INTRODUCTION
Lacrimal sac tumors are rare with a typically non-specific presentation. As the most common signs of lacrimal sac tumors are epiphora or presence of a mass, the process can be incorrectly diagnosed as dacryostenosis or chronic dacryocystitis (DC)(1-4). Consequently, definitive diagnosis is delayed leading to worsened prognosis(5).
Adenoid cystic carcinoma (ACC) is an extremely rare form of malignant epithelial neoplasia of the lacrimal sac. However, it is the most common type of malignant epithelial tumor of the lacrimal and minor salivary glands(6,7). To date, 11 cases of ACC of the lacrimal sac have been reported in literature (Table 1).
Table 1 Summary of previously reported clinical cases
| Age | Sex | Side | Presentation | Treatment | Recurrence | Follow-up interval | Author |
|---|---|---|---|---|---|---|---|
| 62 | F | Right | 2 years epiphora. Lacrimal sac mass (without data specification) | Enbloc excision of the tumor with exenteration of the orbit, radical maxillectomy, and ethmoidectomy. | No | 14 months | L. Miller et al.(8) |
| 57 | F | Left | Epiphora and swelling of the left lower lid (without data specification) | Orbital exenteration. Further treatment: CT. | Lung metastases after 2 years. | 48 months after which she was lost | C. Kincaid et al.(3) |
| 38 | F | Not specified | Not specified | Surgery | No | 60 months | A. Stefanyszyn et al.(1) |
| 51 | F | Not specified | Not specified | Not specified | No | 60 months | A. Stefanyszyn et al.(1) |
| 64 | F | Not specified | Not specified | Not specified | No | 60 months | A. Stefanyszyn et al.(1) |
| 41 | M | Left | 1 month epiphora and lacrimal sac mass | Surgery and RT | No | 12 months | R. Parnel l et al.(9) |
| 72 | M | Right | 1 year epiphora and lacrimal sac mass | Orbital exenteration and RT for pulmonary metastases | Lung metastases after 16 years | 192 months | DN. Parmar et al.(2) |
| 62 | F | Not specified | Epiphora, epistaxis and nasal obstruction (without data specification) | Surgery and RT | Not specified | Not specified | O. Choussy et al.(10) |
| 74 | M | Right | Tearing associated with a palpable mass in the internal canthus (without data specification) | Exclusive RT | No | Death at 30 months | A. Montalban et al.(5) |
| 48 | F | Not specified | Mass | Globe sparring surgery, RT, and CT | Metastatic disease | Death at 48 months | T. El-Sawy et al.(11) |
| 70 | M | Not specified | Mass | Globe sparring surgery, RT, and CT | No | 6 months | T. El-Sawy et al.(11) |
F= female; M= male; RT= radiotherapy; CT= chemotherapy.
We report the case of a 41-year-old woman with a right lacrimal sac ACC with a follow-up duration of 24 months post surgery.
CASE REPORT
A 41-year-old Caucasian woman presented to our department in August 2012 with a 2-year history of lacrimation and pain affecting the medial canthus of the right eye. The lacrimal drainage system was permeable; however, reflux of mucopurulent material was observed. Dacryocystography (DCG) demonstrated a patent pathway with forced passage of contrast from the lacrimal sac. Tumoral pathology was not suspected, and the patient was diagnosed with dacryocystitis and started on topical and systemic antibiotic treatment accordingly.
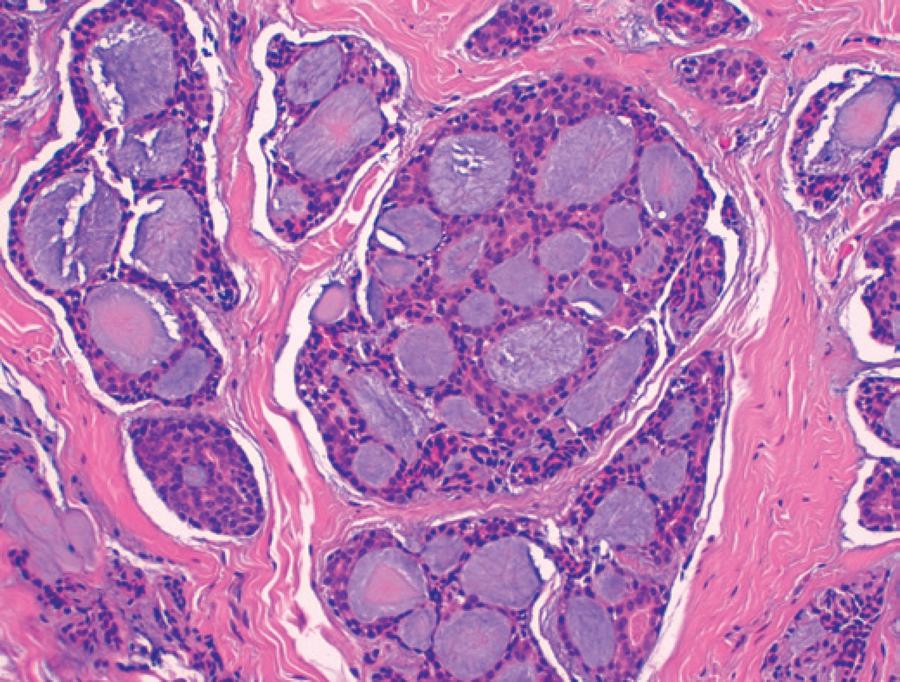
In August 2013, the patient was re-attended complaining of pain in the right canthus and mucosanguineous secretions from the lacrimal punctum in response to pressure. A new DCG was performed demonstrating a filling defect in the sac without passage of contrast into the distal duct. Orbital magnetic resonance imaging identified a solid-cystic lesion measuring 17 × 17 × 13 mm in the right lacrimal sac seen extending towards the orbit and infiltrating the extraconal fatty tissue (Figure 1). Right dacryocystectomy was performed following observation of a gelatinous mass infiltrating the lacrimal sac and eroding the surrounding bony structures. Pathologic examination demonstrated ACC with a predominantly cribriform pattern infiltrating the muscle and bone tissue with additional perineural infiltration (Figure 2). In the extension study, no signs of tumor spread were evident. Further intervention with right lateral rhinotomy located the mass to the canthal area. The tumor planes were dissected and an osteotomy was performed from the canthal ligament to the orbital floor. The orbital floor was reconstructed before tension-free closure and approximation of the rhinotomy flap. Pathological examination of the dissected tissues confirmed the existence of ACC. Following surgery, the patient had a favorable clinical course. A multidisciplinary approach was established, and the patient received 33 sessions of radiotherapy with no signs of recurrence observed after a follow-up for 2 years.
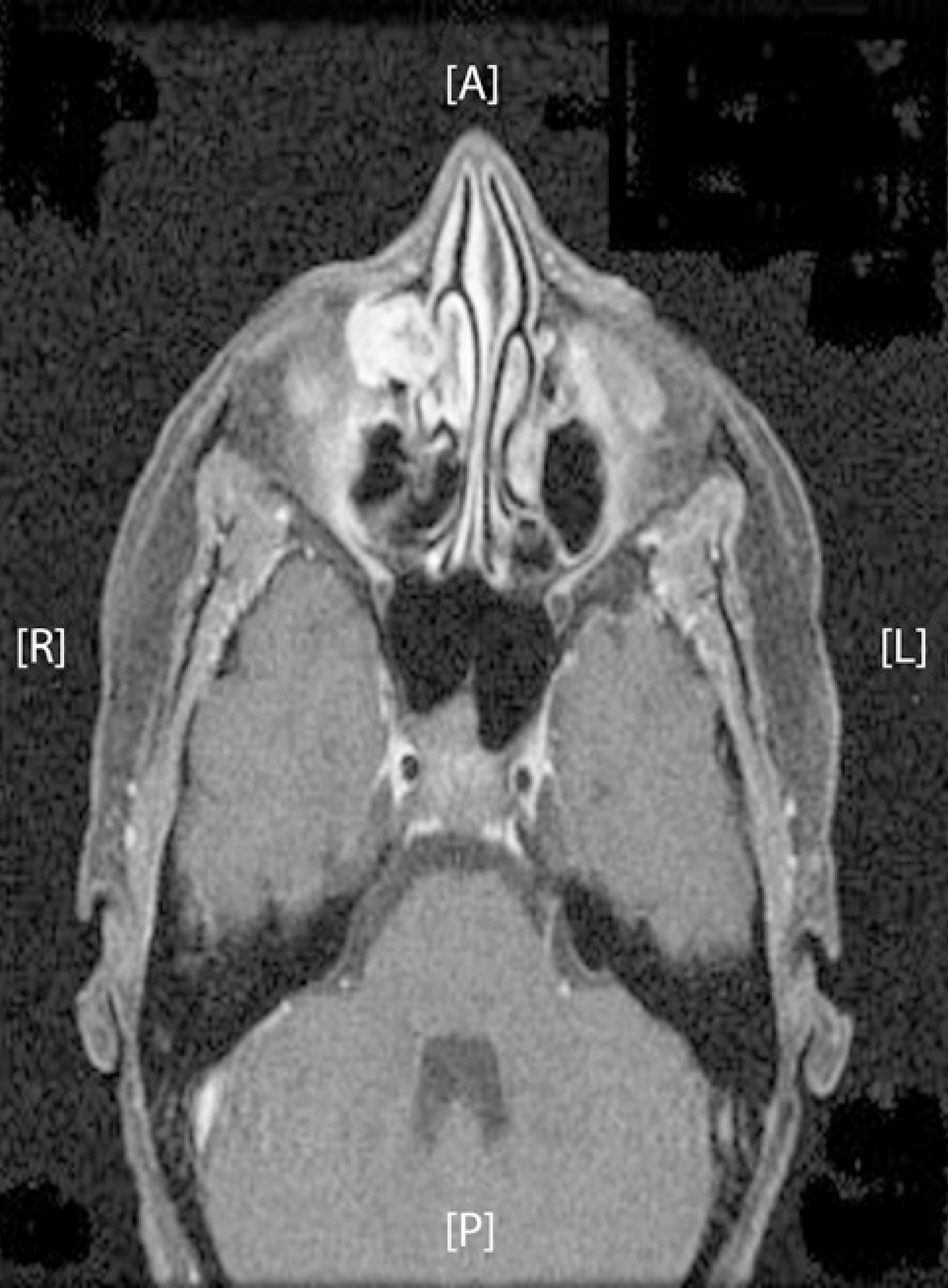
Figure 1 Solid-cystic lesion occupying the right lacrimal sac region consistent with a neoplastic process.
DISCUSSION
Epiphora is the most common clinical sign of lacrimal sac tumors(1-4). These tumors may also present as masses in the canthal area. Sanguineous discharge (spontaneous or on lacrimal sac irrigation), epistaxis, pain, and skin ulceration are all highly suspicious of malignancy.
Pathologically, lacrimal sac tumors can be divided into epithelial tumors, mesenchymal tumors, lymphomatous lesions, melanoma, and neuronal tumors. Inflammatory lesions are not true neoplasms but appear as masses in the lacrimal sac with similar symptoms(1).
The most common malignant tumors affecting the lacrimal sac are of the epithelial type, with squamous subtype having the highest incidence within this group. ACC is an extremely unusual entity in the lacrimal drainage system(1,2,4).
ACC is slow-growing(6,7) but has a tendency for perineural invasion and spread to adjacent tissues, such as the bone(4,8). Local recurrence is frequently observed several years after surgical excision. Although a late finding, hematogenous metastases are possible and(7) most commonly affect the lungs. Local lymph node involvement is rare(5-7).
From a histological standpoint, there are three types of ACC: cribriform, tubular, and solid. Cribriform pattern foci are generally constant even when a different histological tumor type predominates. The cribriform pattern is the most common and associated with the best prognosis, whereas the solid type is less frequent but has a poorer prognosis(3,7,8).
The most appropriate approach to the management of lacrimal sac tumors depends more on the tumoral size and the general condition of the patient rather than the histological type(5). The classical treatment of malignant lacrimal sac tumors has been complete excision of the tumor and lacrimal drainage system, including the canaliculi and nasolacrimal duct, followed by radiotherapy and/or adjuvant chemotherapy(1,9). At present, a multidisciplinary approach to disease treatment is essential in obtaining the best clinical outcomes(11). The need to perform orbital exenteration versus more conservative surgery should always be evaluated individually, as exenteration does not ensure a better prognosis(2) and causes substantial facial disfigurement that may lead to severe psychological and psychiatric disorders.
Following appropriate treatment, patients must undergo lifelong follow-up given the high rate of local recurrence of lacrimal sac tumors(11). Because of the poor specificity of clinical symptoms, clinicians must have a high degree of suspicion to arrive at a prompt definitive diagnosis. Lacrimal sac tumors should be considered in any patient with chronic epiphora or dacryocystitis who does not respond to standard treatments. Radiological studies with DCG, Computed Tomography (CT)-DCG, CT, and magnetic resonance imaging are essential in ruling the possibility of a lacrimal sac tumor(1,5). In any case, pathological examinations are required for a definitive diagnosis of lacrimal sac tumor(4).
CONCLUSION
Lacrimal sac tumors should be considered in any case of epiphora or dacryocystitis that does not improve with dacryocystorhinostomy. Imaging studies are required to rule out the presence of a lacrimal drainage system tumor.
The finding of a mass or gelatinous tissue during dacryocystorhinostomy may require termination of the procedure or performance of a biopsy and imaging studies to rule out the existence of neoplasia(11).
Ophthalmologists should be aware of the characteristic triad of primary lacrimal sac tumors, which includes the clinical findings of persistent dacryocystitis or epiphora, an irreducible mass, and abnormal dacrycystography. Delayed diagnosis may worsen the prognosis of this rare type of malignant tumor.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

