INTRODUCTION
Central serous chorioretinopathy (CSC) is an idiopathic disease of the retina and choroid that affects one or both eyes. The condition was first described by Albrecht von Graefe in 1866 and later named by Donald M. Gass(1). It appears as a well-delimited serous detachment of the neurosensory retina in the posterior pole due to focal or diffuse leakage of fluid from choroidal vessels through the retinal pigment epithelium (RPE)(1-2).
Although the pathogenesis of CSC is still under debate and the precise physiopathological events involved remain unknown, it is believed that stasis, ischemia, or inflammation in the choroid (or a combination of these factors) may lead to abnormal permeability with an eventual rupture of the outer blood-retinal barrier, with con se quent serous retinal detachment and small areas of RPE elevation(3).
The current understanding of the pathogenesis of CSC suggests the involvement of the choroid. Primary evidence of choroidal hyperpermeability has been provided by the staining of the inner choroid seen on mid-phase indocyanine green (ICG) angiography(4). Studies in rabbit eyes have shown that focal da ma ge to the choriocapillaris and RPE resulted in serous detachment(5). Experimental models of CSC have been produced by the intras cle ral injection of indomethacin and repeated injections of epinephrine(6). These models provide evidence that stress plays a role in causing a change in focal permeability in the choriocapilla ris. The primary role of the choroid is further supported by the enhanced depth imaging (EDI) optical coherence tomography (OCT) findings(7). Hyperpermeable choroidal vessels are thought to increase tissue hydrostatic pressure, promoting the formation of RPE detachments, overwhelming the barrier function of the RPE, and leading to areas of fluid accumulation between the retina and the RPE. Not all areas of choroidal staining are associated with RPE leaks, suggesting that, in some instances, the RPE may be able to withstand the stresses posed by choroidal disease. CSC may result from impaired choroidal vascular autoregulation induced by steroids, catecholamines, or sympathomimetic agents. Elevated serum levels in CSC of plasminogen activator inhibitor-1, an inhibitor of physiologic fibrinolysis, have led to suggestions that there may be a thrombotic mechanism for these vascular changes(8). CSC more commonly affects middle-aged men (aged 30-50 years). The risk factors are stress and type A personality, with the condition usually having an acute course. In around 5% of patients, visual function may be compromised due to progression to chronicity and RPE involvement (secondary epitheliopathy). When there is involvement of the central macula, the patients report the sudden onset of low visual acuity, micropsia, metamorphopsia, and central or paracentral scotoma(9). Other risk factors related to the disease includerace, high systemic arterial pressure, and abnormal steroid regulation (idiopathicor from a history of corticoid use, Cushing syndrome, or steroid-producing tumors)(10). Although rare, the most serious complication of CSC is the development of choroid neovascularization. This usually affects patients aged 40-50 years and is a serious threat to vision. There have also been reports of an association with Helicobacter pylori and with a predisposing genetic condition(11).
Clarification of the pathological process of CSC became possible after the invention of fluorescein and ICG in the second half of the 20th century(12). Maumenee described the characteristic findings with angiofluorescein leakage, which revealed that the choroid and RPE were the primary tissues involved(13). Gass characterized the angiography findings and named the condition central serous choroid retinopathy(2).
Fluorescein angiography (FA) is the imaging technique most extensively used to diagnose CSC. A "chimney smoke leakage" is the classical angiographic characteristic reported and is observed in 25% of CSC cases(14). Although it is possible to use FA to clinically investigate the existence of any choroidal abnormality, it may fail to detect such abormalities(15). Fluorescein leaks rapidly through the choriocapillaris layer, blurring the anatomy of the choroid; furthermore, 59%-75% of the choroid fluorescein is absorbed by the RPE and so is of no use for the investigation of diseases of the choroid(16-17).
ICG is a dye that has advantages over fluorescein regarding the choroidal circulation. Protein-bound ICG passes slowly through the fenestrations of the choroid, revealing the circulation of the choroid and its abnormalities. The fluorescent dye absorbs and reflects light close to the infrared, improving the visualization by fluorescence in areas of exudates, hemorrhages, and ocular pigment, thus pro viding a better assessment of the choroid(17).
Although it is recognized that there are differences between the two diagnostic methods for the assessment of CSC, to date there has been no report of a large clinical trial showing the advantages of one method over the other with regard to CSC(18). The objective of the present study was therefore to compare the findings of FA, ICG an giography, and OCT used simultaneously in patients with chronic CSC.
METHODS
This case study included ten consecutive patients with a defined diagnosis of chronic CSC that affected one or both eyes, who underwent multimodal assessment that included FA, ICG angiography, and OCT. Chronic evolution was characterized by a history of more than six months duration or recurrence of the condition(11). The study population consisted of patients who were being followed up at the Retina and Vitreous Outpatient Clinic of HC-RP and who were evaluated from July to August 2013. The patients provided written informed consent prior to undergoing the examinations and the study was conducted in accordance with the principles of the Declaration of Helsinki. The study was approved by our hospital's institutional review board.
Inclusion criteria were a defined diagnosis of chronic CSC (with an evolution of more than 6 months or recurrence) and agreement to undergo FA and ICG angiography examinations simultaneously.Exclusion criteria were a history of allergy to dyes or crustaceans, any condition that would prevent an appropriate observation of the posterior pole, and having received cataract surgery or vitrectomy within 3 months prior to the study.
The patients included in the study received a complete ophthalmologic examination with corrected visual acuity before undergoing the FA and ICG examinations, which were performed using high-resolution angiography coupled to OCT (Spectralis HRA-OCT, Heidelberg Engineering, Heidelberg, Germany). This permitted the simultaneous execution of angiography with fluorescein and ICG. Peripheral venous access to an upper limb was obtained for the sequential infusion of the dyes. The patients were evaluated during three phases of the examination:early (up to 4 min), intermediate (4-8 min), and late (after 8 min). Changes such as hyperfluorescence (caused by transmission, impregnation, or pooling) and hypofluorescence (caused by a blockade or defect of vascular filling) were assessed in each patient during the examination with each dye.During the intervals in the image capture of the dyes, OCT was performed with high-definition images in the areas where changes in fluorescence were observed. After the procedure, the patients were asked to wait for 20 min before discharge to exclude the possibility of allergic reactions to the dyes.
RESULTS
The study included 10 patients and a total of 19 eyes. Only one patient did not have bilateral disease. Bilateral disease was detected by evidence of the already documented subretinal fluid or by the presence of pigment epithelial detachment or RPE changes. Seven patients (70%) were men and 3 (30%) were women. The mean age was 50.7 ± 8.4 years (range: 38-66 years) and the mean duration of monitoring a tour hospital was 14 months. The mean corrected visual acuity of the 19 eyes was20/25 on the Snellen scale (Table 1).
Table 1 Demographic data for the patients with chronic central serous chorioretinopathy
| Patients | Sex | Age | Visual acuity ** |
|---|---|---|---|
| 1 | M | 60 | 1.0/1.0 |
| 2 | F | 43 | 0.8/1.0 |
| 3* | M | 42 | 0.32 |
| 4 | M | 47 | 1.0/0.32 |
| 5 | M | 47 | 1.0/1.0 |
| 6 | M | 66 | 1.0/0.4 |
| 7 | M | 52 | 0.8/0.5 |
| 8 | M | 56 | 1.0/0.8 |
| 9 | F | 56 | 0.8/1.0 |
| 10 | F | 38 | 0.8/1.0 |
*the patient showed alteration only in the left eye.
**right eye/left eye on the Snellen table.
Early phase (up to 4 min)
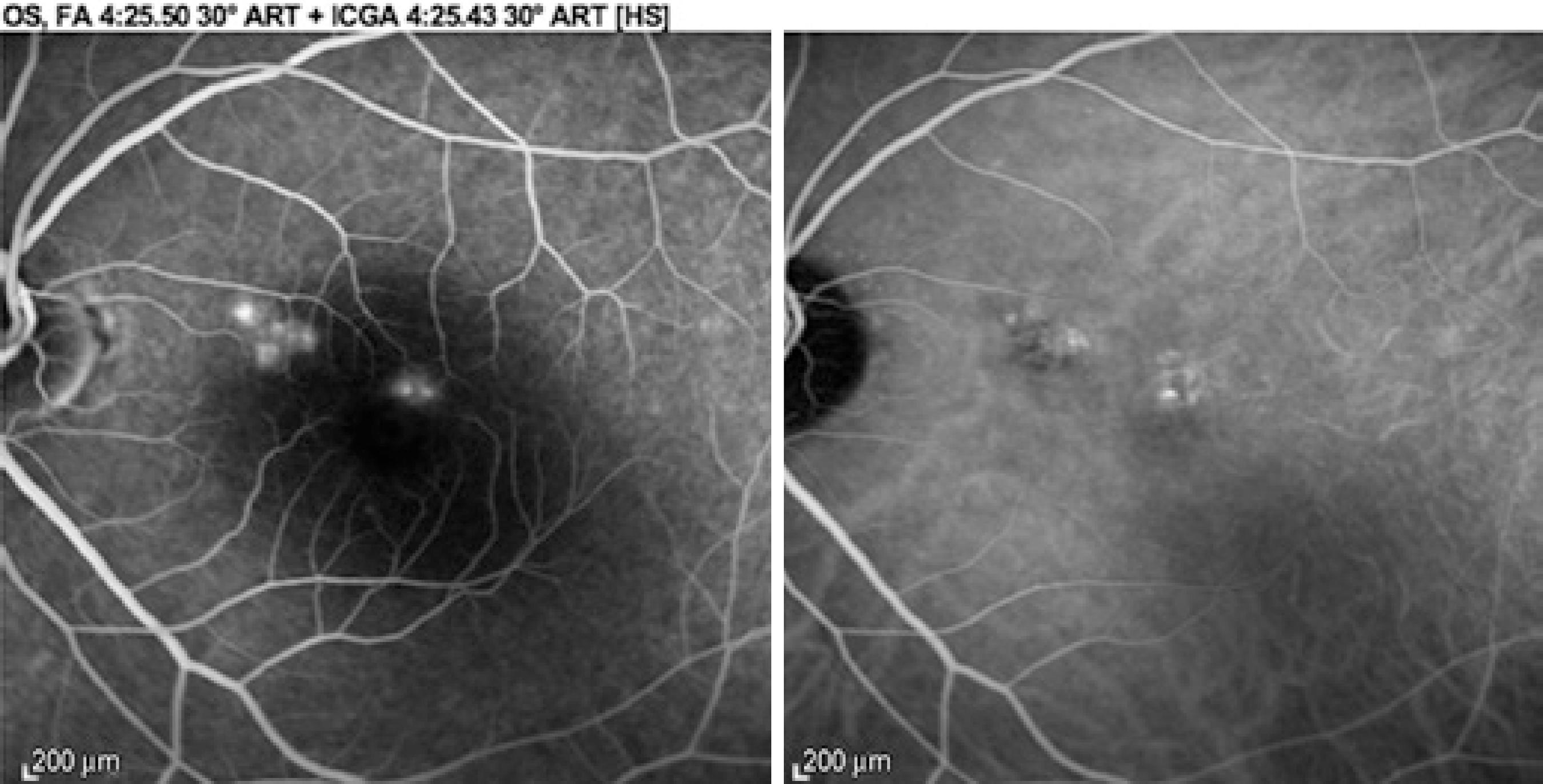
Abnormal areas in all 19 eyes studied (100%) could be observed on FA, represented by hyperfluorescent areas due to increased transmission of the normal choroidal fluorescence, indicating RPE atrophy, as well as areas with early staining. Digital angiography with ICG revealed abnormal areas in 17 of the 19 eyes. Hyperfluorescence (demonstrating impaired choroid permeability due to hyper permeability) and areas with hypofluorescence of irregular choroidal perfusion due to a probable filling deficit were observed. In the two cases in which no abnormality was observed on ICG angiography, several hyperfluorescent points were observed on FA, characterizing a window defect (Figure 1). Another difference observed was that areas of ICG hyperfluorescence did not correspond to areas of FA hyperfluorescence in 12 (70%) of the 17 eyes in which ICG demonstrated alteration (Figure 2).
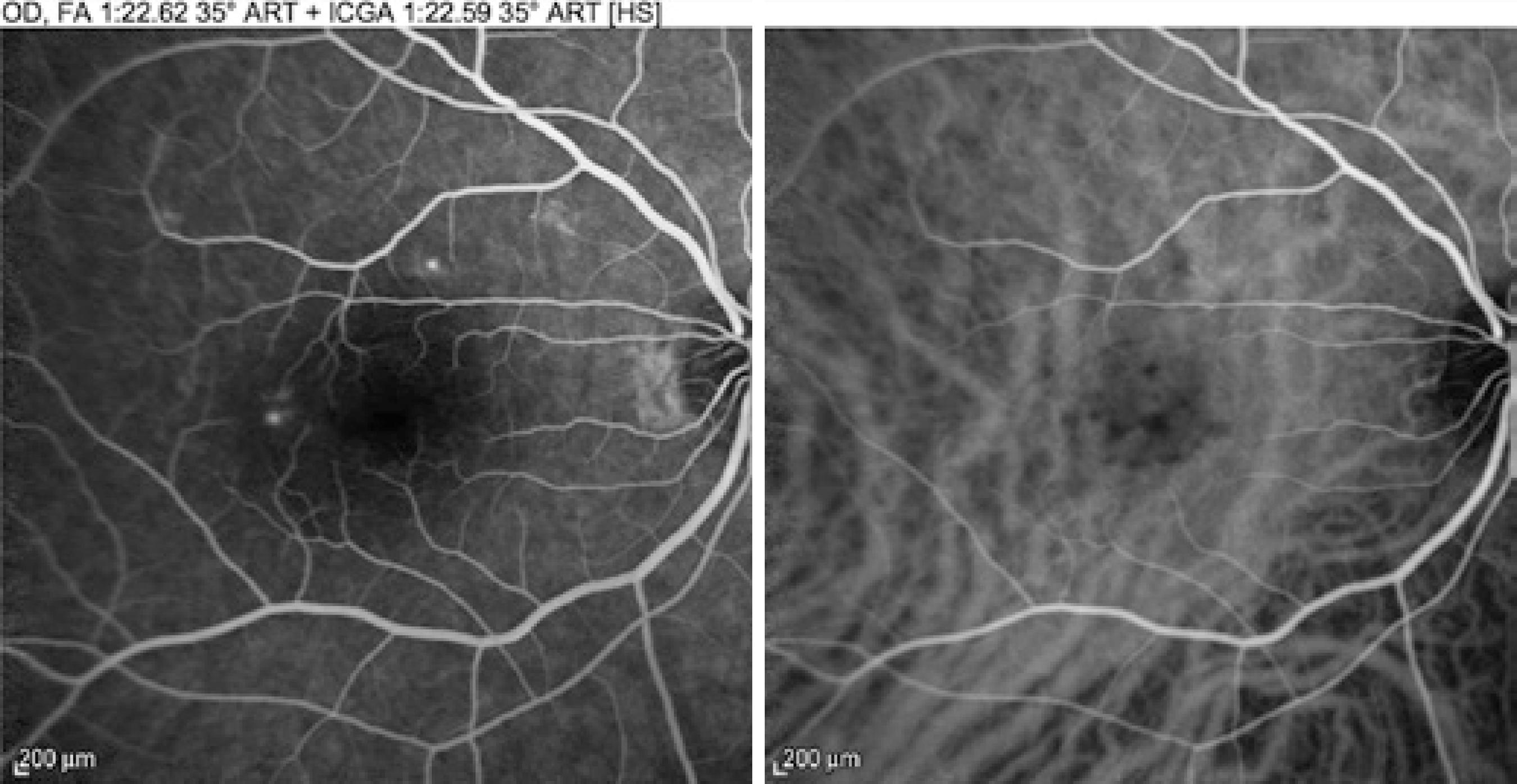
Figure 1 Early phase images showing hyperfluorescent areas on fluorescein angiography (left) that were not demonstrated during the early phase of indocyanine green angiography (right).
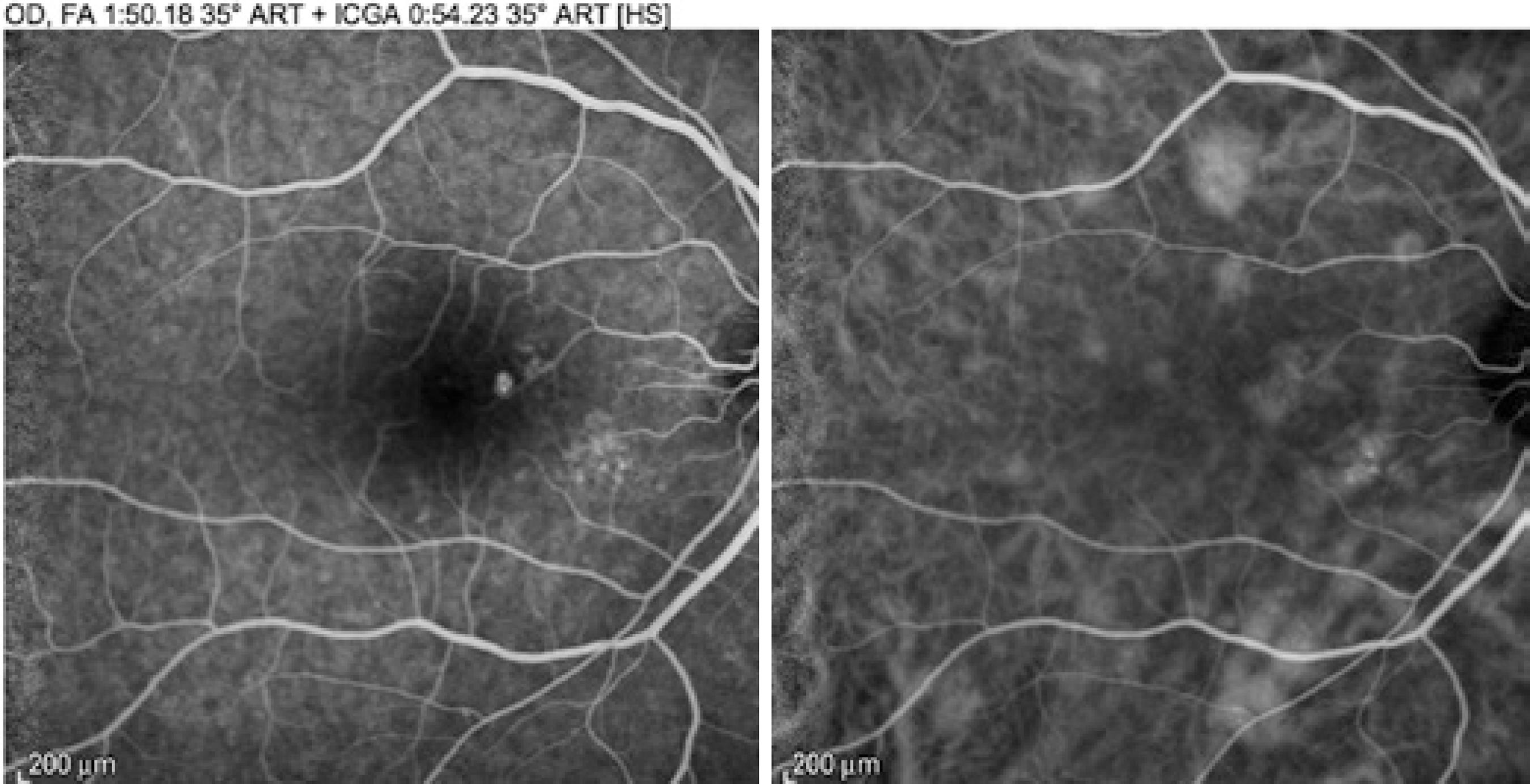
Figure 2 Early phase images of the examinations showing changes in fluorescein angiography (left) and indocyanine green angiography (right). A large number of areas of hyperfluorescence that did not appear in the fluorescein angiography were demonstrated in theindocyanine green angiography, suggesting increased choroidal permeability.
Intermediate phase (4-8 min)
All patients showed changes on both FA and ICG angiography. Hyperfluorescent areas due to a window defect, staining, and accumulation were more evident and better characterized on FA. However, the ICG angiography was clearer and also revealed areas not coincident with FA (Figure 3).
Late phase (after 8 min)
FA maintained distribution patterns closely similar to those of the intermediate phase, only delimiting less intensely areas of window defect and maintaining hyperfluorescence in areas of dye staining or pooling. Pathological RPE zones localization was heterogeneously distributed with no greater prevalence of lesions in any quadrant. ICG also revealed an attenuation of fluorescence in the areas showing changes.
Optical coherence tomography
The OCT was guided by the changes in FA and ICG angiography. Normal areas on FA corresponding with areas of choroidal hyperpermeability observed on ICG angiography were shown on OCT to have normal RPE (Figure 4). Hyperfluorescent areas on both FA and ICG showed the presence on OCT of an irregular RPE with slight pigment epithelium detachment and opaque content (Figure 5).
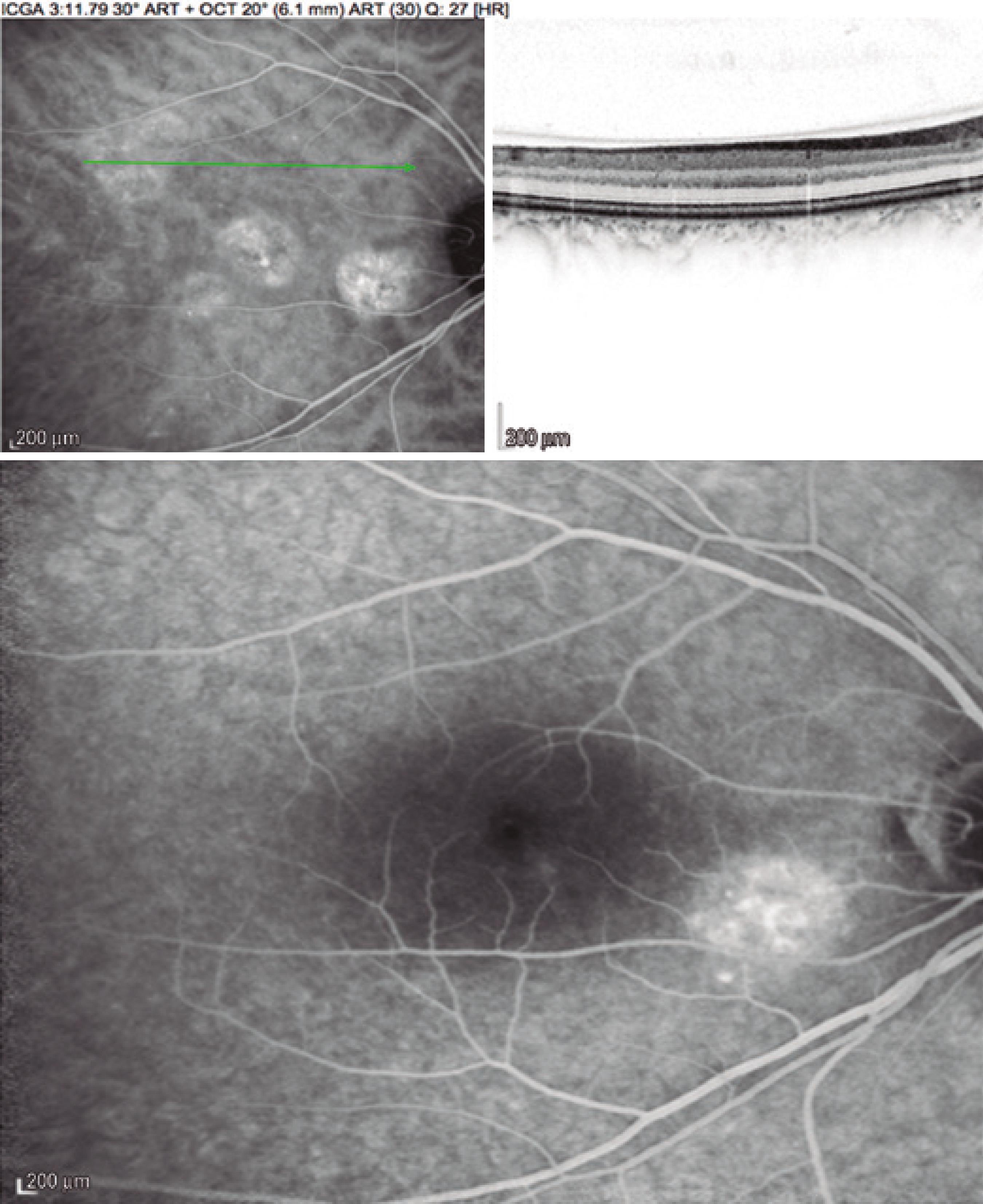
Figure 4 Optical coherence tomography image (top right) of a non-coincident area that demonstratedretinal pigment epithelium integrity in a normal area on fluores cein angiography (bottom) and changes in permeability on indocyanine green an giography (top left).
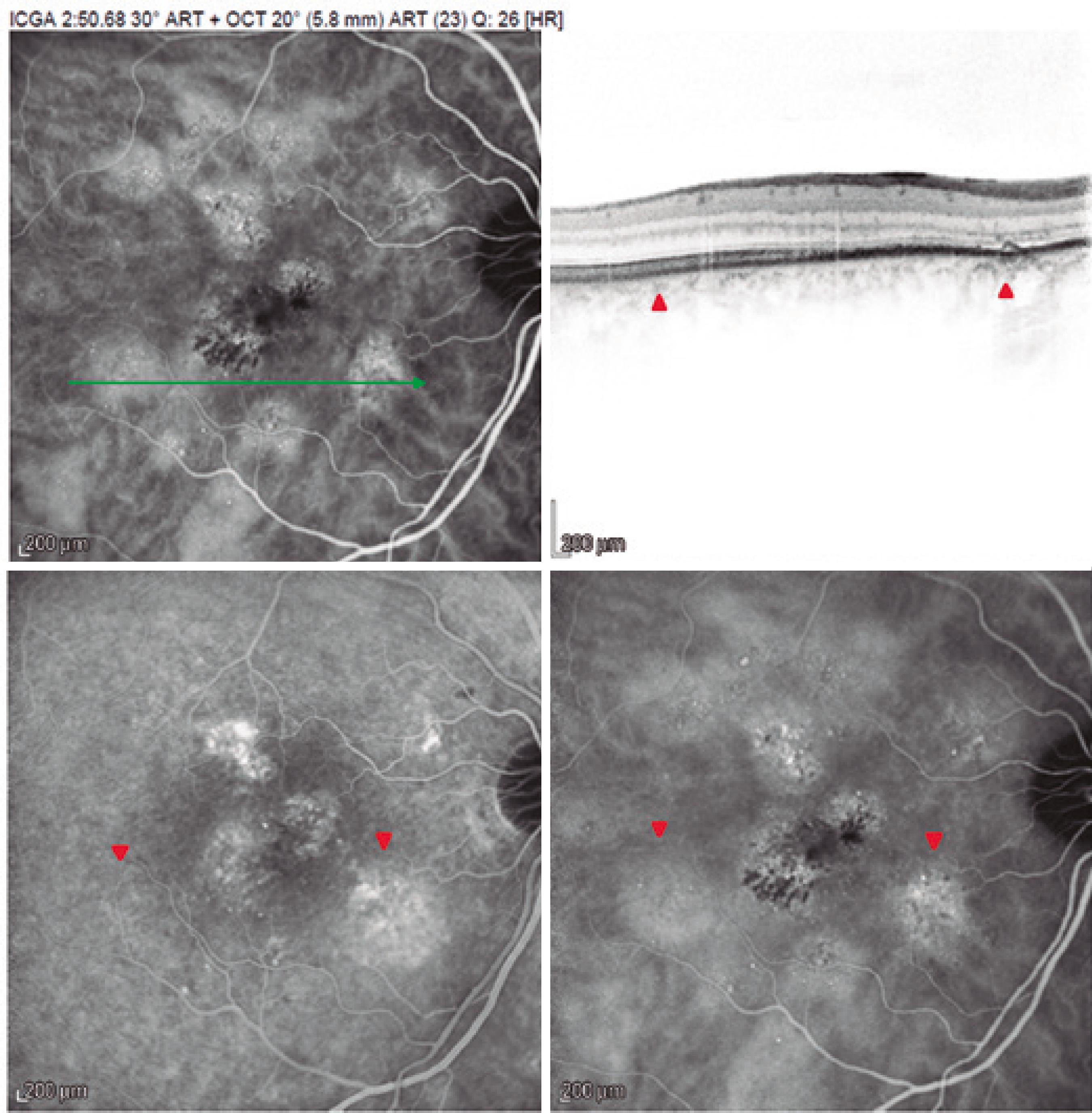
Figure 5 Images demonstrating that areas with altered fluorescence on fluorescein angiography (bottom left) and indocyanine green angiography (bottom right). Section of an hyperpermeability area (top left, green line) showed changes in the retinal pigment epithelium on optical coherence tomography (top right, arrows). A non-coincident area in the same section (arrowheads) showed no changes in the retinal pigment epithelium, whereas indocyanine green angiography showed hyperpermeability.
DISCUSSION
CSC remains controversial, with questions remaining about its pathogenesis and treatment. Imaging procedures such as FA and ICG angiography therefore play an important role in the diagnosis of CSC and in understanding its pathophysiology. They are tools that can help with the management of the disease(19).
In the present study, we assessed 19 eyes of 10 patients. The male/female ratio was 2.33/1, similar to ratios observed in previous studies. For example, the ratio was 4.50/1 in a series of 22 cases(20), 2.64/1 in a series of 51 cases(21), and 2.33/1 in a series of 87 patients (in Brazil)(22). The mean visual acuity in the 19 affected eyes was 20/25 on the Snellen chart, similar to the mean values of best corrected visual acuity (both 20/32) of two other studies of chronic CSC(16,23).
The assessment of changes in FA and ICG angiographs is already routined in studies of chronic CSC, but the simultaneous application of both methods to the same patient has not been previously reported.
In the present study, the frequency of hyperpermeability diagnosed by ICG angiography was 100%, compared with 63%-100% in earlier studies(16). It should be emphasized, however, that this 100% frequency was detected with a procedure that lasted, on average, more than 5 minutes, demonstrating the importance of allowing the procedure enough time for the evaluation to avoid the potential underestimation of some changes(23).
Yannuzzi reported that chronic CSC can be focal or multifocal, with clearly visible leakage on FA and ICG angiography. He also observed that it was more commonly persistent with exudative neu rosensory retinal detachment that resulted from a state of zonal or diffuse RPE hyperpermeability with the accumulation of fluid from the choroid in the subretinal space, with passage through abnormal RPE junctions(24). Other causes of hyperfluorescence include RPE atrophy-inducing transmitted hyperfluorescence secondary to RPE depigmentation that arises from the chronic aggression caused by the presence of subretinal fluid. Classical alterations with hyperfluorescence are described as "chimney smoke" and "ink spots"; both are related toCSC, with the lattermore prevalent in chronic cases(25-26). In addition, a chronic change in RPE can lead to focal areas of hypofluorescence caused by blockade due to the accumulation of pigments that alternate with areas of depigmentation (the window defect)(14).
The multimodal imaging of the present study revealed differences in areas of fluorescence change. FA revealed hyperfluorescent areas earlier. Although digital angiography with ICG took more time to determine the areas of hyperfluorescence, it demonstrated other points that were not found with FA. Most of the hyperfluorescences revealed by ICG involved areas with choroidal hyperpermeability observed in the late phases of the procedure, as was also reported by Tsujikawa et al.(27), demonstrating the importance of these points in the evaluation of CSC, with its physiopathology linked to hyperpermeability. The identification of these areas can be of fundamental importance for planning treatment with therapeutic modalities such as micropulse laser treatment and photodynamic therapy(28).
The images captured by OCT during the simultaneous assessment of the two dyes allowed the observation of tomographic sections in non-coincident areas of fluorescence abnormalities, showing the importance of using indocyanine in the late phases and OCT in the corresponding areas for monitoring purposes. This procedure demonstrated that RPE integrity was maintained in the areas in which ICG hyperfluorescence did not coincide with FA. However, areas showing hyperfluorescence in the two modalities demonstrated RPE abnormalities identified by OCT in these regions(29), confirming the importance of OCT for the assessment of CSC(30).
CONCLUSION
Although it has been shown that FA and ICG angiography both have a good capacity for detecting RPE changes and activity in chronic CSC, ICG can be more efficient by revealing areas of choroidal hyperfluorescence; it therefore represents a good method for the prediction of future RPE injuries, with OCT also being a good method for confirming these changes. Multimodal imaging with FA, ICG angiography, and OCT permits the differentiation of areas with clinically significant changes in the RPE (shown by altered areas on both FA and ICG) from areas that, although they show changes in choroidal permeability demonstrated by ICG, still do not show changes in RPE (as visualized on OCT) and are considered to be normal on FA. A prospective study with a larger number of patients and a long follow-up period is necessary for establishing a better understanding of the pathogenesis of CSC.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

