INTRODUCTION
Keratoconus is a bilateral, asymmetric, non-inflammatory, and slowly progressive corneal disease with an approximate incidence of 1 in 2000 individuals. This condition is characterized by corneal thinning and protrusion, progressive myopia, and irregular astigmatism(1) and has conventionally been treated using modalities, such as rigid contact lenses, intrastromal corneal ring segment implantation, and keratoplasty. However, current treatment objectives include not only improved visual acuity but also the prevention of disease progression(2). Accordingly, corneal cross-linking (CXL) is a relatively new treatment method designed to increase the mechanical and biochemical strength of the stromal tissue via exposure of the ectatic cornea to riboflavin and ultraviolet-A (UVA) light(3). This procedure is the only currently available semisurgical therapeutic approach for patients with progressing keratoconus and has been shown to delay or even stop the progression of corneal ectasia, thus reducing the need for keratoplasty(4).
A minimum safety limit is defined as 400 µm for corneal preoperative thickness to avoid damage of ultraviolet A (UV-A) irradiation to endothelium, lens, and deeper structures(5,6).
Different CXL techniques for thin corneas have been developed, including transepithelial CXL(7) and CXL with customized pachymetric-guided epithelial debridement preserving the epithelium in thinner corneal regions(8). Alternatively, the induction of iatrogenic corneal swelling via the administration of hypo-osmolar riboflavin solutions before CXL application has been proposed as an alternative method for corneas thinner than 400 µm(9). However, the duration of thickening induced by hypo-osmolar solutions is controversial, given that some reports indicate a failure of this effect to persist throughout the procedure, thus rendering deeper structures vulnerable to possible side effects from ultraviolet light exposure towards the end of the procedure(10). Notably, a recently introduced iso-osmolar riboflavin solution that contains hydroxymethylcellulose instead of dextran is considered a possible alternative to hypo-osmolar solutions in cases with thin corneas.
In the present study, changes in visual acuity and refractive and topographic outcomes were analyzed after CXL treatment performed with this newly introduced dextran-free, isotonic riboflavin solution.
METHODS
Twenty-six eyes of 26 patients (12 males, 14 females; mean age: 25.1 ± 4.6 years, range: 18-33 years) with progressive keratoconus who underwent CXL between September 2012 and October 2013 at Necmettin Erbakan University Meram Faculty of Medicine were included in this study. The local ethics committee approved this study, which adhered to the tenets of Declarations of Helsinki, and informed consent was obtained from all patients. The inclusion criteria were keratoconus with documented progression in the past 12 months, defined as an increase in maximum keratometry (Kmax) of 1.00 diopter (D) or more in the previous 12 months; corneal thickness of at least 400 µm at the thinnest point; age of at least 18 years; and patient-reported deterioration of visual acuity (excluding other possible non-corneal reasons for deterioration). The exclusion criteria were corneal opacity, previous ocular surgery, previous herpetic keratitis, active ocular infection, autoimmune disease, chemical injury, delayed epithelial healing, and lactation at the time of the study.
The CXL procedure was performed under sterile conditions in a surgical room according to the following description. After administering 0.5% propacaine drops (Alcaine; Alcon Pharmaceuticals, Fribourg, Switzerland) as a topical anesthestic, the corneal epithelium was removed by mechanical debridement over the central 8.0 mm. A dextran-free isotonic riboflavin solution [>0.1% riboflavin with 1.1% hydroxypropylmethylcellulose (MedioCROSS M; Kiel, Germany)] was applied to the cornea every 3 min for 30 min. After 30 min, UVA (370 nm, 3 mW/cm2 intensity) was applied to the cornea (CCL-VARİO; Peschke Meditrade GmbH, Huenenberg, Switzerland) for 30 min. Application of the riboflavin solution continued every 3 min during irradiation. Ultrasound pachymetry (OcuScan RxP; Alcon Laboratories, Inc., Fort Worth, TX, USA) was performed on the de-epithelialized cornea at approximately the thinnest point, which had been determined preoperatively from a corneal pachymetry map obtained via corneal topography. Three repeated measurements were taken by the same surgeon (RO) after de-epithelization, at 15, 30, and 45 min into the procedure, and at the end of the procedure. For each, the average of 10 measurements was taken, and the mean value obtained from the 3 measurements was used for the evaluation. Topical anesthetics were added as needed during the procedure. Postoperatively, a bandage contact lens (PureVision (balafilcon A); Bausch & Lomb, Rochester, NY, USA) was placed, and levofloxacin and dexamethasone eyedrops were administered 4 times daily until epithelization was complete.
At baseline and each of the postoperative follow-up examinations (1, 3, 6 months), all patients underwent ophthalmological evaluations to measure the best corrected visual acuity (BCVA), refraction (spherical equivalent, diopters; D) and corneal topography (Pentacam; Oculus GmbH, Wetzlar, Germany). The preoperative and postoperative K-readings of Kmax and mean simulated keratometry (Sim K) were assessed from topography data.
All variables were found to be normally distributed according to the Kolmogorov-Smirnov test. The statistical power analysis yielded a power of approximately 35%. The Friedman two-way analysis of variance test was used to compare preoperative and postoperative data. Following a Bonferroni correction, a p value of <0.0083 was considered statistically significant in comparison tests.
RESULTS
The mean baseline BCVA was 0.51 ± 0.2 (Snellen lines), and the corresponding readings after CXL were 0.48 ± 0.2, 0.57 ± 0.2, and 0.64 ± 0.2 at the 1-, 3-, and 6-month follow-ups, respectively. A significant difference was observed between the baseline and 6-month postoperative BCVA values (p=0.006; Figure 1). The preoperative mean spherical equivalent (SEQ) refraction was -5.6 ± 2.4 D; although this parameter decreased to -5.0 ± 2.1 D at the last follow-up (SEQ change=0.59 D), this change was not statistically significant (p=0.145; Figure 2). In other words, an inverse relationship was observed between the SEQ and BCVA values.
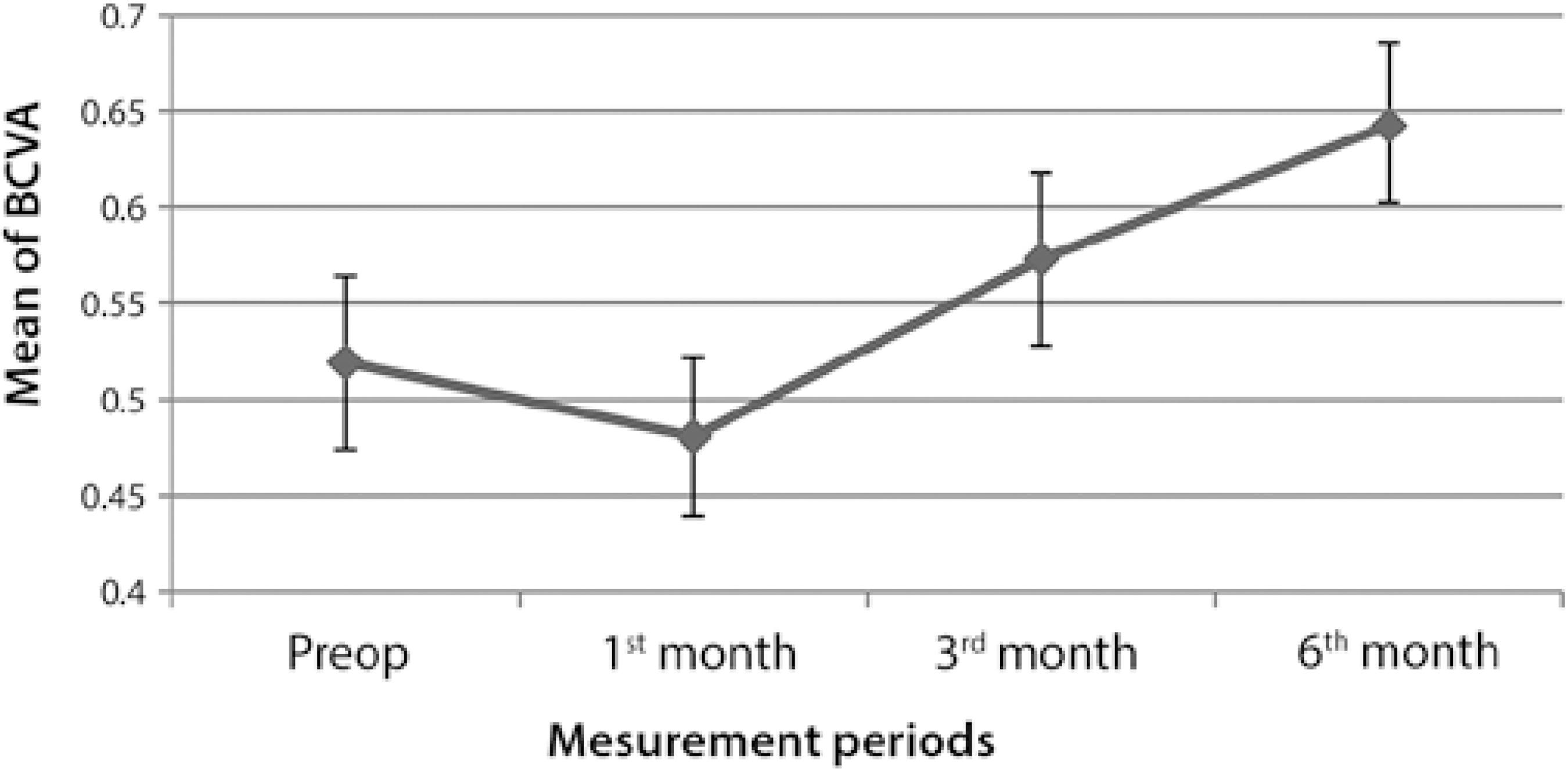
BCVA= best corrected visual acuity.
Figure 1 Graph representing changes in best corrected visual acuity over time.
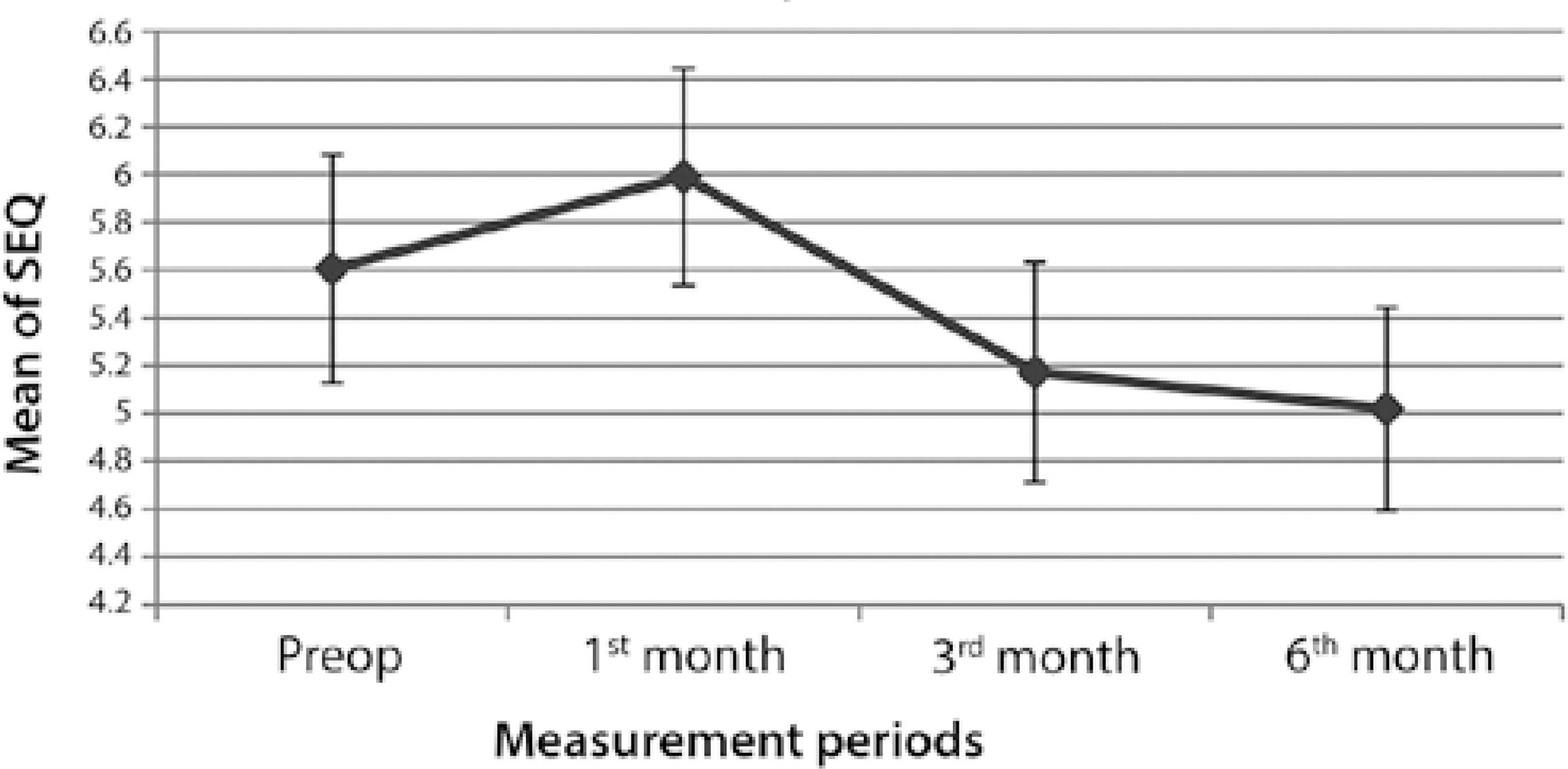
SEQ= mean spherical equivalent.
Figure 2 Graph representing changes in spherical equivalent refractive values of the eyes over time.
Compared with the baseline, the mean Sim K increased slightly during the first postoperative month (p=0.407), followed by a decrease at the 3-month follow-up (p=0.361) and subsequent plateau from 48.5 ± 2.5 D to 47.8 ± 2.6 D at the 6-month follow-up (p=0.001). The mean Kmax exhibited a progressive decrease over 6 months, and this change represented a significant difference from the baseline value (p=0.003; Figure 3).
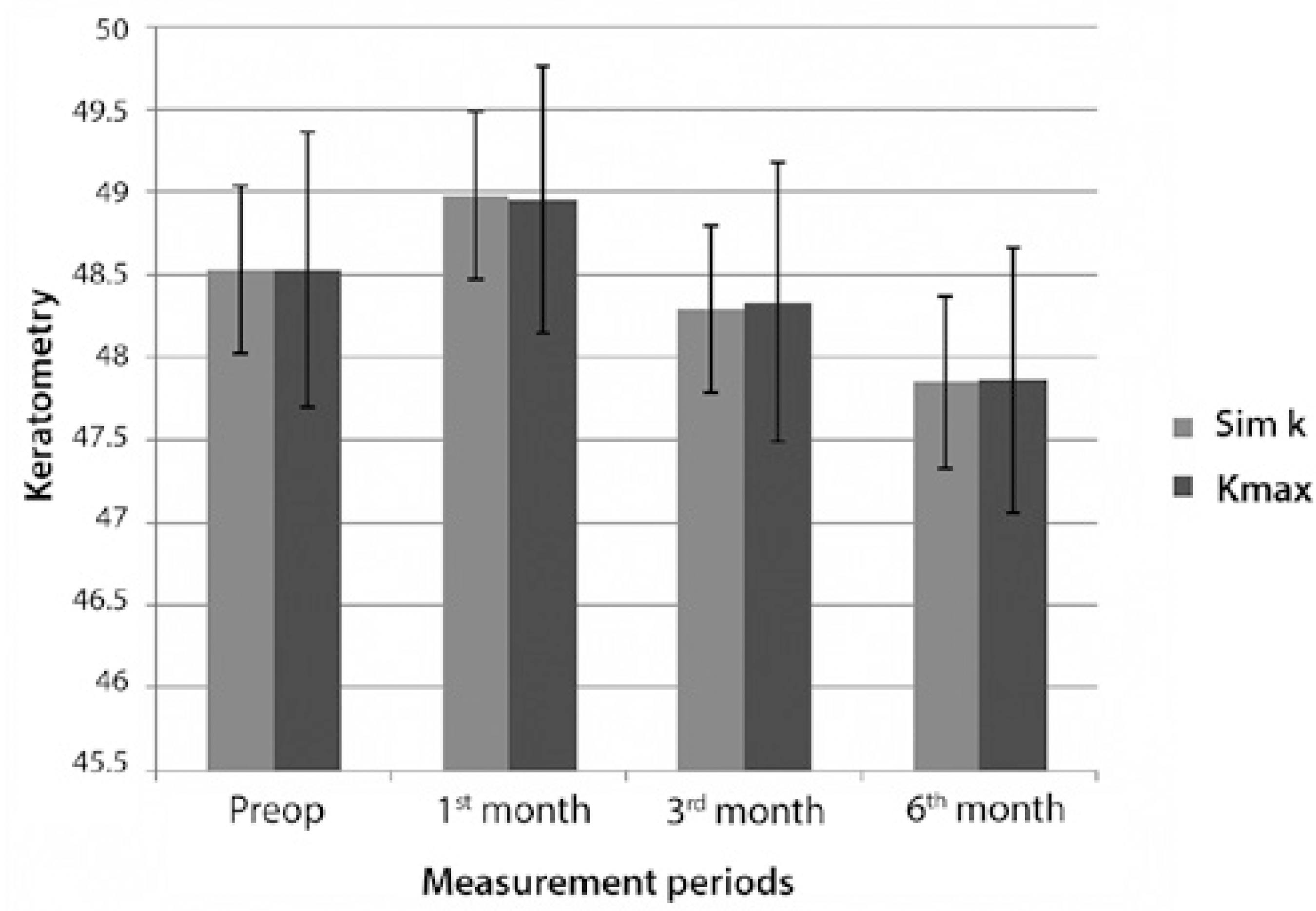
Sim K= average simulated keratometry; Kmax= maximal keratometry.
Figure 3 Bar graph demonstrating the Kmax and Sim K values (measures of keratoconus) before surgery and at 1, 3, and 6 months after corneal crosslinking.
Before surgery, the central corneal thickness (CCT) and minimal corneal thickness (MCT), including the epithelium, were 442.8 ± 25.6 µm and 430.5 ± 23.9 µm, respectively. These values decreased to 417.6 ± 31.9 µm and 407.2 ± 31.1 µm, respectively, at 3 months but subsequently increased to 420.7 ± 31.8 µm and 409.3 ± 28.7 µm, respectively at 6 months. Notably, the differences between the preoperative and postoperative CCT and MCT values were statistically significant at every time point during follow-up (p<0.001; Figure 4). At baseline, the mean preoperative MCT, including the epithelium, measured 430.5 ± 23.9 µm; this was reduced to 396.8 ± 21.3 µm after removal of the epithelium. After the application of dextran-free isotonic riboflavin solution, the MCT exhibited a steady increase at the 15-, 30-, 45-, and 60-min time points during the procedure (422.3 ± 19.1 µm, 450.4 ± 14.9 µm, 459.1 ± 15.7 µm, and 464.9 ± 15.5 µm, respectively).
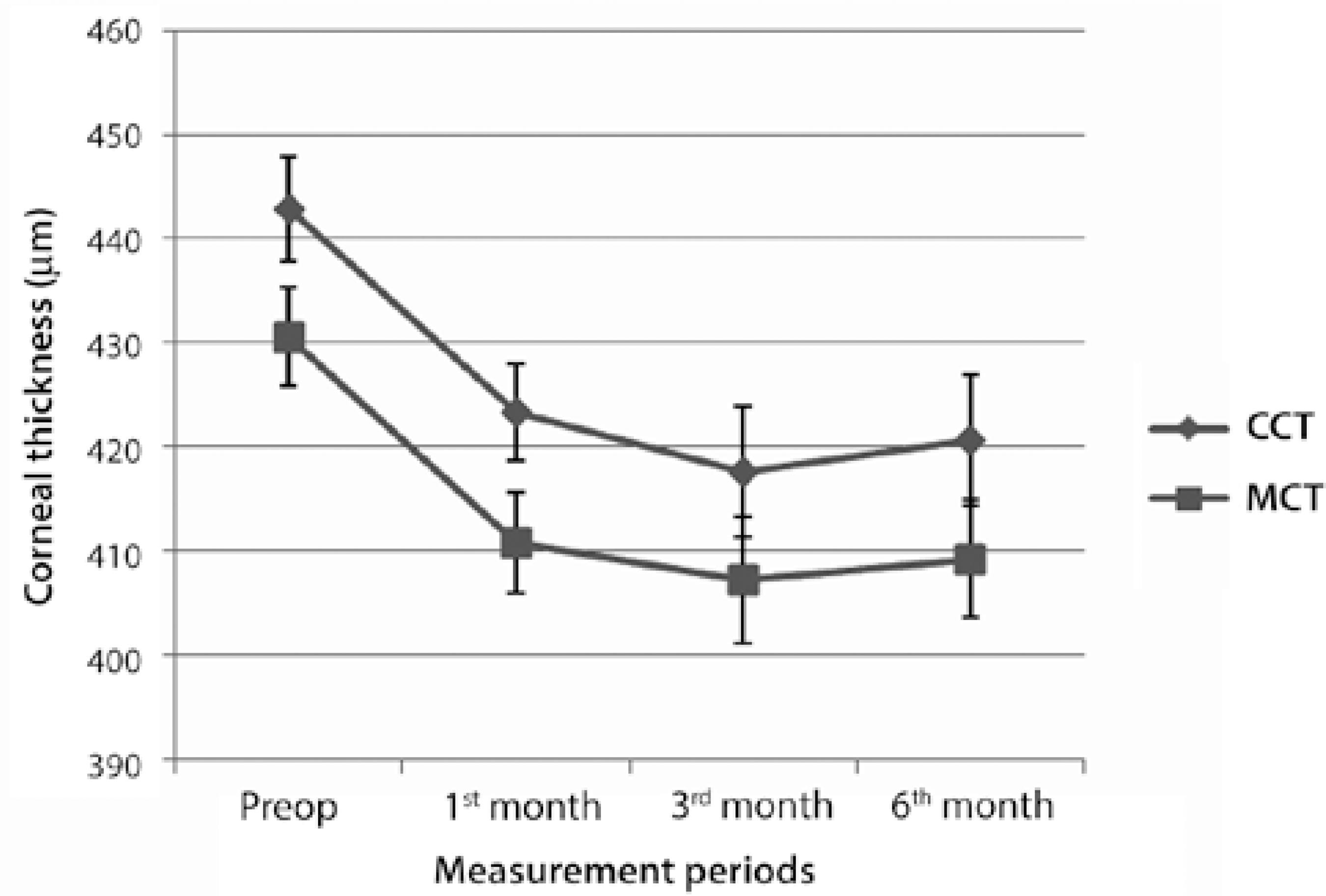
CCT= central corneal thickness; MCT= minimal corneal thickness.
Figure 4 Changes in the central corneal thickness and minimum corneal thickness measurements over time in patients with keratoconus.
No eye exhibited a sterile or infectious infiltrate in the corneal stroma after surgery, and no complications were observed after the application of dextran-free isotonic riboflavin solution. All corneas demonstrated normal progression with respect to the epithelial healing process. At the final follow-up examination (6 months after CXL), all corneas were transparent, with no detectable stromal scarring.
DISCUSSION
Riboflavin-induced ultraviolet-light CXL has received a significant amount of attention in recent years. Previous studies have demonstrated the safety and efficacy of CXL for preventing the progression of keratoconus(10-12). In this procedure, riboflavin serves as a photosensitizer for crosslink induction and protects the underlying tissues from the deleterious effects of UVA irradiation; in addition, it prevents corneal dehydration during the operative procedure(13). In cases with particularly thin corneas, a 0.1% hypo-osmolar riboflavin solution can also be applied to artificially swell the cornea to a thickness of at least 400 µm before CXL, thus reducing the risk of UVA-induced endothelial cytotoxicity(9).
According to an earlier protocol described by Hafezi et al., UVA treatment was administered after inducing iatrogenic corneal swelling with hypo-osmolar riboflavin solution to a minimum corneal thickness of 400 µm, a procedure that was found to efficiently increase the stromal thickness by 25% after 30 min(9). In this procedure, the application of iso-osmolar riboflavin solution continued during UVA irradiation. This led to concerns regarding the durability of corneal thickness throughout the procedure such as those raised by Kaya et al., who suggested that the iatrogenic swelling induced by a hypo-osmolar riboflavin solution might be short-acting and thus would not persist throughout UVA application, following an observed decrease in the corneal thickness upon the installation of the iso-osmolar riboflavin solution(10).
Previous studies and the standard CXL procedure have generally used an iso-osmolar riboflavin 0.1% solution containing 20% dextran (402.7 mOsmol/L), which exerts a temporary dehydrating effect and consequent corneal thinning. In contrast, we performed the CXL procedure with a dextran-free isotonic riboflavin solution and observed that the corneal thickness increased throughout the procedure, in agreement with the results of a previous study(14). However, the safety CXL in the presence of an artificially swollen cornea remains controversial because the lower concentration of collagen fibers in the hydrated stroma is expected to weaken the crosslinking effect of UVA, as demonstrated in experiments with collagen gels(15).
The current study aimed to analyze the variables related to short-term outcomes in a group of patients with keratoconus who were treated via corneal CXL with a dextran-free isotonic riboflavin solution. After an initial worsening of all keratoconus indices and BCVA, likely due to epithelial debridement, continuous improvements were observed in most keratometric and topographic indices for up to 6 months after surgery. In previous studies, BCVA has been reported to improve by 2 Snellen lines at 36 months and 1.05 Snellen lines at 12 months after CXL(12,16). In another study, Goldich et al. observed a significant improvement in the BCVA (0.21 ± 0.1 to 0.14 ± 0.1; p=0.002)(17). Our results demonstrated a significant improvement of 1.03 Snellen lines in the BCVA at 6 months.
A previous study conducted by Wittig-Silva et al. failed to exhibit changes in the SEQ or the spherical or cylindrical component of subjective refraction(18). However, other studies have reported changes in SEQ ranging from +0.40 D to +2.13 D(12,19,20). Similarly, Caporossi et al. observed a decrease in the SEQ value of 2.21 D at 3 months after CXL(21), and Wollensak et al. reported a significant improvement of 1.14 D in the average SEQ at 6 months postoperatively(11). In our study, we observed a mean improvement in the SEQ of 0.6 D at the 6-month follow-up; in addition, this was the lowest SEQ observed in this study. However, the change in this parameter failed to reach statistical significance, possibly as a result of the limited number of patients in our study.
With respect to corneal curvature, we observed significant reductions in the mean Kmax and Sim K values of 1.26 and 0.73 D, respectively, at 6 months postoperatively. Caporossi et al. reported similar results, with a postoperative average reduction in the mean keratometry measurement of 1.96 D(21). Similarly, Wollensak et al. reported a reduction in the mean keratometry reading of 2.01 D(11).
Similar to previous studies, the corneal thickness decreased from the preoperative to the final time point, indicating corneal compaction(20,22,23). In our study, statistically significant differences between the pre- and postoperative measurements were detected when the corneal thicknesses at the apex of the keratoconus (MCT) and pupil center (CCT) were measured. Notably, the CCT initially decreased significantly from the baseline up to the 3-month time point but exhibited significant improvement at the 6-month follow-up. The MCT values similarly decreased from the baseline, although the 6-month value remained significantly below the preoperative value.
To the best of our knowledge, the outcomes of CXL treatment with a dextran-free isotonic riboflavin solution have not been reported previously. This study demonstrated improvements in outcomes related to keratometry and visual acuity in patients undergoing CXL with a dextran-free isotonic riboflavin solution, similar to the improvements observed in patients from previous studies who were treated with dextran-containing solutions. Furthermore, we reported that the use of a dextran-free iso-osmolar riboflavin solution during CXL induced a steady increase in corneal thickness throughout the procedure. This finding might be beneficial with respect to an increased indication for CXL in patients with thin corneas, as it removes the concern of unpredictable intraoperative thinning below the safety margin reported in our other study(14). We note that the improvements in visual acuity and keratometry readings were found to occur progressively throughout the postoperative follow-up period, suggesting that a longer follow-up is needed to determine the total functional and anatomic effects of CXL and to obtain stable functional and keratometric values. The small number of subjects in the study group, lack of a control group comprising patients treated with a standard dextran-containing riboflavin solution, and the short follow-up period were limitations of our present study.
In conclusion, this study has demonstrated the safety of CXL with a dextran-free isotonic riboflavin solution for the treatment keratoconus. This procedure was found to yield good visual results and to reduce disease progression, as well as iso-osmolar solutions containing dextran.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

