleomorphic adenoma of the lacrimal gland.
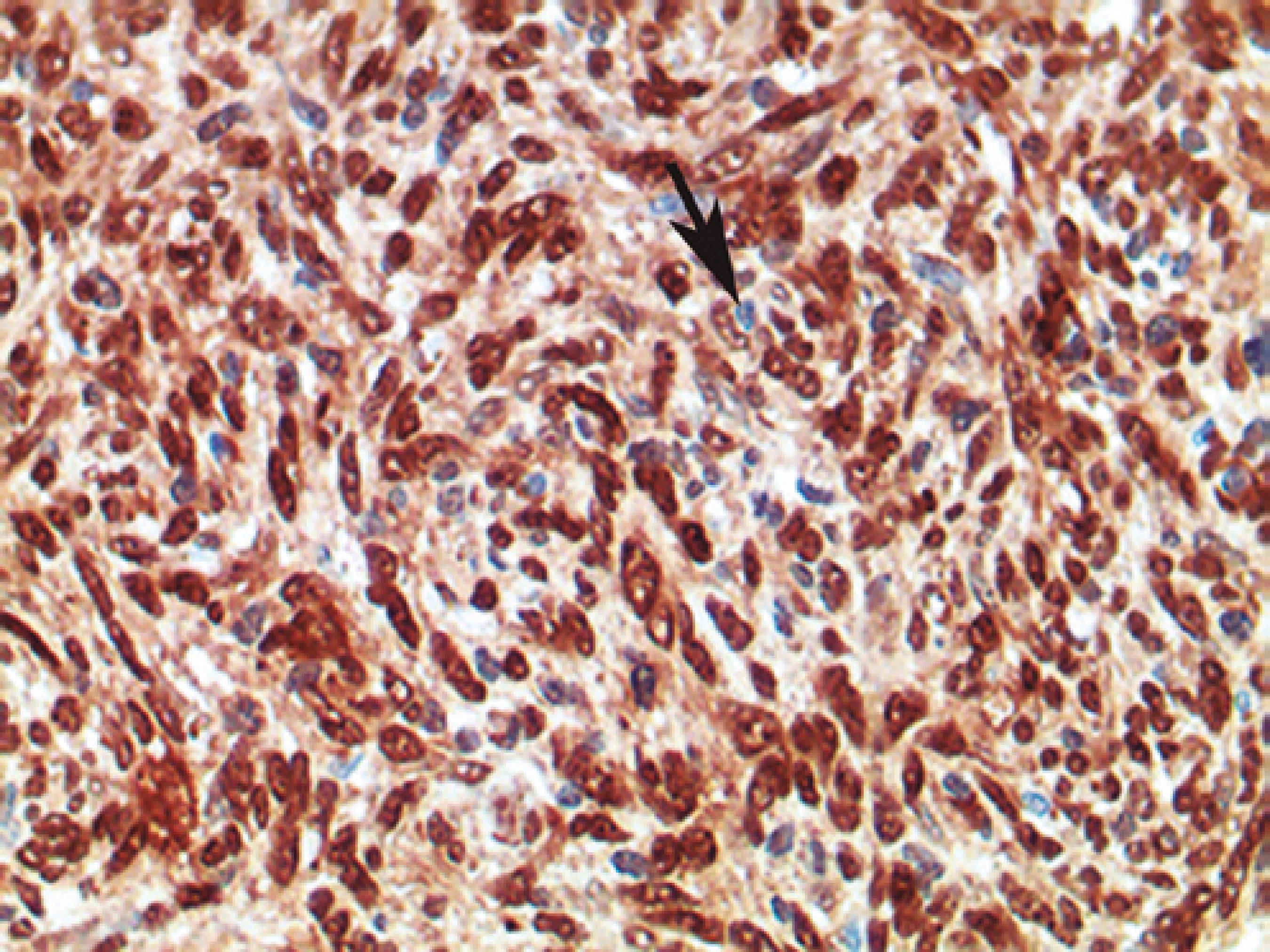
The mass was fully excised via a lateral orbitotomy approach, and a macroscopic presumptive diagnosis was typical pleomorphic adenoma. The excised tumor was ovoid and firm, measuring 2 × 2 × 1.5 cm. There were no bone changes caused by the tumor as determined via surgical exploration. Histopathological analysis of the tumor revealed mesenchymal neoplasia with a spindle-cell proliferative lesion and hemangiopericytoma-like pattern encircled by the lacrimal gland parenchyma. Mitotic activity was low. Histomorphology was suggestive of a benign spindle-cell tumor (Figures 2A and 2B). IHC showed that the spindle cells were highly positive for CD34 and STAT6 (Figure 3). S-100 protein and smooth muscle actin were not detected. An SFT was diagnosed based on these IHC and histological findings. During 6 months of follow-up there was no tumor recurrence.
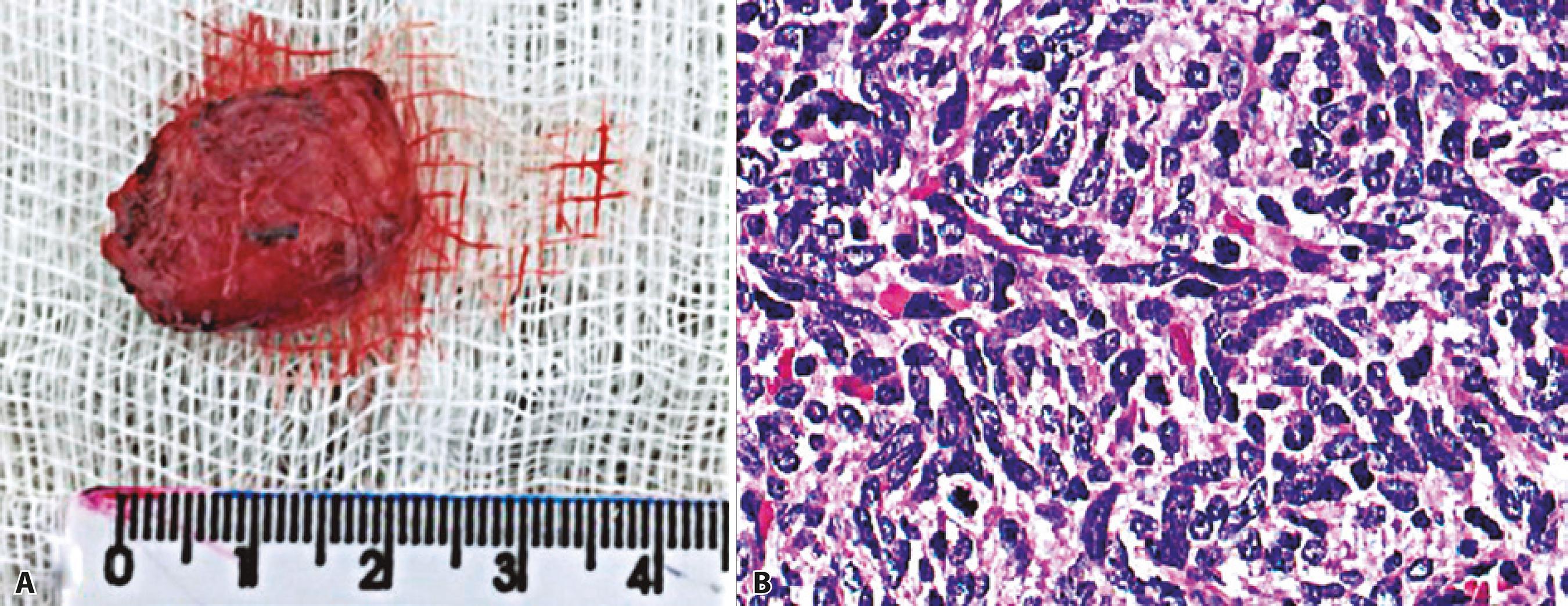
Figure 2 A) Macroscopic aspect of the tumor, well demarcated, ovoid, and firm, with measurements of 2 × 2 × 1.5 cm. B) The histopathological analysis of the tumor revealed a mesenchymal neoplasm with a spindle-cell proliferative lesion and hemangiopericytoma-like pattern as determined via hematoxylin-eosin staining.
DISCUSSION
SFT is a rare tumor, originally presumed to be derived from the mesothelium, that affects middle-aged adults, with no apparent sex predilection(1-5). However, these tumors are not often associated with serosal surfaces, such as the nasal cavity and paranasal sinuses, but rather are of a mesenchymal origin.
The orbit is an unusual site for SFT occurrence and generally presents with a slow and non-aggressive course, possibly achieving sizes of up to 4 cm(3-4). Our patient also had a slow-growing SFT, with a duration of 4 years and 2 cm in size. In this case, the external examination and MRI suggested pleomorphic adenoma of the lacrimal gland, which is the most common neoplasia of the lacrimal gland.
Dorfman et al.(4) also reported three cases of orbital region SFTs in a 44-year-old man, 65-year-old woman, and 69-year-old woman, with MRI and histopathological findings comparable with our case. However, our patient was younger; a 38-year-old woman.
Histopathological analysis has prognostic as well as diagnostic value. SFTs associated with hypercellularity, pleomorphism, and a high mitotic count (2:4 per 10 high magnification fields) are typically malignant, with relapse and distant metastases as possibilities. Vallat- Decouvelaere et al. (9) suggested that nuclear atypia, mitosis in 4:10 magnification fields, and necrosis in addition to hypercellularity are considered malignant features of SFTs. In our case, the mitotic count was two per 10-high-power fields. Nuclear pleomorphism, necrosis, or an invasive growth pattern were not observed in this study, suggesting a benign SFT.
Differential diagnoses according to histopathological findings include fibrous histiocytoma, schwannoma, and hemangiopericytoma. The differential diagnosis between hemangiopericytoma and SFTs is extremely important, because hemangiopericytoma has an aggressive clinical course with high relapse and higher rate of metastasis in contrast to the general benign nature of SFTs(3-5). Hemangiopericytoma classically consists of oval to spindle-shaped cells arranged around vessels. For definitive diagnosis, IHC is crucial. In most cases, an IHC of hemangiopericytoma shows a weak positivity to CD34 and a strong positivity to vimentin. Strong and consistent CD34 immunoreactivity in SFTs is critical to ensuring correct diagnosis(10).The present case showed spindle cells exhibiting strong immunoreactivity to CD34 and nuclear expression of STAT6(3, 4-6).
Recent molecular analyses have suggested that most SFTs express STAT6, and thus it is considered a specific marker to this neoplasia. Doyle et al.(8) investigated STAT6 nuclear expression by IHC in SFTs outside the central nervous system. They evaluated 60 SFT cases, and 59 (98%) of these cases displayed STAT6 nuclear expression, thus, clearly demonstrating it as a highly sensitive and specific marker for SFTs(8). As aforementioned, SFT is a rare tumor in the lacrimal gland region. Histopathological examination along with IHC findings are essential for correct diagnosis(6), and STAT6 is a suitable IHC marker to distinguish SFTs from other tumors that mimic it histologically, as clearly shown in this case report.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

