INTRODUCTION
Granulomatosis with polyangiitis (Wegener's) predominantly affects the upper and lower respiratory tracts, lungs, and kidneys and represents a rare multisystem necrotizing granulomatous vasculitis of small-sized vessels. Central nervous system, cutaneous, heart, gastrointestinal tract, orbital, and ocular involvement may also be observed(1). Ocular or orbital involvement in granulomatosis with polyangiitis is reportedly occurs in 20-50% of patients(2,3).
Bilateral acute angle-closure (AAC) glaucoma is a very rare clinical entity that is generally caused by the use of various topical or systemic medications, many of which are known to cause pupillary dilatation, emotional stress, dim illumination, surgical anesthesia, viral infections, systemic vasculitis, and subarachnoid hemorrhage(4-7). To our knowledge, this is the first reported case of granulomatosis with polyangiitis presenting with bilateral acute angle-closure glaucoma.
CASE REPORT
A 59-year-old Caucasian man presented to a local ophthalmologist with acute bilateral onset of ocular pain, blurred vision, and a severe headache. He was diagnosed with bilateral AAC glaucoma and immediately referred to the Ophthalmology Department, Gaziantep University for further evaluation and treatment.
On initial examination, his best-corrected visual acuity (BCVA) was 20/200 in both eyes (OU). IOPs were measured using an applanation tonometer and recorded as 43 mmHg and 47 mmHg in the right and left eye, respectively. On slit-lamp examination we observed bilateral conjunctival chemosis, mild corneal edema, shallow anterior chambers, and immature senile cataracts. On gonioscopy, we observed angle closure in the superior and lateral quadrants (Shaffer Classification, Grade 0), and Grade 1 angle closure in the inferior and medial quadrants. There was no evidence of previous angle closure glaucoma, such as iris atrophy or glaucomflecken. He had no previous glaucoma-related medical history. We initially planned treatment with timolol maleate, 0.5% twice daily; brimonidine, 0.15% twice daily; pilocarpine, 1% four times daily; oral acetazolamide, 250 mg four times daily; and 350 ml mannitol, 20% intravenously. Six hours later, IOPs dropped to 28 mmHg bilaterally. The following day, we continued topical anti-glaucomatous medication and oral acetazolamide. His BCVA improved to 20/30 and 20/40 in the right and left eye, respectively. His IOP dropped to 19 mmHg and 20 mmHg in the right and left eyes, respectively. On slit-lamp examination, we observed resolution of the mild corneal edema, reduction in conjuctival chemosis, and improved anterior chamber depth which continued to be shallow peripherally (Figure 1). Undilated fundus examination demonstrated normal optic discs and maculae in both eyes. Subsequently, YAG laser iridotomies were performed 36 hours after the initial examination. On the third day, IOPs were 11 mmHg in the right eye and 13 mmHg in the left eye with topical and oral anti-glaucomatous medication. Therefore, oral acetazolamide was stopped at this time.
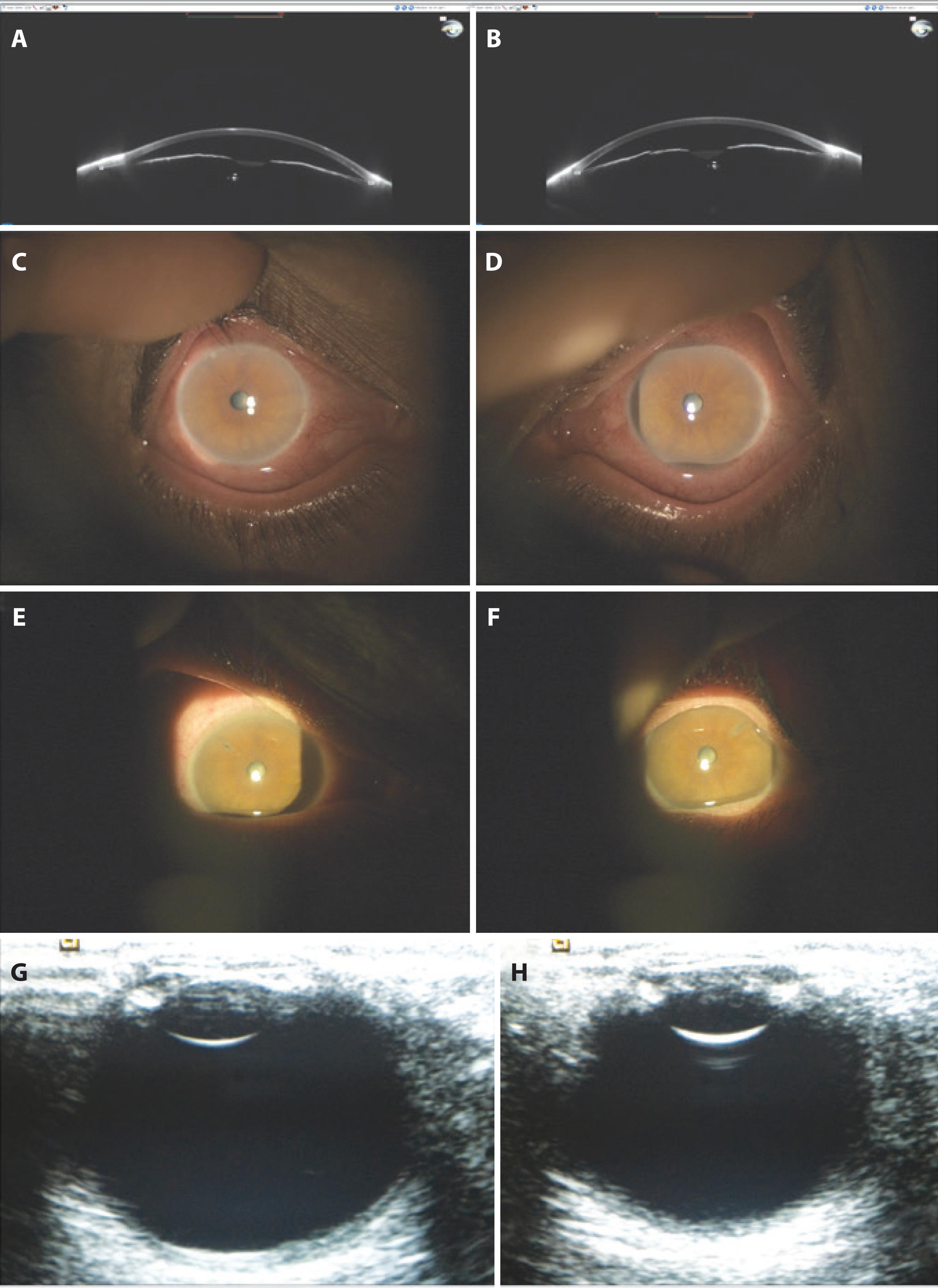
Figure 1 A, B) Sirius topography revealed narrow angles in both eyes on the second day. C, D) Slit-lamp examination of both eyes on the second day. E, F) Slit-lamp examination of both eyes following laser iridotomy. G, H) B-scan ultrasonography of both eyes on the second day.
The patient reported a one-week duration of shortness of breath and mild fever at the initial presentation. We therefore arranged a consultation with our department of respiratory medicine on the first day of hospitalization. Laboratory examinations and radiological evaluations were planned by the same department. Serological examination demonstrated an elevated erythrocyte sedimentation rate, proteinuria, and elevated levels of C-reactive protein, urea, and creatinine. Chest radiography and computed tomography (CT) revealed ground glass opacities with nodular consolidation in the right upper lobe. Enlarged bilateral axillary, paratracheal, and carinal lymph nodes were also noted (Figure 2 A, B). Subsequently, he was evaluated by our departments of rheumatology and nephrology. Abdominal CT and ultrasonography revealed bilateral cysts within the kidney parenchyma. Pathological examination of a kidney biopsy specimen was reported as consistent with focal and segmental glomerulosclerosis (FSGS) with chronic tubulointerstitial changes. Additional laboratory evaluations revealed the presence of autoantibodies to neutrophil cytoplasmic components (cytoplasmic anti-neutrophil cytoplasmic antibodies, C-ANCA) with proteinase-3 (PR3) specificity. Granulomatosis with polyangiitis (Wegener's) was diagnosed accordingly and treatment with cyclophosphamide and prednisolone was initiated.
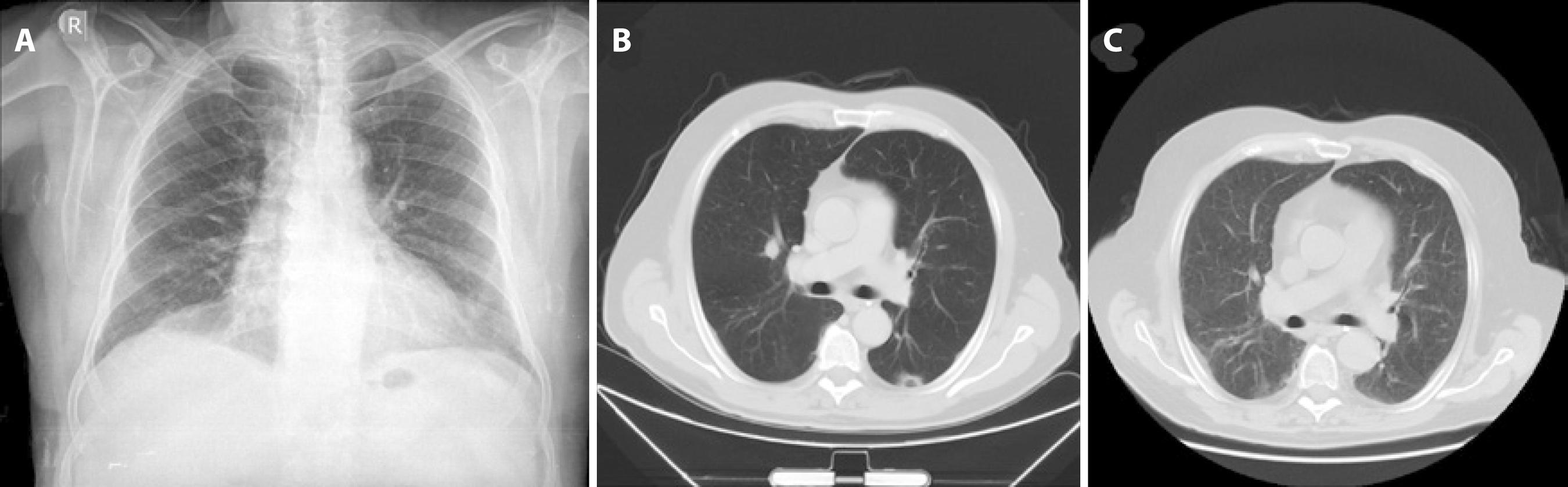
Figure 2 A) Chest radiography revealed bilateral opacities consistent with focal consolidation. B) Chest CT demonstrated ground glass opacities with focal regions of consolidation in the right upper lobe. C) Chest CT at 3 months after systemic cyclophosphamide and prednisolone therapy demonstrated complete resolution of nodular opacities in the right upper lobe.
The patient attended a follow-up visit one week later and reported complete resolution of his ocular symptoms. His BCVA had improved to 20/20 and 20/25 in the right and left eye, respectively. IOPs were 15 mmHg in the right eye and 16 mmHg in the left eye. Openings created by laser iridotomy were seen to be patent. Gonioscopy revealed angles open to the scleral spur bilaterally. All systemic symptoms continued to gradually improve with systemic treatment (Figure 2 C).
DISCUSSION
Granulomatosis with polyangiitis, formerly known as Wegener's granulomatosis, commonly involves the upper and lower respiratory tracts and kidneys. Ocular or orbital manifestations are present in approximately one-tenth of patients with granulomatosis with polyangiitis(8). Ocular involvement can range from mild conjunctivitis and episcleritis to more severe inflammation with peripheral ulserative keratitis, scleritis, uveitis, and retinal vasculitis. Orbital involvement may cause proptosis, diplopia, restrictive myopathy, and compressive optic neuropathy, as a consequence of orbital inflammation(8). Ocular or orbital manifestations may result from a variety of pathologies, including focal vasculitis of small-sized vessels, granulomatous inflammation, vascular thrombosis, hemorrhage, or as a consequence of chronic inflammation or ischemia(9). AAC glaucoma has been previously reported to be associated with other vasculitides(4-6). The exact mechanisms underlying the association between AAC glaucoma and systemic vasculitis are yet to be elucidated. Choroidal ischemia secondary to vasculitis may cause choroidal thickening of an already narrow angle, which may then precipitate an acute episode of glaucoma. Previous studies have reported that a 20% increase in choroidal thickness is sufficient to result in a forward shift of the iris against the cornea and acute development of glaucoma(10). Alternatively, iris sphincter ischemia secondary to vasculitis, AAC glaucoma, or increased sympathetic output due to pain related to vasculitis may cause mydriasis and precipitate acute glaucoma(6). In the present case, we did not observe choroidal thickening on B-Scan ultrasonography or fundus examination. Therefore, we believe AAC glaucoma in our patient was most likely due to the development of mydriasis.
An accurate diagnosis of granulomatosis with polyangiitis is dependent on comprehensive clinical examinations and supporting pathology evaluations. Early diagnosis and treatment of granulomatosis with polyangiitis may prevent the development of serious associated complications. To the best of our knowledge, this is the first report of bilateral AAC glaucoma as the initial presenting symptom of granulomatosis with polyangiitis. The findings in the present case demonstrate AAC glaucoma as a rare but significant manifestation of granulomatosis with polyangiitis.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

