CASE REPORT
A 21-year-old female presented with decreased vision in her right eye (OD), which already had a low vision, for the past 4 days. She had undergone several surgeries in both eyes because of congenital glaucoma and had lost light perception in her left eye (OS) several years prior. For treatment of both her eyes, she was on topical anti-glaucomatous medication, including dorzolamide hydrochloride and timolol maleate combination and brimonidine tartrate.
Ophthalmological examination revealed 0.15 Snellen visual acuity OD and no light perception in OS. Intraocular pressure was 14 mmHg OD and 15 mmHg OS, as evidenced using applanation tonometry. Anterior segment findings included megalocornea and temporally located posterior embryotoxon bilaterally. Fundoscopy revealed nearly total cupping and pallor of the optic disc and multiple retinal hemorrhagic foci in the macula with decreased autofluorescence corresponding to the hemorrhagic areas (Figures 1 A and B). Spectral domain optical coherence tomography (SD-OCT; Topcon 3D OCT-2000, Topcon Inc., Japan) revealed thickening and increased reflectivity of the outer retinal layers at the fovea with disturbance of the IS/OS layer (Figure 2 A). There was a full-thickness loss of retinal integrity along with subretinal hyper-reflectivity competent with hemorrhage, temporal to the macula. Hyperreflectivity over the retina in the vitreous because of hemorrhage and increased hyper-reflectivity of the internal limiting membrane (ILM) over the patchy hemorrhagic area were also noted (Figure 2 B).
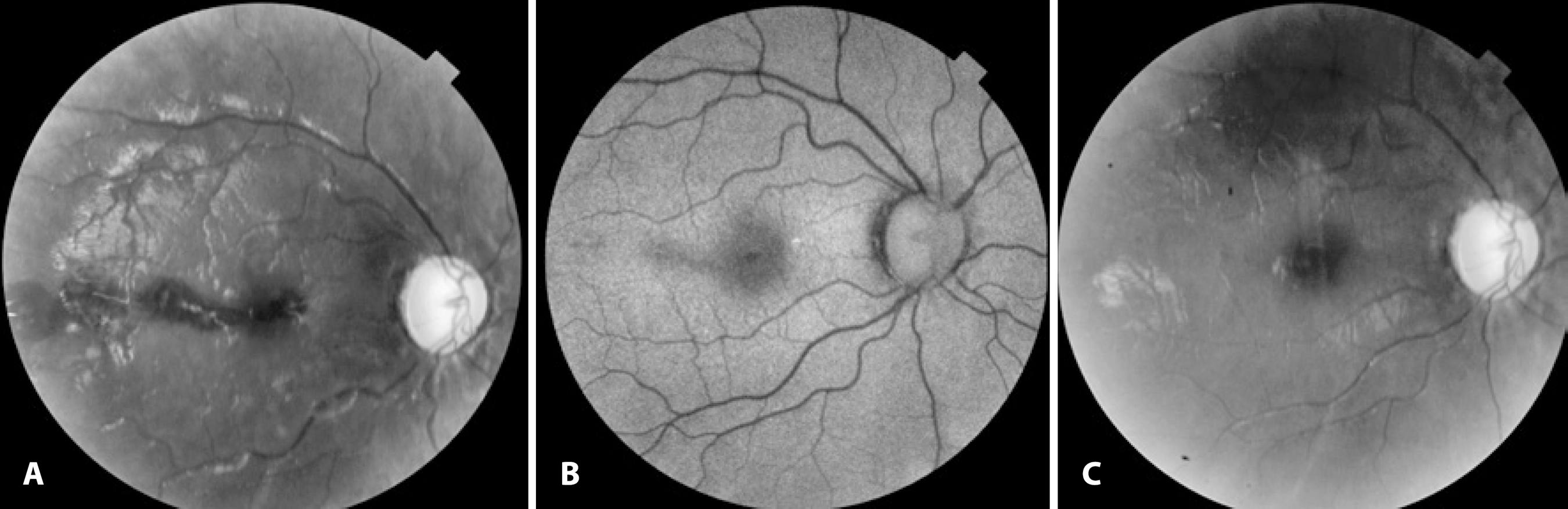
Figure 1 A) Grey-scale fundus image of the right eye showing foveal and extrafoveal retinal hemorrhage 5 days after the roller coaster ride. B) Decreased autofluorescence in the areas where retinal hemorrhage was noted. C) Grey-scale fundus image of the right eye 2 months after admission, showing resolution of the hemorrhages.
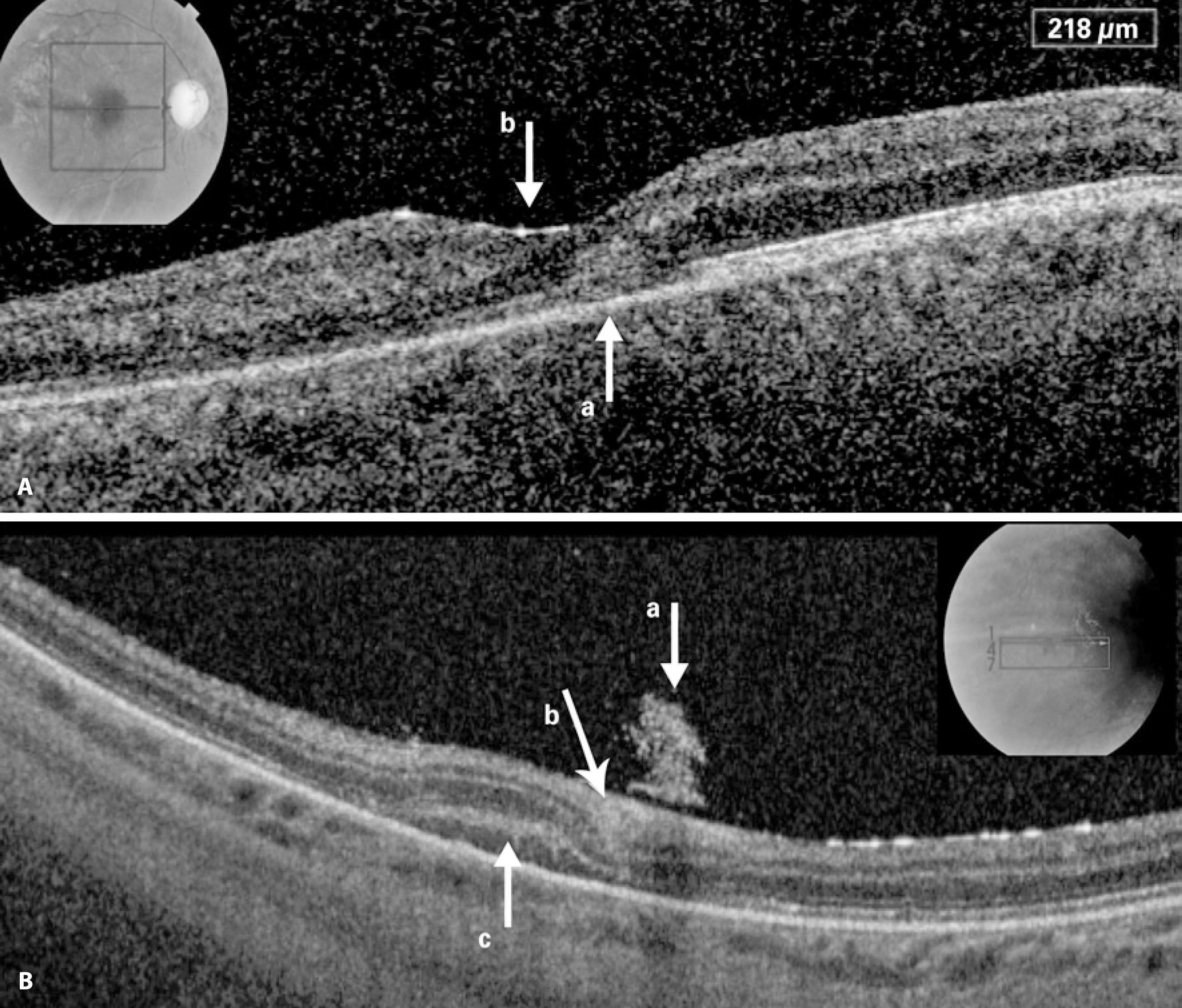
Figure 2 A) Spectral-domain optical coherence tomography (SD-OCT) image of the fovea revealing intra- and subretinal hemorrhage blurring the continuity of the IS/OS band (lower arrow), with increased hyper-reflectivity of the internal limiting membrane (ILM) (upper arrow). B) SD-OCT image of the extrafoveal area, showing hyper-reflectivity in the vitreous because of an hemorrhage (upper arrow), hyper reflectivity under ILM and in the ganglion cell layer (middle arrow) because of an hemorrhage, and hyper-reflectivity corresponding to the subretinal hemorrhage (lower arrow).
The patient did not have any previous or current systemic disease, did not use any systemic drugs, and had no recent history of accident, trauma, or Valsalva maneuver. When asked to help identify any etiological factor that may have caused the retinal hemorrhage, she recounted riding a roller coaster at an amusement park 5 days prior.
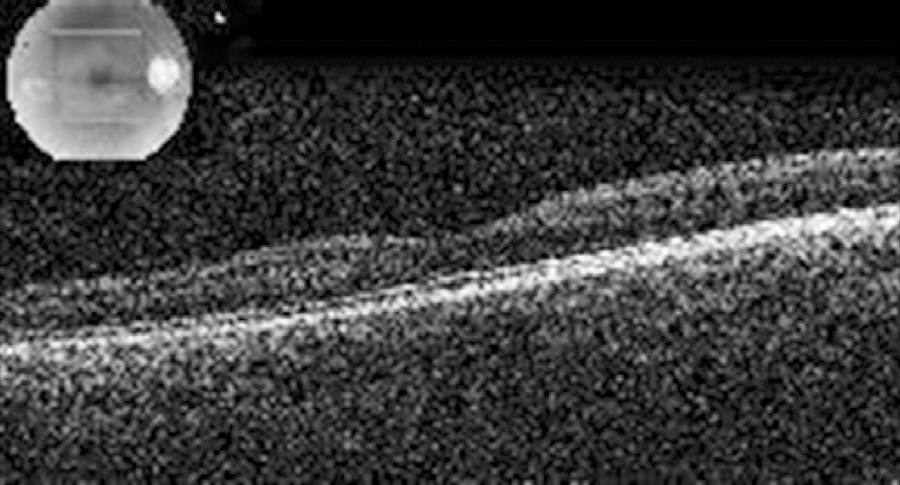
Hematological evaluation revealed iron deficiency anemia, and she was prescribed iron supplements. We followed up with her weekly during the first month and monthly thereafter up to the sixth month. One week after her initial evaluation, her visual acuity increased to 0.3 in OD. After 2 months, the hemorrhages had completely resorbed (Figure 1 C), and SD-OCT sections were found to be normal without any evidence of disturbance of the retinal layers. Only the hyper-reflectivity of the ILM at the fovea remained stable. At the six-month visit, visual acuity was still 0.3, with stable SD-OCT findings (Figure 3).
DISCUSSION
We considered this retinal hemorrhage to be caused by gravitational forces during a roller coaster ride. The excitement of roller coaster rides partly comes from complex and abrupt changes in motion. Roller coaster riding causes rapid acceleration and deceleration in all three dimensions with positive and negative g-forces. The complex and abrupt changes in motion have the potential to cause sudden hyperextension, hyperflexion, or rotation of the neck, causing injury to the carotid or vertebral arteries through the creation of intimal tears(1). Individuals with connective tissue disorders are more vulnerable to these injuries; however, phenotypically normal people may also have ultrastructural connective tissue abnormalities, which may increase the risk of injury.
Riding roller coasters can cause systemic complications, including headache, intracranial hemorrhage, vascular dissection (vertebral artery and internal carotid artery), cerebral aneurysm, and cardiac complications such as arrhythmia and myocardial infarction. Reported ocular complications because of indirect trauma include retinal macrovessel decompensation as observed in a 19-year-old female(2), macular hemorrhage as observed in a 26-year-old female(3), and retinal artery occlusion that is associated with ipsilateral ophthalmic artery occlusion secondary to internal carotid artery dissection in a 35-year-old female(4). Our patient developed blurred vision 1 day after the roller coaster ride. We believe there could be two explanations for the delay in symptoms; either she may not have noticed the blurring in her eye which already had poor visual acuity or the retinal edema and hemorrhage may have migrated towards the fovea.
Mechanical disruption of macular vessels by shearing forces at the interface between the vitreous and retina, increased retinal venous pressure caused by sudden increases in cerebral pressure, high hydrostatic pressure because of g-forces temporarily and intermittently disrupting blood flow to the head and eye, or a mechanism similar to shaken baby syndrome (SBS) are possible reasons for the hemorrhage(3).
Roller coasters can accelerate passengers up to 100 km/h in 2.5 s(5). Repositioning of a dislocated intraocular lens during a roller coaster ride after reaching a height of 73 m and being brought to a speed of 130 km/h exposing passengers to a centripetal force of 4 G has been reported(6). In SBS, which is primarily caused by repeated acceleration-deceleration forces, retinal hemorrhage is observed in 50%-100% of patients(7); usually bilaterally but also unilaterally with asymmetric presentation. Shaking induces shearing forces at the vitreoretinal interface and is the main contributing factor in multilayered retinal hemorrhages observed in SBS. Repeated acceleration and deceleration is believed to be necessary for the vitreous to separate from the retina in cases with retinoschisis(8). Asymmetric presentation was observed in this case. This may be attributed to the difference in ocular dynamics in these two eyes, which had undergone several major operations in the past.
FAF is a method of evaluating the integrity of the retinal pigment epithelium (RPE), with a normal RPE metabolic activity showing a homogenous pattern and hypo-autofluorescence showing probable photoreceptor or RPE cell impairment. A report on FAF imaging in patients with blunt ocular-trauma demonstrated hypo-autofluorescence of recent subretinal hemorrhage with no degradation of red blood cells and hyper-autofluorescence of old subretinal hemorrhage on degradation of blood cells(7). In our case, the area of hypo-autofluorescence because of blockage of hemorrhage resolved, and iso-autofluorescence was observed during follow-up.
With this case report, we wish to attract attention to a completely and spontaneously recovered sub- and intraretinal macular hemorrahge in a patient went for a roller coaster ride. This patient has the risks of probable ocular tissue alterations because of congenital glaucoma and previous surgeries. As ophthalmologists, we should warn our younger patients with predisposing factors against the possible risks of injury on riding roller coasters.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

