INTRODUCTION
Varicella zoster virus (VZV), a ubiquitous human alpha-herpes virus, is a member of the Herpesviridae family(1). Following primary infection with VZV (chicken pox), the immune response protects against reinfection on re-exposure to VZV. However, when cell-mediated immunity declines through aging or immunosuppression, VZV can reactivate in the sensory ganglia, causing herpes zoster (HZ), which is the secondary (recurrent) form of the disease(2,3).
Age also appears to be important in the natural history of HZ infection. It is known, for example, that HZ affects >50% of individuals by 80 years of age(4) and that there is an increased prevalence of impaired immunity due to systemic disorders or immunosuppressive therapy(5,6). Considering that the number of people aged ≥60 years is projected to double over coming decades, the number of HZ cases is also expected to increase substantially.
A diagnosis of HZ is primarily based on the history and clinical findings(7), with laboratory confirmation unnecessary in all but specific patient populations(8). Definitive proof of HZ requires viral antigen detection using direct fluorescent antibody or polymerase chain reaction (PCR). The virus can be detected in cutaneous lesions, cerebrospinal fluid (CSF), bronchoalveolar lavage fluid, saliva, and aqueous humor, as well as in blood, corneal, retinal, and vitreous fluids(9-13). Although direct fluorescent antibody is more frequently used for the diagnosis of VZV, it is less specific and sensitive than PCR, and even less effective for early diagnosis. PCR of the CSF can detect VZV within 1 week of infection onset and can remain positive for 14-50 days(10,14).
HZ ophthalmicus (HZO) is 20 times more common when compared with either mandibular or maxillary infection(2,15), being exceeded only by thoracic zoster(16). As shown in table 1, there are several potential complications associated with HZO, and these can affect either the skin, anterior ocular segment, optic nerve, retina, or central nervous system(7). HZ infection can also occur in the absence of cutaneous involvement(17,18), as is seen in zoster sine herpete.
Table 1 Acute and chronic features of herpes zoster ophthalmicus
| Ocular structure | Clinical features | |
|---|---|---|
| Acute | Chronic | |
| Lids and ocular adnexa | Hyperemia | Lagophthalmos |
| Edema | Allodynia | |
| Rash | Ptosis | |
| Cicatricial skin changes | ||
| Loss of lashes | ||
| Conjunctiva | Conjunctivitis (pseudomembranous/ membranous/follicular) |
Symblepharon |
| Hypoesthesia | ||
| Ulcers | ||
| Hemorrhages | ||
| Cornea | Punctate epithelial | Corneal mucous plaques |
| Keratitis | Disciform keratitis | |
| Pseudodendrites | Neurotrophic keratitis | |
| Ulcers | Exposure keratitis | |
| Stromal infiltrates | ||
| Endotheliitis | ||
| Sclera | Episcleritis | Scleral atrophy and thinning |
| Scleritis | ||
| Uvea | Uveitis | Paralytic mydriasis |
| Hyphema | Iris atrophy | |
| Hypopyon | Posterior synechiae | |
| Retina | Retinitis | Cystoid macular edema |
| Acute retinal necrosis | Retinal detachment | |
| Progressive outer retina | Retina atrophy | |
| Necrosis | ||
| Optic nerve | Optic neuritis | Optic atrophy |
| Papillitis | ||
| Orbit and brains | Paralysis of eye movement | Strabismus |
| Diplopia | ||
| Vasculitis | ||
HZO is a serious and unpredictable disease that should always be treated with nucleoside analogs at the first sign of infection, preferably within 72 h of prodromal symptoms(19,20). Early acyclovir treatment (800 mg, five times a day) can reduce acute pain and the incidence of eye complications from 50% to 20%-30%(21). Valacyclovir (1000 mg t.i.d.) and famciclovir (500 mg t.i.d.), which are therapeutically equivalent, can also be used, and published recommendations on the management of HZ agree that antiviral therapy with either drug is preferable to acyclovir(20,22). Valacyclovir and famciclovir provide higher plasma concentrations of the acyclic nucleoside analog required to inhibit VZV, thus reducing acute viral shedding and minimizing neural damage. Further, these drugs have simpler dosing regimens and are associated with higher treatment adherence. Foscarnet is an alternative treatment option in special cases(23).
In addition to antiviral therapy, corticosteroid eye drops are recommended for severe inflammation caused by HZO, such as uveitis, and an oral corticosteroid may eventually be required(24). Moreover, oral or topical corticosteroids in combination with oral antivirals are the treatment of choice for recurrent and chronic HZO(25). However, the role of steroids in the management of HZ is controversial(24), and the results of a systematic review of their efficacy are awaited. Therefore, the use of corticosteroids to treat HZ without concomitant antiviral therapy is not recommended(23).
Following HZO, ocular complications associated with poor visual outcomes include acute corneal lesions, retinitis, optic neuritis, and uveitis(26). Patients may also develop postherpetic neuralgia, scleritis, or ocular palsies(27). Overall, these may cause permanent visual loss and substantial health care utilization. Moreover, diseases in immunocompromised patients are unpredictable and associated with unfavorable outcomes(28).
VZV vasculopathy
HZ infections were first discovered to be associated with neurologic VZV vasculopathy in 1919, when it was described as a late contralateral hemiplegia following stroke(29). Since then, there have been numerous reports of infarcts in the cerebrum, cerebellum, midbrain, and pons after HZ or varicella infection(30). More recently, active viral infection has been shown in large and small arteries of patients with VZV vasculopathy(31), leading to the clinical spectrum expanding beyond typical hemiplegia to include other signs and symptoms, such as headache, fever, cognitive changes, transient ischemic attacks (TIAs), temporal arteritis(32), and focal neurologic deficits(17) (Table 2). However, specific vascular involvement varies widely, and associated TIAs may also evolve into a variety of vascular events, including single, bilateral, or multiple ischemic/hemorrhagic infarcts; aneurysms; cerebral or subarachnoid hemorrhages(33-35); or infarcts of the basal ganglia or internal capsule(36).
Table 2 Warning signs and symptoms of zoster vasculopathy
| Alert signs and symptoms |
|---|
| Headaches |
| Fever |
| Mental status changes |
| Aphasia |
| Ataxia |
| Hemianopia |
| Hemisensory loss |
| Monocular visual loss |
| Acute hemiplegia |
The mean time from onset of HZ to vasculopathy is unclear, and although it is typically described as 5-12 weeks(37,38), it can range from a day to 2.5 years(14,38,39). The diagnosis of VZV vasculopathy differs from that for either HZ or HZO infection in that it is based not only on clinical signs but also on the results of imaging and serological examinations. The criteria for magnetic resonance imaging rely on the identification of deep-seated infarcts at the junction of the gray and white matter. Magnetic resonance angiography can also show focal stenosis and beading(14,34), with multiple segmental narrowing of any artery on the ipsilateral side to the affected dermatome(35,40).
Screening for VZV vasculopathy is performed using either anti-VZV testing [immunoglobulin (Ig) M and IgG] or PCR of the CSF and serum. Nagel et al.(14) compared the sensitivities of these testing methods for VZV vasculopathy and found that only 30% of subjects had DNA positive for VZV in the CSF, whereas 93% had anti-VZV IgG in the CSF, indicating the significant superiority of VZV antibody testing.
VZV vasculopathy should be suspected in patients presenting with a recent episode of HZ and stroke(s) of undetermined origin, particularly if the patient is immunocompromised. In addition, considering that 30% of patients have neither a rash nor CSF pleocytosis(14), the absence of a rash or the presence of normal CSF should not exclude the possibility of VZV vasculopathy. Recently, there have been reports of similar vascular events due to herpes simplex virus type 2 (HSV-2), and this should be considered in the differential diagnosis. Testing the CSF for HSV-2 DNA can help to differentiate one etiology from the other(41).
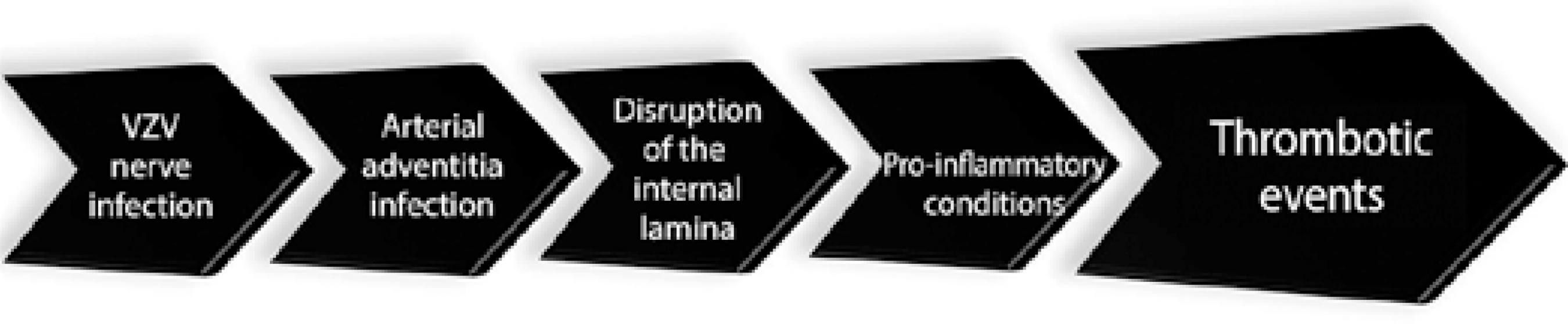
The vasculopathy mechanism was proposed initially as a varicella infection leading to a granulomatous angiitis(39,42,43). However, recent developments have shown evidence of direct VZV infection via ophthalmic branches the trigeminal nerve(44,45), which leads to transmural spread from the adventitia and later disruption of the internal elastic lamina, intimal hypertrophy, and proinflammatory conditions - all of which are related to an increased risk of thrombotic events(16). Large and/or small vessels can be affected(46), in 50% of the cases both vessels are involved(16). (Figure 1).
Originally, the mechanism underlying vasculopathy was believed to be a result of varicella infection causing a granulomatous angiitis(39,42,43). However, recent developments have shown that there is direct VZV infection via the ophthalmic branches of the trigeminal nerve(44,45), which subsequently causes transmural spread from the adventitia that disrupts the internal elastic lamina, causes intimal hypertrophy, and promotes inflammatory conditions, all of which increase the risk of thrombotic events(14). Large or small vessels can be affected(46), and both vessels are involved in 50% of reported cases (14).
HZO and vasculopathy: risk analysis
Major studies have been conducted to assess the relative risk of ischemic, thrombotic, or general vascular events related to zoster infections. Most agree there is a defined and significant risk among them(37,38,47,48), with general risk ratios ranging from 1.31 to 2.27(37,47,48). The risk ratios in these studies were extremely sensitive to the period after the zoster infection, zoster dermatome, treatment, and patient age at the time of infection.
When data obtained from patients with HZO were crossed with those of patients with vasculopathy events, the hazard ratios significantly increased(38). A comparison between 658 patients with HZO with 1,974 controls showed that there was a mean 4.52-fold increased risk of stroke. Kang et al.(47) and Langan et al.(37) reported mean increased hazard risks of 4.59-and 3.38-fold, respectively, when they analyzed only patients with HZO. Overall, the evidence indicates that the first year after zoster infection is critical, being associated with the greatest increased risk of stroke among patients with both HZ and HZO. The maximal risk appears to fall within the first 3 months after zoster infection, when the mean risk ratios for HZ and HZO range from 0.99-fold(37) to 2.27-fold(48) and from 0.82-fold(37) to 4.52-fold(38), respectively.
Multifocal temporal arteritis is another possible presentation of VZV vasculopathy. Termed multifocal VZV vasculopathy, it presents with the same clinical signs, symptoms, and laboratory findings as giant cells arteritis (GCA) and should be considered in cases of classic GCA where the temporal artery biopsy is negative(49).
Prompt diagnosis of VZV vasculopathy is imperative not only because it is a life-threatening condition with a mortality rate of 25%(50) if left untreated but also because the prognosis is benign when treated with intravenous acyclovir(51). Treatment typically involves 10-15 mg/kg of intravenous acyclovir three times daily for 10-14 days, with 1 mg/kg of prednisone administered intravenously or orally according to severity(34,35). In most reports, corticosteroid use has resulted in either improvement or maintenance of the prognosis(52) (Table 3)(53,54).
Table 3 Therapeutic approaches for herpes zoster ophthalmicus
| Drugs | Details | |
|---|---|---|
| Dosing | Indication | |
| Acyclovir | 800 mg PO 5 times a day for 7-10 days 10-15 mg/kg IV t.i.d for 10-14 days |
All cases of HZO Severe HZO |
| Valacyclovir | 1000 mg PO t.i.d for 7 days | All cases of HZO |
| Famciclovir | 500 mg t.i.d PO for 7 days | All cases of HZO |
| Foscarnet | 40 mg/kg t.i.d to 100 mg/kg b.i.d | Resistant HZO |
#= must always be combined with antiviral; HZO= herpes zoster ophthalmicus; PO= per os.
COMMENT
Although the risk for VZV vasculopathy is often high in patients with HZO(37,38,48,55), several risk factors need to be considered when making an assessment. These include age, sex, body mass index, smoking status, and cholesterol levels, as well as the presence of comorbid hypertension, diabetes, and vascular and heart diseases. The absence of an adjusted analysis in some reports(38,48) may also have resulted in bias, such as selection based on the records of compatible treatments for HZ(48), or public medical records, which both may lead to misclassification of zoster types(37,38). Thus, it is not currently possible to confirm whether these risk factors increase the severity of HZ vasculopathy, whether patients with HZ vasculopathy have a higher incidence of these risk factors, whether these are also risk factors for HZ vasculopathy, or whether there is any correlation between them.
Notwithstanding the disagreement among authors over whether the risk of VZV complications is directly attributable to VZV infection or whether they are merely independent vascular diseases associated with post-zoster infection, the severity of VZV vasculopathy should bring our attention to the need for a more aggressive HZ vaccination program. Indeed, HZ is preventable with vaccine administration(55), yet several authors only advocate HZ vaccination for patients with one episode of HZO(56), based on the rationale that most of these patients are older than 50 years and are already at an increased risk of vascular disease(57,58). However, this neglects the facts that prior vaccination reduces morbidity associated with HZ and is well tolerated(59). In general, primary care physicians usually recommend vaccination, but ophthalmologists may also need to play their role in preventing HZO. In the US, the cost of HZ vaccination was approximately $150 in 2009 (60), which limits general access. Although oral prophylaxis is routinely prescribed with either acyclovir or valacyclovir, no evidence-based guidelines have been produced that support the prolonged use of suppressive antivirals for chronic HZO and its complications(61).
Despite the possible benefits of vaccination and its good safety profile, complications have been reported(62). Demyelinating central nervous system diseases are perhaps the most widely reported, and optic neuritis is the most prominent, with symptom onset ranging from several hours after vaccination to as late as 3 weeks. Although the prognosis has been mostly good, several cases of poor visual outcomes have been reported(63). Other autoimmune diseases must also be considered in the differential diagnosis(64), including multiple sclerosis and neuromyelitis optica.
In this review, we analyzed the epidemiologic and clinical concepts of VZV infection and vasculopathy, and the peculiarities in relation to HZO. It is clear that VZV vasculopathy and HZO are related and that patients who present with HZO are at higher risk of developing VZV. However, making a diagnosis of VZV is not always easy, and it is essential that we educate the ophthalmology community on the systemic risks of VZV infections, particularly of stroke in patients with HZO. This is important because proper treatment with currently available antivirals can prevent death and provide better outcomes.
Preventing HZ vasculopathy is a controversial issue because it is not very prevalent. Nevertheless, a relative consensus agrees that vaccination may be important in preventing vascular events such as TIAs and strokes(37,57). In addition, because patients with HZO are already at an increased risk for vasculopathy, efforts should be made to reduce risk factors, including lifestyle habits such as smoking cessation as well as controlling obesity, cholesterol, and diabetes. Moreover, making a diagnosis of VZV vasculopathy is often complicated by the fact that neurologic disease can develop weeks or months after an episode of herpes zoster; that not all patients have a history of rash or chickenpox; that vasculopathies of other origins produce the same clinical, CSF, and imaging abnormalities; and that virological analysis is often limited(14).
The considerations outlined in this review indicate the importance of ophthalmologists in the management of HZO. Follow-up visits for these patients must be frequent, and clinicians should be vigilant for symptoms of VZV vasculopathy. Ophthalmologists should be alert to the onset of neurological signs and instruct patients to report any changes because early systemic antiviral therapy is frequently associated with a good prognosis.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

