INTRODUCTION
Cataracts are one of the most common complications of many forms of uveitis, with a reported incidence of up to 50%(1-3). Uveitis is primarily related to intraocular inflammation and can be secondary to the administration of corticosteroids(1,3). Phacoemulsification with simultaneous intraocular lens (IOL) implantation is the standard method of cataract surgery for patients with uveitis(2-4). High rates of postoperative complications and recurrence of inflammation are observed in patients with uveitis(2,4,5). Careful preoperative management, with skillfully performed surgery and thorough postoperative control, are essential for better results in these particularly challenging cases(1).
In this study, we evaluated the outcomes of phacoemulsification and IOL implantation in patients with uveitis and cataracts at a tertiary center in Brazil.
METHODS
The clinical records of 38 consecutive patients (45 eyes) with uveitic cataracts who underwent phacoemulsification and acrylic IOL implantation (Alcon IOL model MA 30 AC, Alcon Laboratories, Fort Worth, Texas, USA) during the period from June 2007 through January 2012 were retrospectively reviewed. Surgery was performed at the Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP, Brazil. The study was approved by the Institutional Ethics Committee (protocol CAPPesq #0262/11) and informed written consent was obtained from all patients prior to inclusion.
Before surgery, a complete uveitis-oriented history was obtained and ophthalmic and systemic work-ups were conducted for all patients. Laboratory tests included a full blood cell count, tests for renal and liver function, fasting blood glucose level, rheumatoid factor, antinuclear antibody, Treponema pallidum fluorescent antibodies, Toxoplasma gondii antibodies, herpes simplex type 1 and 2 virus and varicella zoster virus antibodies, human immunodeficiency virus antibodies, human T-lymphotropic virus type 1 antibodies, chest X-ray and computed tomography of the chest, when recommended, and a tuberculosis skin test. Data collected included gender, age at surgery, uveitis etiology, preoperative findings, period of inactive intraocular inflammation before surgery, follow-up period, and intrao perative and postoperative complications. A minimum of 3 months of complete preoperative control of inflammation was observed in all patients. Postoperative complications included recurrence or persistence of inflammation (for >6 months) after surgery, posterior synechiae, pupillary capture of the IOL, an increase in intraocular pressure (IOP) measured by applanation tonometry of over 21 mmHg within 1 month of surgery that required treatment, posterior capsule opacification that required neodymium-doped yttrium aluminum garnet (Ng:YAG) laser capsulotomy, postoperative cystoid macular edema, bullous fkeratopathy, and IOL explantation. Best corrected visual acuity (BCVA) analysis included the immediate preoperative visual acuity and 1-year postoperative visual acuity. Anterior chamber cells were graded according to the Standardization of Uveitis Nomenclature Working Group criteria(6).
Surgery was performed by two surgeons (F.T.S. and P.C.C.). Dilation was achieved with instillation of 1% tropicamide and 10% phenylephrine eye drops every 15 minutes, starting 1 hour before surgery. Either retrobulbar (Naropin®, AstraZeneca do Brasil) or to pical (Anestalcon®, Alcon Laboratórios do Brasil) anesthesia was admi nistered according to the surgeons' judgment (e.g., according to the difficultly of each case and patients' profiles). The eye was accessed with a 2.75 mm clear corneal incision along with a 15º sideport paracentesis, with an angle of 60º between the two. Small pupils were managed by synechialysis consisting of sequential anterior chamber expansion with a viscoelastic agent (Viscoat®, Alcon Laboratories, Randburg, South Africa), careful lysis of irido-phakic adhesions with an iris spatula, and finally, iris stretch utilizing Y- and H-hooks as needed. Upon subsequent completion of continuous curvilinear capsulorhexis, the lens material was removed by phacoemulsification using the phaco-chop technique (Infiniti with Ozil® phacoemulsifier, Alcon Laboratories, Fort Worth, Texas, USA). Cortex was aspirated with a coaxial automated irrigation-aspiration device (Ultraflow I/A, Alcon Laboratories, Fort Worth, Texas, USA). With the aid of an ophthalmic viscosurgical device (Viscoat®, Alcon, Randburg, South Africa), an acrylic three-piece IOL (Alcon IOL model MA 30 AC, Alcon Laboratories, Fort Worth, Texas, USA) was implanted in the capsular bag and the incisions were checked for closure, exceptionally requiring 10-0 nylon suturing (Nylon 10-0, Ethicon, Somerville, New Jersey, USA). Upon completion of the surgery, 0.5% moxifloxacin (Vigamox, Alcon Laboratórios do Brasil, Brazil) and 1% prednisolone acetate (Pred-fort, Allergan Produtos Farmacêuticos Ltda, São Paulo, Brazil) were administered.
Postoperative care included topical 0.5% moxifloxacin four times daily, and topical 1% prednisolone acetate every 4 hours for the first and second week, every 6 hours for the third week, and thereafter according to the intensity of the anterior chamber reaction. 1% tropicamide was administered topically once daily for 2-3 months. Patients receiving systemic immunosuppressants before cataract surgery maintained their dosages at the same levels. Oral prednisone (0.5 mg/kg/day) were administered to patients with noninfectious uveitis for 3 days prior to surgery.
Patients were seen on the first and seventh postoperative days. They were then seen every other week for 1 month, and every 2 months thereafter. At each postoperative visit, BCVA, IOP, anterior chamber reaction, vitreous haze, and retinal lesions were evaluated. If severe inflammatory episodes occurred, patients were given systemic corticosteroids and/or immunosuppressants.
Visual acuity was measured using a decimal chart. Differences in preoperative and postoperative visual acuity were tested for statistical significance using the Wilcoxon related test. A p value of less than 0.05 was considered statistically significant. Statistical analysis was performed using SPSS 15.0 (SPSS Science, Chicago, Illinois, USA).
RESULTS
The mean age of the 15 men and 23 women was 52.1 ± 12.5 years (range, 20 to 79 years). The mean follow-up after surgery was 19.4 ± 10.6 months (range, 12 to 53 months).
The demographic and clinical characteristics of the subjects included are shown in table 1. The most frequent diagnosis was Vogt-Koyanagi-Harada disease (9 eyes). The mean duration of disease was 130.2 ± 134.7 months (range, 24 to 636 months). The mean period of inflammation control before surgery was 20.1 ± 18.4 months (range, 3 to 100 months). Thirteen eyes (28.9%) had posterior synechiae in three or more quadrants. Nineteen eyes (42.2%) had total cataracts, seven (15.5%) of which were intumescent(4). Surgery was indicated in order to either improve visual function (n=39; 86.7%) or to better visualize the posterior segment (n=6; 13.3%). In-the-bag acrylic IOL implantation was achieved in all eyes. Posterior capsular rupture occurred in one eye of a patient with sclerouveitis associated with relapsing polychondritis; however, it was still possible to place the lens in the bag. All patients received postoperative eye drops as previously described.
Table 1 Demographic and clinical characteristics of patients with uveitis and cataracts
| Description | |
|---|---|
| N, patients (eyes) | 38 (45.0) |
| Age, mean ± standard deviation (range) (years) | 52.1 ± 12.5 (20-79) |
| Gender, female (%) | 23 (60.5) |
| Race | |
| White (%) | 25 (65.8) |
| Non-white (%) | 13 (34.2) |
| Uveitis duration, mean (range) (months) | 130.2 (24-636) |
| Postoperative follow-up duration, mean (range) (months) | 019.4 (12-530) |
| Bilaterality | |
| Right eye | 11 |
| Left eye | 20 |
| Both eyes | 07 |
| Uveitis etiologic classification | |
| Infectious, patients (eyes) | 12 (13.0) |
| Toxoplasmosis | 06 (06.0) |
| Presumed tuberculosis | 03 (04.0) |
| Syphilis | 02 (02.0) |
| Human immunodeficiency virus | 01 (01.0) |
| Non-infectious, patients (eyes) | 26 (32.0) |
| Vogt-KoyanagiHarada disease | 05 (09.0) |
| Sympathetic ophthalmia | 03 (03.0) |
| Behçet’s disease | 02 (02.0) |
| Multifocal choroiditis | 01 (01.0) |
| Posner-Schlossman syndrome | 01 (02.0) |
| Fuchs’ heterochromic iridocyclitis | 04 (04.0) |
| Ankylosing spondylitis | 01 (01.0) |
| Psoriasis | 01 (01.0) |
| Relapsing polychondritis | 01 (01.0) |
| Systemic lupus erythematosus | 02 (02.0) |
| Other connective tissue disease | 01 (01.0) |
| Sarcoidosis | 01 (01.0) |
| Idiopathic | 03 (04.0) |
| Visual acuity, eyes (%) | |
| Preoperative | |
| ≤0.1 | 40 (88.8) |
| Postoperative (12 months) | |
| ≥0.5 | 28 (62.2) |
| >0.1–≤0.4 | 10 (22.2) |
| ≤0.1 | 07 (15.5) |
A comparison of preoperative and postoperative BCVAs is shown in figure 1. The median BCVA was 0.01 (range, to 0.001 to 0.4) preoperatively and 1.00 (range, 0.001-1) postoperatively (p=0.001).
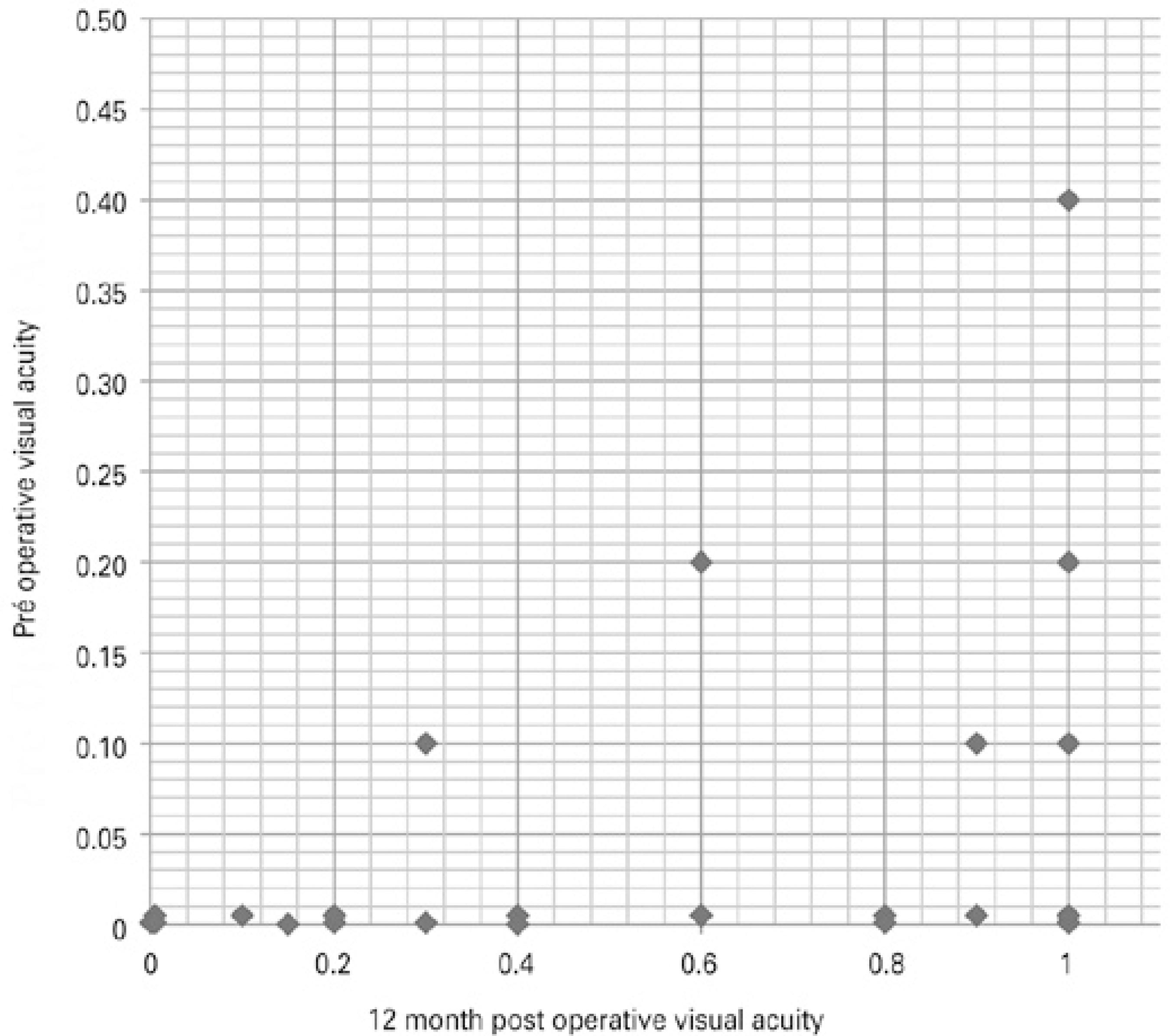
Figure 1 Comparison of preoperative and 1-year postoperative best corrected visual acuity of patients with uveitis and cataracts who underwent phacoemulsification
Before surgery, only 20% of the patients had a BCVA of 0.1 or better. After surgery, at the 6-month visit, 86.7% of the patients had a BCVA of 0.1 or better, 62.2% had a BCVA of 0.5 or better, and 55.6% had a BCVA of 0.8 or better. At the 12-month visit, a BCVA of 0.1 or better was observed in 86.7% of the patients; a BCVA of 0.5 or better was seen in 62.2% of the patients; and 53.3% of the patients had a BCVA of 0.8 or better.
At the 1-year follow-up, the visual acuity of 38 eyes (84.4%) had improved by two or more lines. Seven (15.5%) eyes did not gain or lose lines Table 1, among which six eyes had previous macular abnormalities such as retinal detachment (toxoplasmosis), foveal scarring and/or subretinal fibrosis (Behçet's disease, multifocal choroiditis, presumed ocular tuberculosis), optic disk atrophy (Behçet's disease), and choroidal neovascular membrane (sympathetic ophthalmia).
Posterior capsule opacification was observed in 10 eyes (22.2%) during the first year of follow-up. Persistent postoperative inflammation (for >6 months) was observed in seven eyes (15.5%), and uveitis recurrence occurred in four eyes (8.8%) due to Posner-Schlossman syndrome (n=1), Vogt-Koyanagi-Harada disease (n=1), sympathetic ophthalmia (n=3), Fuchs' heterochromic iridocyclitis (n=2), tuberculosis (n=2), and unknown causes (n=2). The IOL was explanted from one eye with Posner-Schlossman syndrome 2 months after surgery due to intense inflammation and glaucoma. This eye developed postoperative bullous pseudophakic keratopathy. Intraocular hypertension was observed in six eyes (14%).
DISCUSSION
Cataracts are a major cause of vision loss in patients with uveitis(1-3). The clinical outcomes in these patients are directly related to the type and cause of uveitis. Careful preoperative evaluation and adequate intraoperative and postoperative management affect the visual outcomes of cataract surgery(1-5). In this retrospective case se ries of complicated cataract extraction, 38 eyes (84.4%) had improved visual acuity after surgery at the 1-year evaluation. Despite this fa vorable outcome, persistence and recurrence of inflammation were observed in 11 eyes (24.4%), and the prolonged use of corticosteroids and immunosuppressants was needed in these patients.
In this report, the main causes of infectious uveitis were toxoplasmosis and presumed ocular tuberculosis. The main causes of noninfectious uveitis were Vogt-Koyanagi-Harada disease, sympathetic ophthalmia, and Fuchs' heterochromic iridocyclitis(1,2).
An appropriate diagnostic workup and meticulous preoperative care are crucial for successful surgery(1,5). A minimum of 3 months of complete preoperative control of inflammation was observed in all patients. The adequate control of preoperative inflammation is necessary for reducing the risk of postoperative chronic macular edema and for ensuring minimal postoperative inflammation. Several protocols for achieving this have been proposed, such as administering oral steroids at 1 mg/kg per day, starting 3 days or up to 1 week before surgery, with or without topical steroids 6 to 8 times per day(3,5,6). In the present study, oral prednisone (0.5 mg/kg/day), starting 3 days before surgery, was used in non-infectious uveitis, and in patients already taking oral steroids, the dose was maintained, as suggested by Ram et al.(7). Preoperative antibiotic prophylaxis of surgically induced inflammation was not conducted for any patients with infectious uveitis. Interestingly, no reactivation was observed during follow-up of these patients, although some authors have previously suggested that there is an increased risk of reactivation of ocular toxoplasmosis following cataract surgery and have suggested the use of prophylactic antibiotics in the perioperative period(3,8).
Regarding intraoperative considerations, when synechialysis prior to phacoemulsification was needed, this was assisted with the use of an irrigation cannula, iris spatula, and Y- and X-hooks, as needed. None of the subjects required iridotomy, iris hooks, or the use of a Malyugin ring. Minor sphincterotomies were employed when there was fibrosis of the pupillary rim. For better results in capsular visualiza tion, trypan blue was injected under the iris and into the anterior chamber prior to viscoelastic injection. In some patients, altered elas ticity and rigidity of the anterior capsule during capsulorhexis was observed, suggesting tissue changes due to inflammation and/or chronic corticosteroid use(9). Previous studies comparing different types of IOLs in patients with complicated cataracts consistently demonstrated that acrylic IOLs led to the least postoperative inflammation(10). Therefore, acrylic three-piece IOLs were implanted in all patients in this study. All lenses were successfully placed in the bag following the recommendations of several other studies establishing this as the ideal method(2).
Intraoperative medications can also be used to prevent significant postoperative inflammation in patients with uveitis. In addition to prophylactic oral steroids before the procedure, some authors have suggested the addition of a large dose of intravenous methylprednisolone at the time of surgery, or administration of preservative-free intraocular steroids into the anterior chamber or intravitreal at the end of cataract surgery or fluocinolone acetonide implantation(11-13). In our cases, no adjunctive anti-inflammatory intraocular therapy was instituted at the time of surgery. Oral steroids were maintained in the postoperative period and tapered according to response for the sake of better control of side effects.
Postoperative management included topical antibiotics and corticosteroids. The severity of the ocular inflammatory disease guided tapering of the topical steroids in the immediate postoperative course. The most common topical medication used was 1% prednisolone acetate ophthalmic solution(5). Persistent postoperative inflammation in patients with uveitis should raise suspicion about the recurrence of inflammation, chronic low-grade infection-related inflammation, and/or other infectious and non-infectious etiologies. In the present study, 81.8% of the eyes that had persistent or recurrent inflammation had non-infectious uveitis, and an increase in immunosuppressive treatment led to a favorable response. Nevertheless, one patient with Posner-Schlossman syndrome had their IOL explanted due to intense inflammation and an increase in IOP. Foster et al. pointed out that one of the most common causes of intraocular lens removal was chronic low-grade inflammation with poor response to treatment and, after removal of the lens, visual acuity improved or stabilized in most cases(14). In our case, the aqueous humor, as well as the explanted material, was submitted for microbiological analysis; no pathogen was isolated. High doses of oral steroids alongside immunosuppressive therapy controlled the ocular inflammation.
In this study, a low incidence of postoperative ocular hypertension was observed. Roesel et al. compared the outcomes of cataract surgery in patients with chronic non-infectious uveitis who were given either orbital floor triamcinolone acetonide or oral prednisolone(13). The authors observed that up to 12% of patients in the first group and 28% in the second group developed IOP elevation. A meta-analysis of intraocular pressure monitoring after administration of intravitreal steroids found that 32% of individuals developed ocular hypertension following 4 mg intravitreal triamcinolone administration(15). As such, the current study raises the question of whether adjunctive intravitreal and/or periocular triamcinolone acetonide injection should be systematically employed for the control of posto perative inflammation.
The majority of patients with poor postoperative visual acuity (≤0.1; n=6; 85.7%) had previous macular abnormalities such as retinal detachment, foveal scarring, subretinal fibrosis, and choroidal neovascular membrane. The remaining patient developed postoperative bullous keratopathy.
Despite the limited number of patients and the retrospective design of this study, we showed that careful planning of cataract surgery, independent of the etiology of the uveitis, and a systematic follow-up, makes it easier to identify pre- and postoperative inflammation, allowing a prompt intervention and a better outcome.
In conclusion, cataract surgery was successful in the patients with uveitis in this study. In the majority of cases (86.6% of eyes) a gain in visual acuity of two or more lines was achieved. Several authors have previously described favorable outcomes from surgery for complicated cataracts. This report further reinforces the importance of strict control of preoperative inflammation, meticulous surgery, in-the-bag IOL implantation, and vigilant postoperative care. The main causes of final low visual acuity were related to posterior segment abnormalities(16-20).
WHAT WAS KNOWN
Phacoemulsification with acrylic in-the-bag IOL implantation is the current standard of care for most patients with complicated cataracts.
Higher rates of postoperative complications and recurrence of inflammation are observed in patients with uveitis than in those without uveitis.
Strict control of preoperative inflammation ensures favorable postoperative outcomes.
WHAT THIS PAPER ADDS
The profiles of Brazilian patients with complicated cataracts undergoing phacoemulsification and IOL implantation at a te r tiary center are outlined.
This study demonstrates that visual outcomes are overall comparable to previous case series from centers elsewhere.
A low incidence of postoperative ocular hypertension was observed.
Macular scarring was the cause of poor postoperative visual outcomes.
The results also suggest that meticulous tapering and adjustment of oral prednisone (switching to immunosuppressants, antimetabolites, or biological agents as needed) may provide optimal control of postoperative inflammation in conjunction with minimal side effects




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

