INTRODUCTION
Uveal metastasis of systemic carcinoma to the eye is estimated to occur in 8% of cases, according to the results of autopsy evaluations where microscopic detection rate is reported(1). The rate of intraocular metastasis varies according to the primary tumor site and the degree of systemic control. A previous report suggests that the frequency of macroscopic metastases has decreased over 12 years from 4.7% to 1% owing to improved cancer therapy(2).
Uveal metastases occur far more frequently in the choroid than in the iris, possibly due to the substantial blood supply to the posterior choroid by the posterior ciliary arteries(3).
Metastatic tumors to the iris are relatively uncommon; they may present as stromal nodules or ill-defined iris thickening, or they may be associated with atypical features such as pain, iridocyclitis, and hyphema(4,5). In 2014, Shields et al. reported their 40-year experience of 104 cases of iris metastases arising from systemic cancer, demonstrating the breast, lung, and skin as the most common primary sites for such lesions(4).
Many of these patients are never examined by an ophthalmologist because many have no visual complaints or have systemic advanced disease.
Here, we describe three patients with iris metastasis and with different presentations and discuss the diagnostic challenges and unusual findings associated with these cases.
CASE REPORTS
Case 1
A 61-year-old man presented with a 3-month history of blurred vision affecting the right eye and the presence of iris lesion. His past ocular history was unremarkable, while his past medical history included a renal adenocarcinoma treated by total nephrectomy 5 years previously. Follow-up with imaging and laboratory studies demonstrated no evidence of recurrence or metastatic disease.
On admission, ocular examination revealed a best-corrected vision of 20/30 in the right eye and 20/20 in the left eye. Full extraocular motion was observed. The pupils were 3 mm in diameter and reactive to light. The right pupil had an area of irregularity inferiorly, and there were neovessels in the collarette (Figure 1 A). A 2+/4+ anterior chamber reaction with no keratic precipitates were also observed. Further, a 7 × 4 mm pinkish-yellow mass from 1 to 5 o'clock with intrinsic friable vessels was observed, in addition to a band of tissue from 7 to 9 o'clock in the anterior chamber. The intraocular pressure was 25 mmHg (right eye) and 12 mmHg (left eye), as determined by applanation tonometry. Fundoscopic examination was normal. Based on all these findings, a clinical diagnosis of an iris tumor was made. Ultrasound biomicroscopy (UBM) of the right eye revealed an iridociliary mass with homogeneous reflectivity, featuring areas of internal hyporeflective spaces within the tumor with clear margins (Figure 1 B). UBM of the left eye was normal.
Hypotensive agents and topical prednisolone 1% three times daily were initiated. Magnetic resonance imaging (MRI) revealed a renal mass, in addition to liver, brain, and pulmonary masses. A clinical diagnosis of iridociliary metastasis arising from a primary renal carcinoma was established. Treatment with oral anti-tyrosinase was initiated, leading to shrinkage of both the iris and the systemic lesions (Figures 1 C and 1 D). The patient remains alive at 18 months after the initial diagnosis.
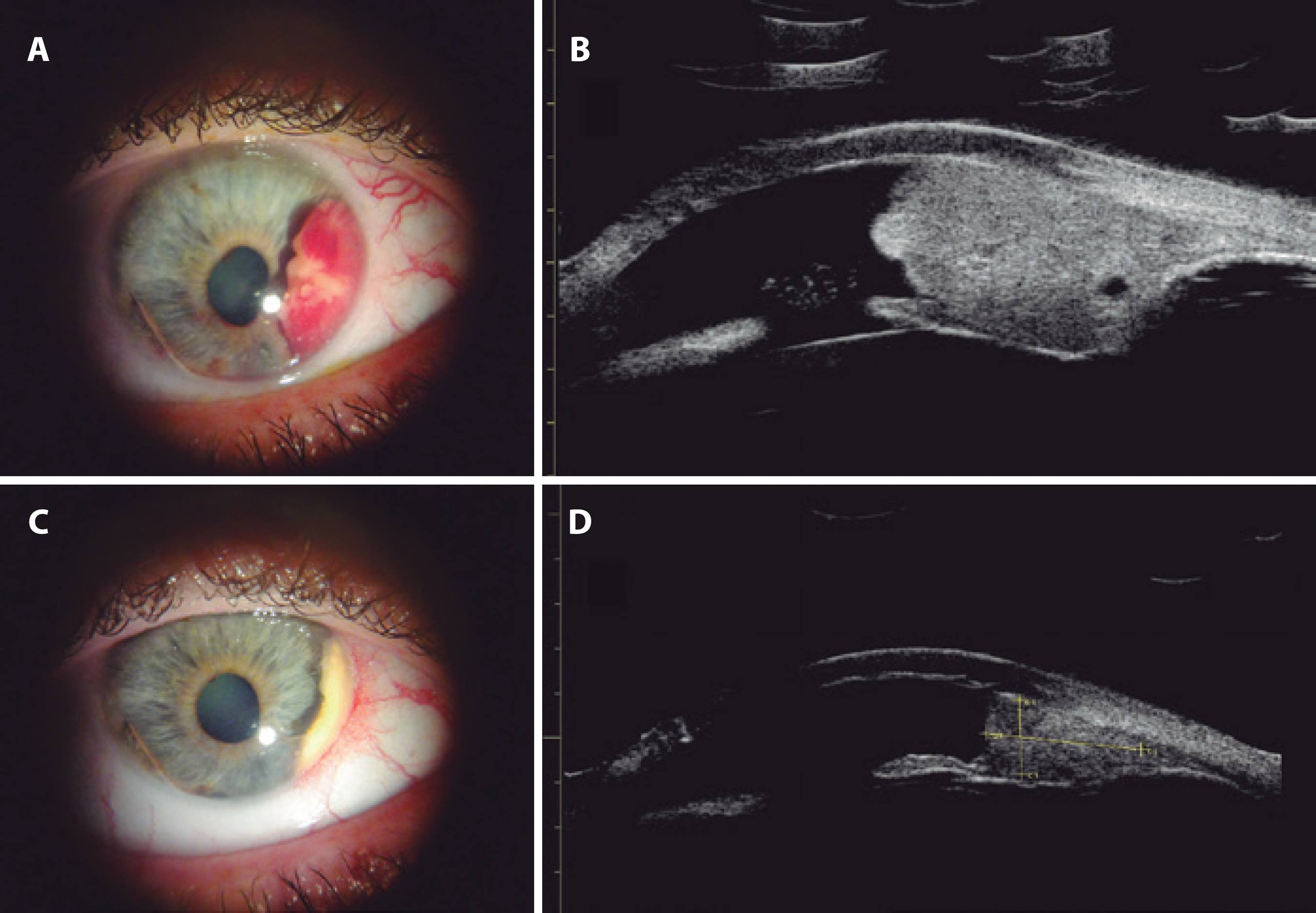
Figure 1 Case 1. A) Photography demonstrating a 7 × 4-mm pinkish-yellow mass from 1 to 5 o'clock with intrinsic friable vessels. A band of tissue was observed from 7 to 9 o'clock in the anterior chamber. B) Ultrasound biomicroscopy (UBM) image of an iridociliary mass with homogeneous reflectivity and areas of internal hyporeflective spaces within the tumor. C and D) Post-treatment images demonstrating shrinkage of the lesion.
Case 2
A 58-year-old female presented with pain and blurred vision in her left eye. She had breast cancer, which was treated 10 years earlier with mastectomy, lymphadenectomy, and systemic chemotherapy. Ocular examination revealed a best corrected vision of 20/20 in the right eye and finger-counting only in the left eye. Full extraocular motion was observed. The left pupil was slowly responsive to light, with an area of irregularity at 2 o'clock and a 3 × 2-mm white pearl mass in the temporal upper quadrant associated with bulging of the iris superiorly (Figure 2 A). Intense anterior chamber inflammation with 3+/4+ cells and an inferior white hypopyon without keratic precipitates was observed. UBM of the left eye revealed an iris lesion with heterogeneous reflectivity (Figure 2 B). Systemic work-up for inflammatory and infectious uveitis was negative. Other systemic metastases were also ruled out. Findings of histological examination of an iris biopsy were highly suggestive of metastatic carcinoma (Figure 2 C). Immunohistochemical analyses were positive for CEA and CK7, and negative for estrogen. The patient was treated with external beam radiotherapy, with full regression of the lesion observed (Figure 2 D). After 13 months follow-up, no evidence of disease was observed at the primary site or other sites of metastatic disease.
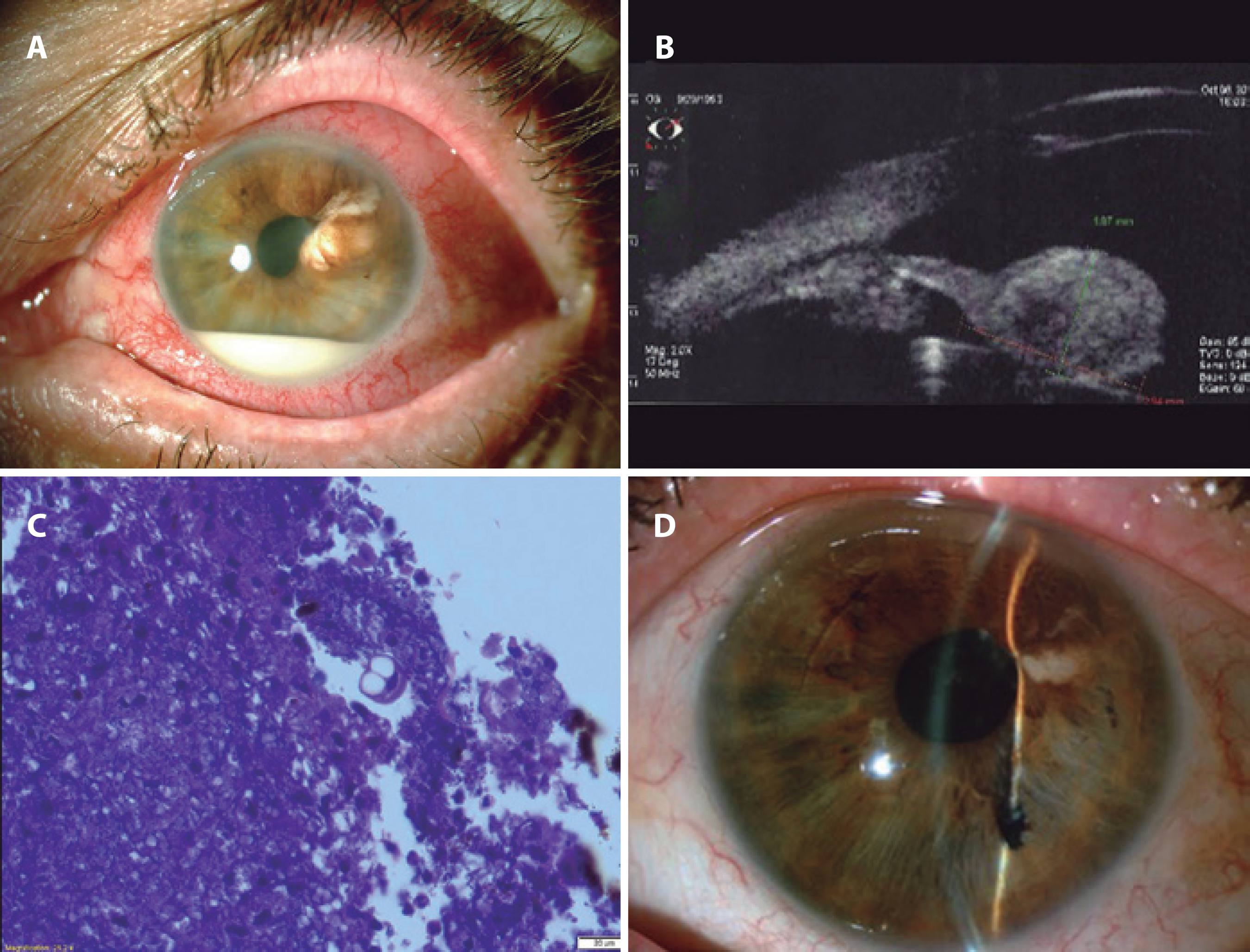
Figure 2 Case 2. A) Photograph of a white pearl mass in the temporal upper quadrant associated with bulging of the iris superiorly. Intense anterior chamber inflammation with 3+/4+ cells was observed with an inferior white hypopyon without keratic precipitates. B) UBM image of the lesion with heterogeneous reflectivity. C) Lesion after treatment. D) Histopathology.
Case 3
A 25-year-old woman presented with an iris lesion affecting her right eye and a 3-month history of blurred vision. Her past ocular history was unremarkable. She had an adenocarcinoma 1 year previously, which was treated by a total parotidectomy and a mandibulo-mastoidectomy with extraction of her cervical lymph nodes; however, surgical margins were not clear. Adjuvant external beam radiotherapy was performed at the surgical site. No evidence of local recurrence was observed on follow-up. Ocular examination revealed a best corrected vision of 20/100 in the right eye and 20/20 in the left eye. Full extraocular motion was observed. The right pupil was irregular and slowly responsive to light, with no signs of uveal inflammation. A pink iris mass was observed from 1 to 3 o'clock with the presence of intrinsic vessels (Figure 3 A). UBM of the right eye revealed an iridociliary mass with homogeneous reflectivity and areas of internal hyporeflective spaces within the tumor (Figure 3 B and 3 C). A clinical diagnosis of metastatic disease was made. Full work-up, including positron emission tomography (PET), findings were negative. Plaque brachytherapy was performed to treat the focal iris metastasis, with consequent lesion improvement observed (Figure 3 D). However, the patient died 10 months later due to the progression of metastatic disease.
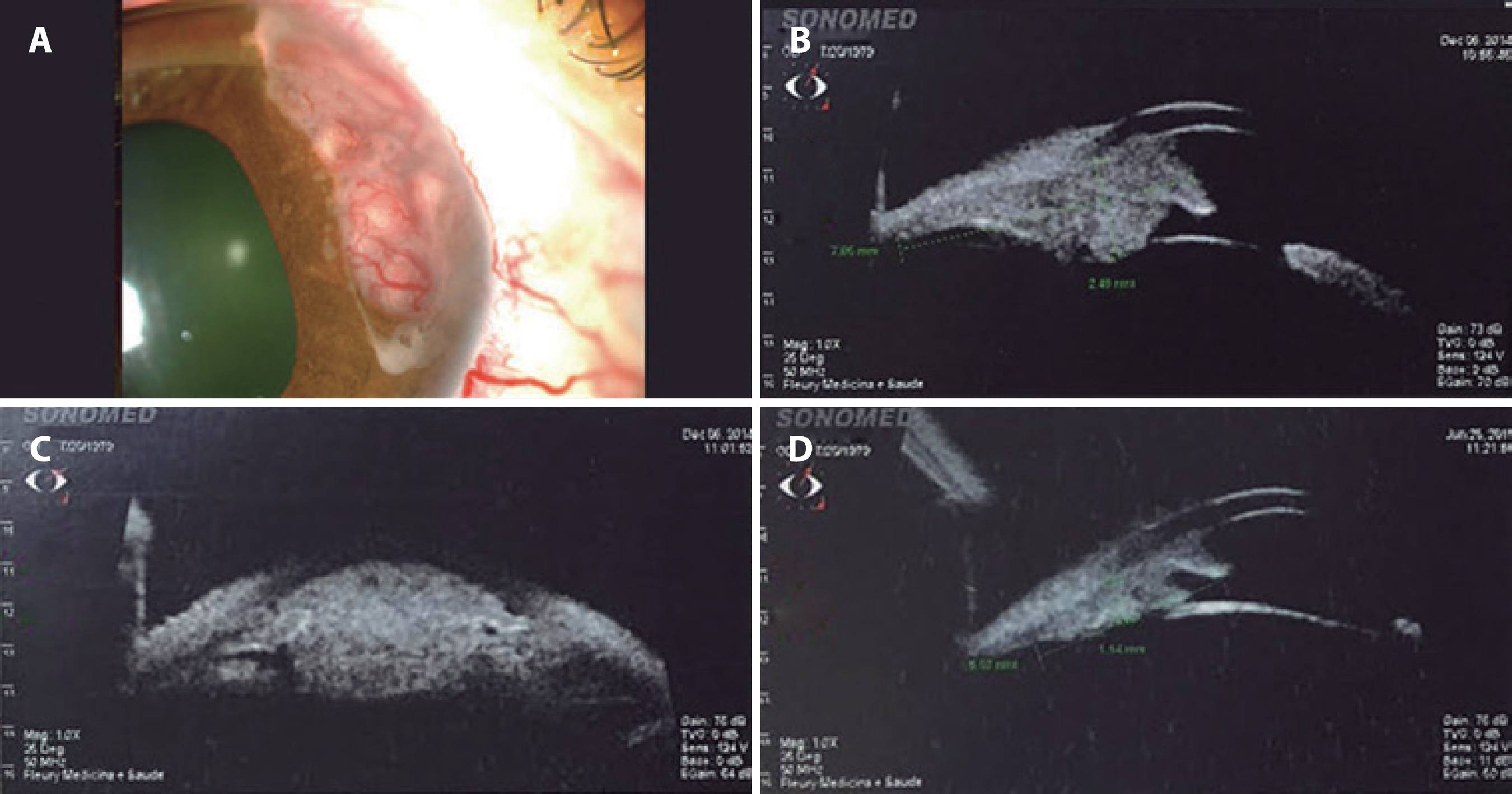
Figure 3 Case 3. A) Biomicroscopy image demonstrating a pink iris mass from 1 to 3 o'clock with intrinsic vessels. B and C) Ultrasound biomicroscopy (UBM) demonstrating a mass with homogeneous reflectivity and areas of internal hyporeflective spaces. D) UBM after treatment showing shrinkage of the lesion.
DISCUSSION
In a clinical survey(6) of 3,680 iris tumors, 21% were reported as cystic and 79% as solid. In the solid group, 68% were melanocytic and 11% were non-melanocytic. Non-melanocytic iris tumors included a range of diagnoses, including choristomatous, vascular, fibrous, neural, myogenic, epithelial, xanthomatous, metastatic, lymphoid, leukemic, and non-neoplastic conditions masquerading as iris masses. Only 67 (2%) tumors were metastatic.
In the largest published series of 107 eyes with metastatic tumors of the iris, Shields et al.(4) reported primary tumors were more likely to originate from the breast (33%), lung (27%), skin (12%), kidney (7%), esophagus (3%), and other regions. The kidney and parotid are considered very rare primary tumor sites. Shields et al.(4) found that the majority of iris metastases were inferior (35%) and superior (28%), whereas the majority of cases were nasal (28%) or temporal (28%) in a series reported Ferry and Font(2). All three of our patients reported blurred vision, with the presence of non-melanocytic iris lesions on the nasal side in cases 1 and 3 and in the upper temporal region in case 2. Shields et al.(4) reported pain and blurred vision as the most common complaints, as observed in cases 1 and 2. Pain was related to secondary glaucoma in case 1 and to inflammation in case 2. All cases had a history of previously treated malignancy, as did the majority of patients in previous studies(4,5). Melanoma is considered the main differential diagnosis of iris metastasis, but it is clinically challenging to diagnose due to a lack of specific pathognomonic features(7).
UBM has been used to study and monitor iris tumors in previous studies(8); however, no pathognomic features have demonstrated utility in distinguishing melanomas from other metastases. In a series of UBM studies(8) of iris melanomas, two distinct patterns of tumor vascularity were observed by histological analysis with UBM: small hyperechoic dots relating to small-caliber vessels in the iris stroma; and hypoechoic spaces relating to larger vascular spaces. Cases 1 and 3 exhibited the latter pattern, which may have been attributable to intrinsic vessels visible on slit lamp examination. In case 2, UBM demonstrated irregular reflectivity, with no visible intrinsic tumoral vessels observed on biomicroscopy.
The majority of iris tumors can be diagnosed using clinical historical criteria without the need for cytological or pathologic biopsy. In the largest series of fine-needle biopsies for iris tumors, the most common indications were suspected iris melanomas or metastases(9). In these cases, cytological evaluation of fine-needle aspirates was extremely helpful in distinguishing melanoma from metastatic neoplasm(9). We decided to perform a biopsy of the iris lesion in case 2 as the patient had been treated for breast cancer 10 years previously without relapse, and she presented with no other metastatic foci. Further, as she also presented with signs of severe inflammation, biopsy was able to rule out infection. In cases 1 and 3, biopsy was not necessary as case 1 had a further metastatic focus, and the patient in case 3 was young and had a local aggressive parotid adenocarcinoma with involvement of the regional lymph nodes in addition to an iris lesion. Adenocarcinoma of the parotid develops from the secretory element of the gland and is considered an aggressive lesion with potential for both local lymphatic and distant metastasis(10). The patient in case 3 died shortly after treatment of the iris lesion as she developed distant metastatic disease a few months later.
Unfortunately, the median time interval between the detection of iris metastasis and death is reportedly 24 months(4). It should be noted that cases 1 and 2 remain alive after follow-up durations of 18 and 13 months, respectively.
The treatment of uveal metastases, including iris metastases, is palliative. Patients with other systemic involvement should be treated with systemic chemotherapy, while external radiotherapy or brachytherapy are recommended for the treatment of focal metastases.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

