INTRODUCTION
Scleritis is currently recognized as a heterogeneous group of diseases characterized by inflammation of the sclera, which may be caused by a local or systemic infection, an immune-mediated disease, or a primary manifestation of an acquired connective tissue disorder or vasculitic disease, often signaling a life-threatening situation(1,2). Surgically induced necrotizing scleritis (SINS) occurs after ocular surgeries for cataract extraction, trabeculectomy, strabismus, and pterygium retinal detachment(3).
The diagnosis and treatment of these special cases using immunosuppressive patch grafts or amniotic membrane grafts should be prompt(4). Immunosuppressive agents used to treat these conditions include azathioprine, cyclophosphamide, tacrolimus, and high-dose pulse methylprednisolone(4). Although other biological agents can be used, particularly for the treatment of necrotizing scleritis, which potentially represents vasculitis, rituximab is generally recommended for the treatment of systemic vasculitis(5).
CASE REPORT
Our patient was a 51-year-old woman who presented with a chief complaint of redness and pain affecting both eyes. She previously underwent (2-3 months before) pterygium excision using the bare sclera technique, without the use of adjunctive irradiation or mitomycin C. An ophthalmological examination revealed bilateral conjunctival hyperemia and scleral thinning with peripheral corneal ulcers measuring 5 × 2 mm in the right eye and nasal scleral thinning with peripheral corneal swelling in the left eye that further promoted scleral thinning, staphyloma formation, and subsequent ulcerative necrosis. Complete hematology and immunology profiles for rheumatoid arthritis, antinuclear antibody (ANA), and anti-neutrophil cytoplasmic antibodies (ANCA) were determined, which showed that only ANA was positive and extractable nuclear antigen antibodies (ENA) were negative. Serology tests, such as venereal disease research laboratory test, Treponema pallidum hemagglutination assay, and tuberculin test, were all negative.
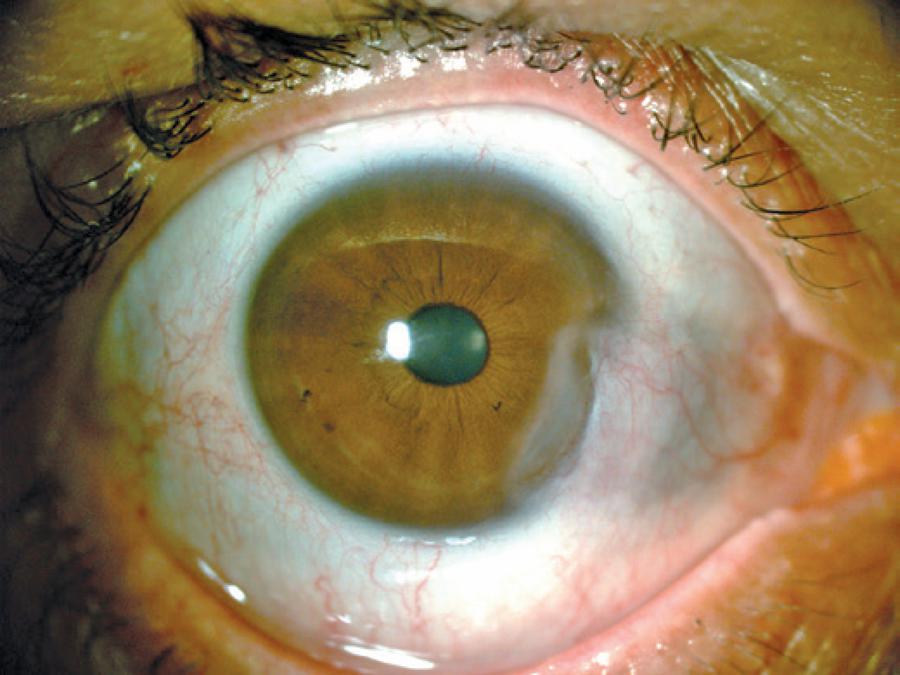
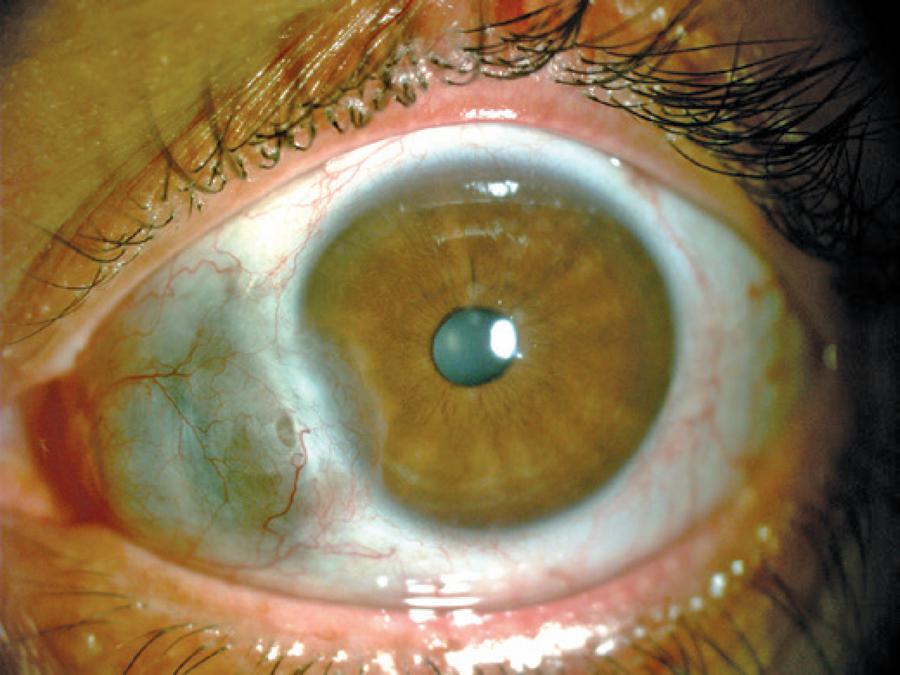
She was further evaluated in the Rheumatology Department because of generalized pain and ANA positivity. Combined with laboratorial analysis showing normal renal, hematological, and hepatic functions and negativity for anti-double stranded DNA (dsDNA), ANCA, ENA, rheumatoid factor, and anti-cyclic citrullinated peptide antibody (anti-CCP), a diagnosis of fibromyalgia and SINS was made, and the patient was promptly treated with high-dose corticosteroids. However, 1 month later, she presented with aggravated scleral thinning; thus, immunosuppressive agents (2 mg/kg of azathioprine and 1 g/m2/month of intravenous cyclophosphamide) were added to corticosteroid therapy for 12 months. However, remission was not achieved and necrotizing scleritis of the right eye continued. Therefore, rituximab treatment was initiated, which resulted in improvement after the first cycle of two infusions of 1 g each administered 2 weeks apart. Visual acuity was preserved in the left eye but decreased from 20/20 to 20/160 in the right eye. The prednisone dose was tapered off, and after 3 months, the patient was free from all drugs (Figures 1-4). She has remained symptom-free for 6 months after the second rituximab cycle. The laboratory workup was repeated twice, and ANA was the only altered parameter with a 1/320 speckled pattern, and ENA remained negative. There was no symptom that could be attributed to a collagen disease.

Figure 1 Right eye before rituximab. Conjunctival and scleral nasal hyperemia with local thinning and a peripheral corneal ulcer.

Figure 2 Left eye before rituximab. Conjunctival hyperemia, scleral thinning, and associated scleral staphyloma with necrotic ulceration.
DISCUSSION
The local and systemic treatment of scleritis has recently undergone significant changes. These changes include more aggressive and early treatment of patients to maintain vision and achieve rapid remission.
Increased use of combination immunosuppressive therapy and biological agents in patients with severe and refractory ocular inflammatory disease has contributed to modifications in the prognosis of these conditions1.
Scleral necrosis and melting may occur after pterygium surgery due to the use of adjunctive irradiation(6) and mitomycin C(7), although the use of these gents reportedly contributes to prolonged inhibition of wound healing. In addition, excessive cauterization during the bare sclera technique may cause scleral necrosis(8). According to a review by Doshi et al.(9), the technique used for pterygium surgery can alter the risk of necrotizing or even infectious scleritis. In 203 cases, SINS occurred in 17.2% and scleritis in 68.8% of cases that underwent the bare sclera technique, as in our case.
Medical management of SINS after pterygium surgery includes immunosuppression with the oral steroids methylprednisolone + cyclophosphamide or tacrolimus for patients who do not respond to cyclophosphamide and azathioprine(4). Surgical intervention in the form of patch grafts of scleral, corneal, or amniotic membranes(10) has also been reported.
Autoimmunity or hypersensitivity is now well accepted as an etiological factor in the development of SINS. Immune complexes have been found in and around episcleral vessel walls by immunofluorescence techniques, and systemic immunosuppressive regimes have been successful in the treatment of SINS(3,10). Clinical or serological markers of connective tissue disorders are present in as many as 62% of cases. Our patient was ANA-positive without evidence of any associated connective tissue disorder. The search for an associated autoimmune disease was exhaustive and included tests for anti-CCP, ENA panel, complement system proteins, and anti-dsDNA. These tests were performed on more than two occasions, particularly for ANA and the ENA panel, because it was important to exclude the possibility of an autoimmune disease associated with ANA positivity, such as systemic lupus erythematosus or systemic vasculitis.
In this case, the scleritis was refractory to classical immunosuppressive therapy, although all recommended steps, including high prednisone doses, azathioprine and cyclophosphamide (12 pulses), were attempted.
A review of the literature for studies of biologic therapy for scleritis revealed case reports and a randomized clinical trial of necrotizing scleritis treated with rituximab after immunosuppressive therapy, which achieved good responses(11,12).
Rituximab is a chimeric anti-CD20 monoclonal antibody that continues to increase in popularity for the treatment of ocular inflammatory diseases and intraocular lymphoma(13). SINS should be considered as a differential diagnosis in patients with scleritis or scleral melting following pterygium surgery, particularly after radiation or mitomycin C therapy. Evidence of a connective tissue disease may or may not be found on clinical examination or laboratory investigations, although it remains uncertain whether an autoimmune disease is present before or is unleashed by the section of sclera. Therefore, it is important to be alert to the risks of scleritis after such surgical procedures, particularly those that can lead to the damage of avascular tissue, such as sclera, because the risks of necrosis and infections are considerably increased. Early diagnosis and prompt immunosuppression is required for the successful management of this complication(4). The CD20 antibody rituximab is now an option that can be used for the treatment of these special cases.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

