INTRODUCTION
Toxoplasmosis is the leading cause of infectious posterior uveitis worldwide, accounting for 80% of the cases in some regions(1). Although toxoplasmic retinochoroiditis usually has a self-limiting course, it can lead to an irreversible visual loss, particularly when the macula and optic nerve head are involved. Vascular involvement typically consists of diffuse or segmental sheathing produced by antigen-antibody complex deposition in the vessel wall, as well as by localized mononuclear cell infiltrates(1). Retinal vein occlusion may occur, but artery obstruction is rare(2-4). We herein report an atypical presentation of toxoplasmic retinochoroiditis characterized by the occurrence of combined branch retinal vein and artery occlusion.
CASE REPORT
A 22-year-old healthy man complained of low visual acuity and pain in his left eye [oculus sinister (OS)] for five days. His past ocular and family history were unremarkable. Best-corrected visual acuity (BCVA) was 20/20 in the right eye [oculus dexter (OD)] and 20/400 in the left eye (OS). His anterior segment examination was normal OD and revealed 2+ anterior chamber reaction OS. Intraocular pressure by applanation tonometry was 10 mmHg in both eyes at 08:00. Funduscopy showed a normal OD and a white, poorly demarcated, and slightly elevated retinal lesion at the proximal portion of the inferotemporal vascular arcade OS. There were retinal hemorrhages in the inferotemporal region extending to the periphery with venous dilation and increased tortuosity, as well as ischemic retinal whitening along the inferotemporal vascular arcade, 2+ vitreous cells, and diffuse periphlebitis. The striking macular appearance was reminiscent of viral retinitis, given its necrotic and hemorrhagic features (Figure 1).
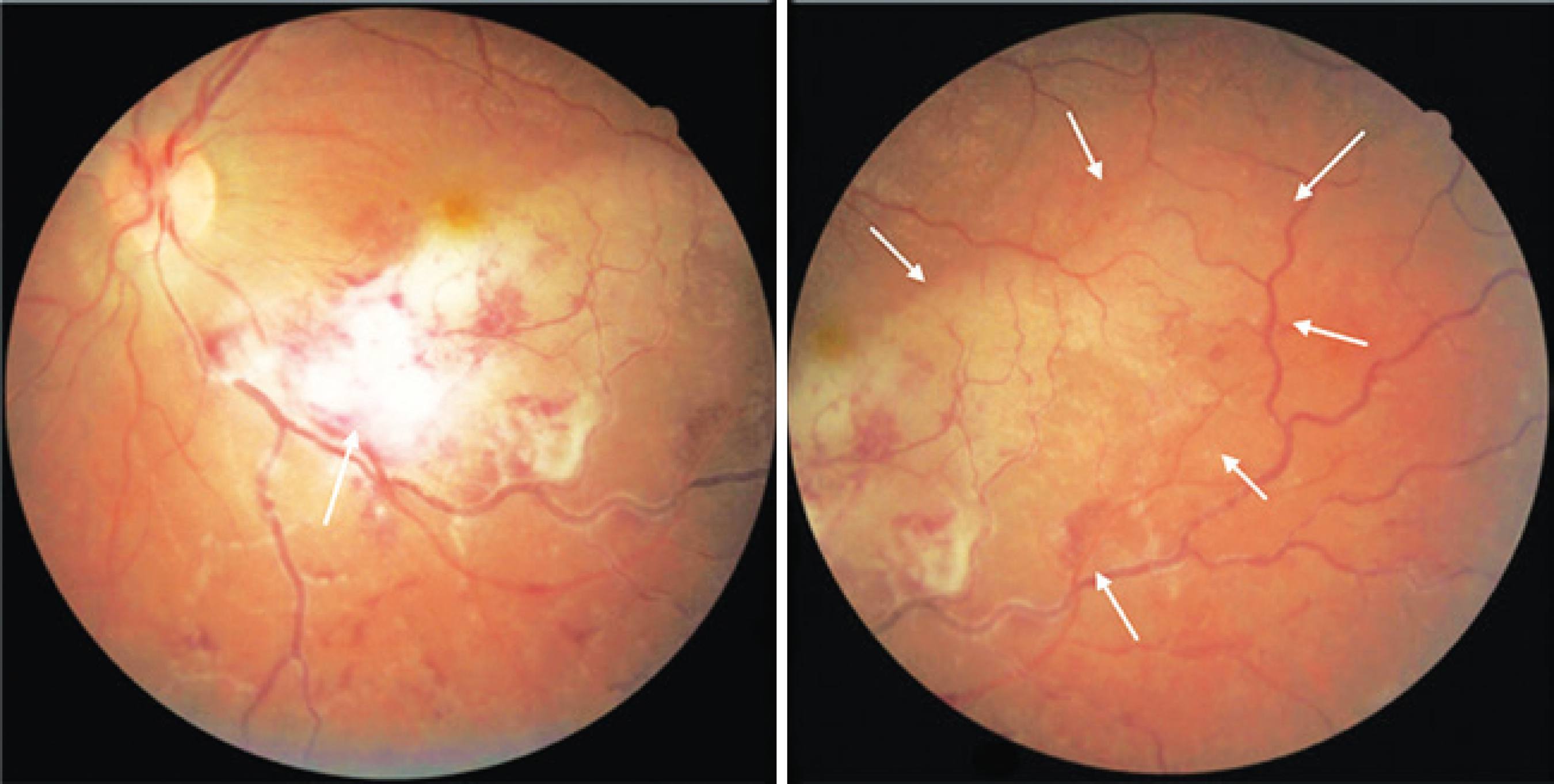
Figure 1 Initial presentation: Fundus photography of the left eye showing a white, poorly demarcated, and slightly elevated retinal lesion at the proximal portion of the inferotemporal vascular arcade (arrow, left). There were retinal hemorrhages in the inferotemporal region extending to the periphery with venous dilation and increased tortuosity, as well as ischemic retinal whitening along the inferotemporal vascular arcade (arrows, right), 2+ vitreous cells, and diffuse periphlebitis.
Blood tests revealed normal leukocyte and erythrocyte counts and erythrocyte sedimentation rates. Serological tests for human immunodeficiency virus (HIV) and syphilis (venereal disease research laboratory and fluorescent treponemal antibody absorption tests) were negative. Chest X-ray films were normal. Toxoplasma immunoglobulin (Ig) G antibodies were positive in an enzyme-linked immunosorbent assay (132 IU/mL), whereas anti-toxoplasma IgM antibodies were negative.
Two days after initial presentation, the patient was started on pyrimethamine at 50 mg daily, sulfadiazine at 2 g daily, folinic acid at 15 mg three times a week, prednisone at 60 mg daily, in a tapering schedule, as well as topical prednisolone acetate 1% and tropicamide 1%. Five days later, BCVA was maintained, and the ophthalmologic examination did not reveal any changes. Three weeks later, BCVA was 20/150 OS. His anterior segment examination was unchanged OD and showed 1+ anterior chamber reaction OS. Intraocular pressure was 16 mmHg OD and 14 mmHg OS. Funduscopy was unchanged OD and showed a well-demarcated, whitish inferotemporal retinochoroidal lesion. There was sheathing of the inferotemporal retinal artery, mild juxtafoveal inferior retinal whitening, a macular star, and 1+ vitreous cells (Figure 2, left). Six weeks after the beginning of treatment, BCVA was 20/30 OS. There was no anterior chamber or vitreous cells. The inferotemporal retinochoroidal lesion showed signs of scarring (Figure 2, middle). Oral medication was discontinued, and the prednisolone acetate 1% drops were tapered.
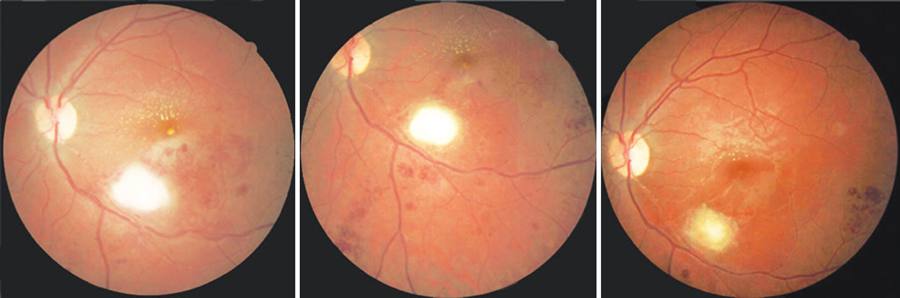
Figure 2 Fundus photography of the left eye at three weeks (left), six weeks (middle), and three months (right) after the beginning of treatment showing progressive improvement of the inferotemporal retinochoroidal lesion with complete scarring at the time of the last visit. A macular star is observed, as well as sheathing of the inferotemporal artery and numerous scattered hemorrhages. Periarterial plaques known as Kyrieleis arteritis can also be noted alongside the inferotemporal artery.
Three months after the initial presentation, BCVA was 20/30 OS. His anterior segment examination revealed no changes. The intraocular pressure was 16 mmHg OD and 15 mmHg OS. Funduscopy showed an inferotemporal retinochoroidal scar and partial resolution of the macular star (Figure 2, right). Fluorescein angiography revealed focal hypofluorescence with surrounding early hyperfluorescence corresponding to the inferotemporal scar and blocked hypofluorescence corresponding to the retinal hemorrhages. No areas of non-perfusion were detected (Figure 3). Optical coherence tomography showed signs of partial posterior hyaloid detachment, inferior macular inner and middle retinal atrophy, hyperreflective intraretinal dots superior to the fovea corresponding to the hard exudates, as well as a mild foveal discontinuity of the outer retina and pigment epithelium layer (Figure 4).
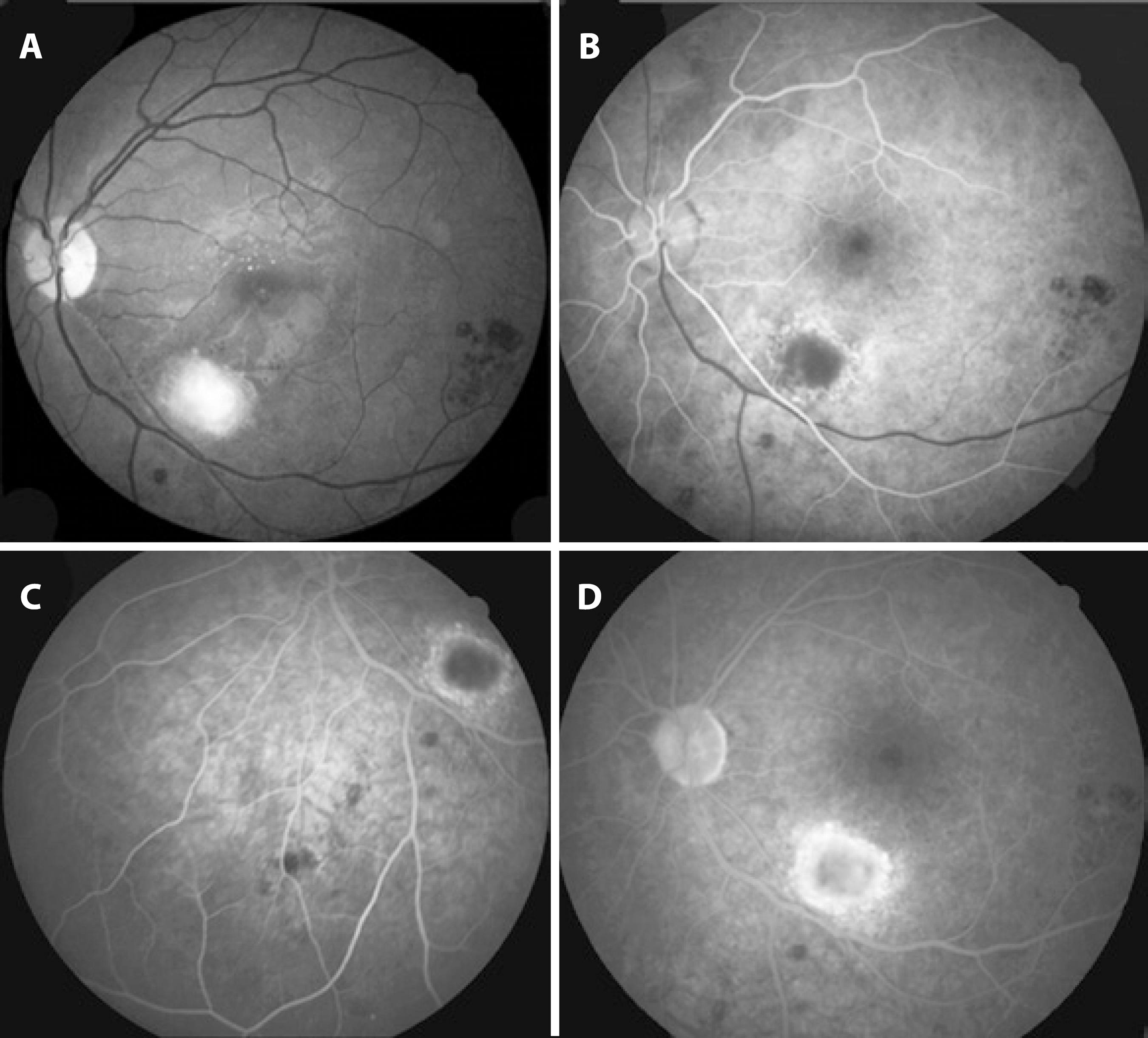
Figure 3 Fluorescein angiography (FA) frames of the left eye three months after the beginning of treatment. (A) Red-free fundus photography. (B) Early FA frame disclosing hypofluorescence corresponding to the inferotemporal lesion surrounded by early hyperfluorescence. (C) Intermediate FA frame of the inferior region. No areas of non-perfusion are observed. (D) Late FA frame showing no leakage at the macular region. Blocked hypofluorescence is seen corresponding to the scattered retinal hemorrhages.
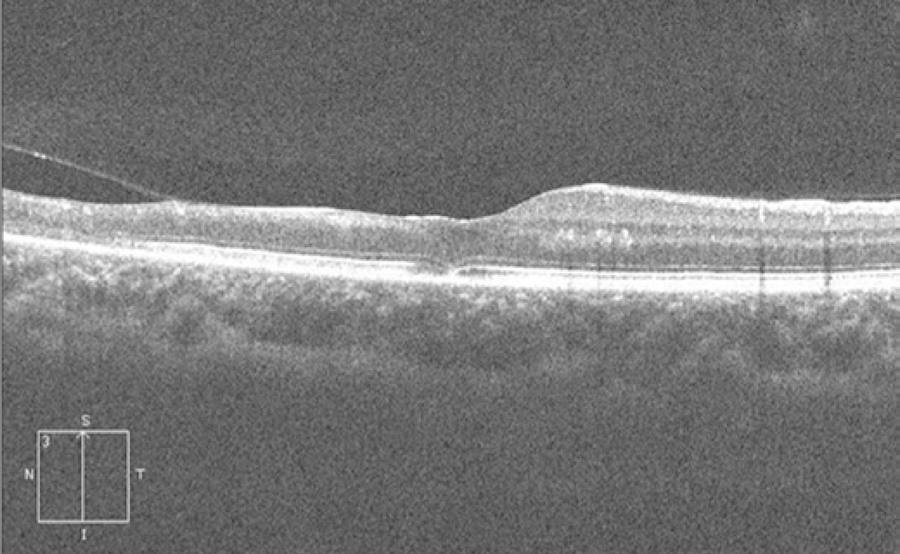
Figure 4 Vertical cross-sectional optical coherence tomography image of the left eye showing signs of partial posterior hyaloid detachment, inferior macular inner and middle retinal atrophy, hyperreflective intraretinal dots superior to the fovea, as well as mild foveal discontinuity of the outer retina and pigment epithelium layer.
DISCUSSION
The diagnosis of ocular toxoplasmosis is usually straightforward; however, challenging cases may occur. In the case presented here, vascular occlusion of the inferotemporal retinal artery and vein led to unusual fundus findings characterized by ischemic retinal whitening and numerous scattered retinal hemorrhages obscuring the boundaries of the focal inflammatory lesion. The appearance of the fundus resembled viral retinitis. Considering the high prevalence of toxoplasmosis in Brazil(5), the health status of the patient, and absence of peripheral retinitis, toxoplasmosis was strongly suspected. An anti-toxoplasma medication was introduced, and the patient was closely followed.
Ocular toxoplasmosis begins in the superficial retina. As retinitis progresses, the involvement of full-thickness retina, adjacent choroid, vitreous, and even sclera may occur. The initial lesion with ill-defined margins due to retinal edema tends to become more defined with treatment. After a variable time period, pigmentation mainly occurs in the lesion margins(1). These findings were observed in our case.
Vascular changes in toxoplasmosis typically involve veins, but arteries may also be affected, particularly in the form of Kyrieleis arteritis(1), characterized by nodular periarterial plaques that were observed in our case (Figure 2). Although classically described in toxoplasmosis, Kyrieleis arteritis may occur in syphilis, rickettsial retinal vasculitis, acute retinal necrosis, and other diseases. Its presence should raise suspicion of an infectious cause of retinal vasculitis(1).
Branch artery occlusion may result from direct artery compression by retinochoroiditis or by arteriolar contraction associated with increased viscosity of blood and inhibition of coagulation due to heparin release from mast cells as a response to acute inflammatory stimuli. It may also be a consequence of perivasculitis, which may cause thickening of the vessel wall, disruption of blood flow, and thrombosis(6). Yu et al.(7) identified the following three patterns of retinal capillary ischemia using optical coherence tomography in arterial occlusive disease in the acute phase: (1) thickening and hyperreflectivity of the inner retinal layers owing to ischemia of the superficial capillary plexus, (2) hyperreflective band at the level of the inner nuclear layer representing ischemia of the intermediate and deep capillary plexuses, and (3) diffuse thickening and hyperreflectivity of the inner and middle retinal layers representing both superficial and deep capillary ischemia. In the chronic phase, thinning and atrophy of the affected retinal layers were seen. In our case, optical coherence tomography in the chronic phase revealed inner and middle inferior retinal macular atrophy, consistent with both superficial and deep capillary ischemia.
Atypical forms of ocular toxoplasmosis include punctate outer retinal toxoplasmosis, neuroretinitis, neuritis, pseudomultifocal retinochoroiditis, multifocal retinochoroiditis, peripheral lesions, and anterior uveitis(1). Atypical presentations have been reported in patients with HIV infection, iatrogenic immunosuppression, or advanced age(8). Moshfeghi et al. reported findings on 25 eyes with widespread retinochoroiditis mimicking acute retinal necrosis(8). In their cases, lesions were atypical, large, multifocal, bilateral, or associated with diffuse retinal involvement or panophthalmitis. The diagnosis of toxoplasmosis was confirmed by the response to anti-toxoplasmosis medications, intraocular diagnostic studies such as polymerase chain reaction, intraocular antibody analysis, ocular fluid culture, or histopathological examination identifying Toxoplasma gondii in necrotic retinal tissue.
In conclusion, we report an uncommon presentation of toxoplasmosis, characterized by combined branch artery and vein occlusion, resulting in ischemic retinal whitening and numerous scattered retinal hemorrhages in the inferotemporal region along with a poorly defined proximal whitish retinal lesion. The possibility of toxoplasmosis in cases presenting with these features must be considered because prompt treatment may prevent a poor visual outcome.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

