INTRODUCTION
The ability to maintain the balance between cell death and the regeneration of the corneal surface depends on the reserve of stem cells located in the limbal region(1). Injury to these cells can result from mechanical or chemical damage causing total or partial limbal stem cell deficiency, unilaterally or bilaterally. This deficiency can cause various signs and symptoms, including corneal neovascularization and conjunctivalization, loss of the Vogt palisades, irregularity of the corneal epithelium, presence of goblet cells on impression cytology of the cornea, and decreased visual acuity.
Different surgical techniques have been proposed for the treatment of ocular surface diseases caused by limbal stem cell deficiency(2) (Table 1). In the case of unilateral presentation, the procedure of choice is conjunctival limbal autograft transplantation (CLAU), which involves the removal and transplantation of two fragments taken 90° (or three clock hours) from the limbus and adjacent conjunctiva of the healthy donor eye. In bilateral limbal stem cell deficiency, the most frequently indicated procedure is a heterologous transplant or limbal allograft, which involves the donation of the limbus and conjunctiva from the eye of either a human leukocyte antigen (HLA)-compatible relative [known as a living related conjunctival limbal allograft (LR-CLAL)] or a non-compatible donor, either live [living conjunctival limbal allograft (CLAL)] or cadaveric [cadaveric limbal allograft (c-KLAL)](3,4). Although rare, there is a potential risk of iatrogenic limbal stem cell deficiency for the donor eye if a large amount of tissue is removed(5).
Table 1 Comparison of the SLET, CLET, and CLAU surgical techniques for limb transplant((10))
| SLET | CLET | CLAU | |
|---|---|---|---|
| Surgical time | One | Two | One |
| Interval between surgical time | None | Two weeks | None |
| Size of donor tissue (mm) | 2 | 2 | 10-20 |
| Conjunctival donor tissue | No | No | Yes |
| Stem cell laboratory | No | Yes | No |
| Amniotic membrane | Yes | Yes | No |
| Site of transplantation | Over entire cornea | Over entire cornea | Only over the limbo |
| Possibility of causing limbal stem cell deficiency in the donor eye | No | No | Yes |
| Favorable outcome | Waiting | 50%-100% | 77%-100% |
SLET= simple limbal epithelial transplantation; CLET= cultivated limbal epithelial transplantation; CLAU= conjunctival autograft transplantation.
Another technique for treatment is cultivated limbal epithelial transplantation (CLET), which involves the minimal removal of limbic tissue, measuring approximately 2 mm, from the donor eye to be expanded ex vivo onto a scaffold as an amniotic membrane, which is then transplanted onto the recipient eye. However, the cost of establishing and maintaining a stem cell laboratory is extremely high, restricting the availability of this technique to major research centers.
More recently, a new technique called simple limbal epithelial transplantation (SLET) was proposed for limbal autografts. SLET involves the removal of a 4 mm × 2 mm limbal tissue graft from the donor eye. One of the benefits of SLET is a reduced risk of iatrogenic limbal stem cell deficiency in the donor eye that may occur during CLAU. In addition, SLET can be performed in a single surgical procedure and does not require a laboratory for cell expansion, thereby reducing the costs of surgery.
This case series evaluates the short-term results of limbal transplantation using SLET in patients with unilateral total limbal stem cell deficiency.
METHODS
Four patients diagnosed with unilateral total limbal stem cell deficiency due to ocular burn were selected for inclusion in this case series. The diagnosis was defined on the basis of clinical criteria, including loss of the Vogt palisades, irregularity of the corneal epithelium, superficial corneal vascularization, persistent epithelial defect, and corneal conjunctivalization.
The procedure was performed under peribulbar anesthesia in the recipient eye and topical anesthesia in the donor eye. In the donor eye, a 4 mm × 2 mm section of limbal tissue was marked with a tecidual pen (Codman 38). Excision of the corneal-scleral conjunctiva and limbal tissue was performed. In the recipient eye, 360° peritomy and superficial keratectomy with the removal of the abnormal epithelium and fibrovascular pannus were performed (Figure 1). Then amniotic membrane(8) attached to the underlying corneal stroma was transplanted using a fibrin tissue adhesive (Evicel®, Johnson & Johnson, Somervile, NJ, USA). The limbal graft was divided into 10 to 20 equal pieces, which were placed on the amniotic membrane with the epithelial side up, in a circular fashion, while avoiding the visual axis. At the end of the surgical procedure, a soft contact lens was placed on the recipient eye and was followed by overnight patching.
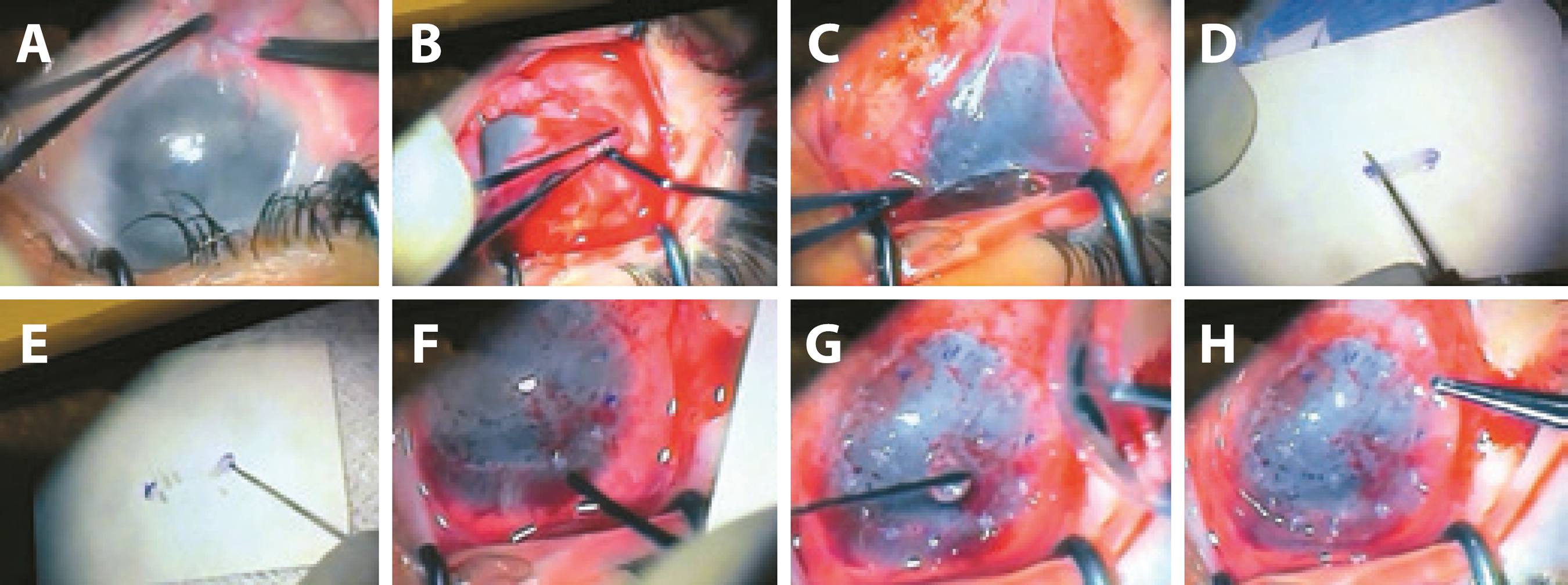
Figure 1 Clinical photographs showing the surgical technique of simple limbal epithelial transplantation (SLET). (A) 360° peritomy was performed. (B) The fibrovascular pannus is excised from the recipient cornea. (C) A human amniotic membrane graft is placed on the bare ocular surface and secured to it with fibrin glue. (D, E) The donor limbal tissue is cut into small pieces. (F, G) The small limbal transplants are transferred to the recipient eye and fixed in place with fibrin glue. (H) A soft bandage contact lens is placed on the recipient eye.
Postoperatively, antibiotics eye drops (moxifloxacin 5 mg/mL eye drops, Vigamox®, Alcon Labs, Brazil) were prescribed for instillation four times a day together with topical steroid (prednisolone acetate 1% eye drops, Pred Fort®, Alcon Labs, Brazil) instillation six times a day. Patients were evaluated on days 1, 7, 15, and 30 and then monthly for until 6-month follow-up.
RESULTS
The demographic and clinical characteristics of patients are described in table 1. At 6-month follow-up, a completely epithelialized and avascular corneal surface was observed in two patients (50%, cases 1 and 2; Figure 2). Visual acuity improved from hand motion (HM) to 20/80 vision (Case 2) in one patient. The other patients did not have any change in the final visual acuity because of the presence of stromal opacity in the visual axis. In one patient, there was no adherence of the amniotic membrane and limbal cornea fragments (Case 3). Another patient (Case 4) had a recurrence of corneal neovascularization and persistent epithelial defect after 6-months follow-up. None of the patients developed any infectious complications resulting from the surgical procedure (Table 2).
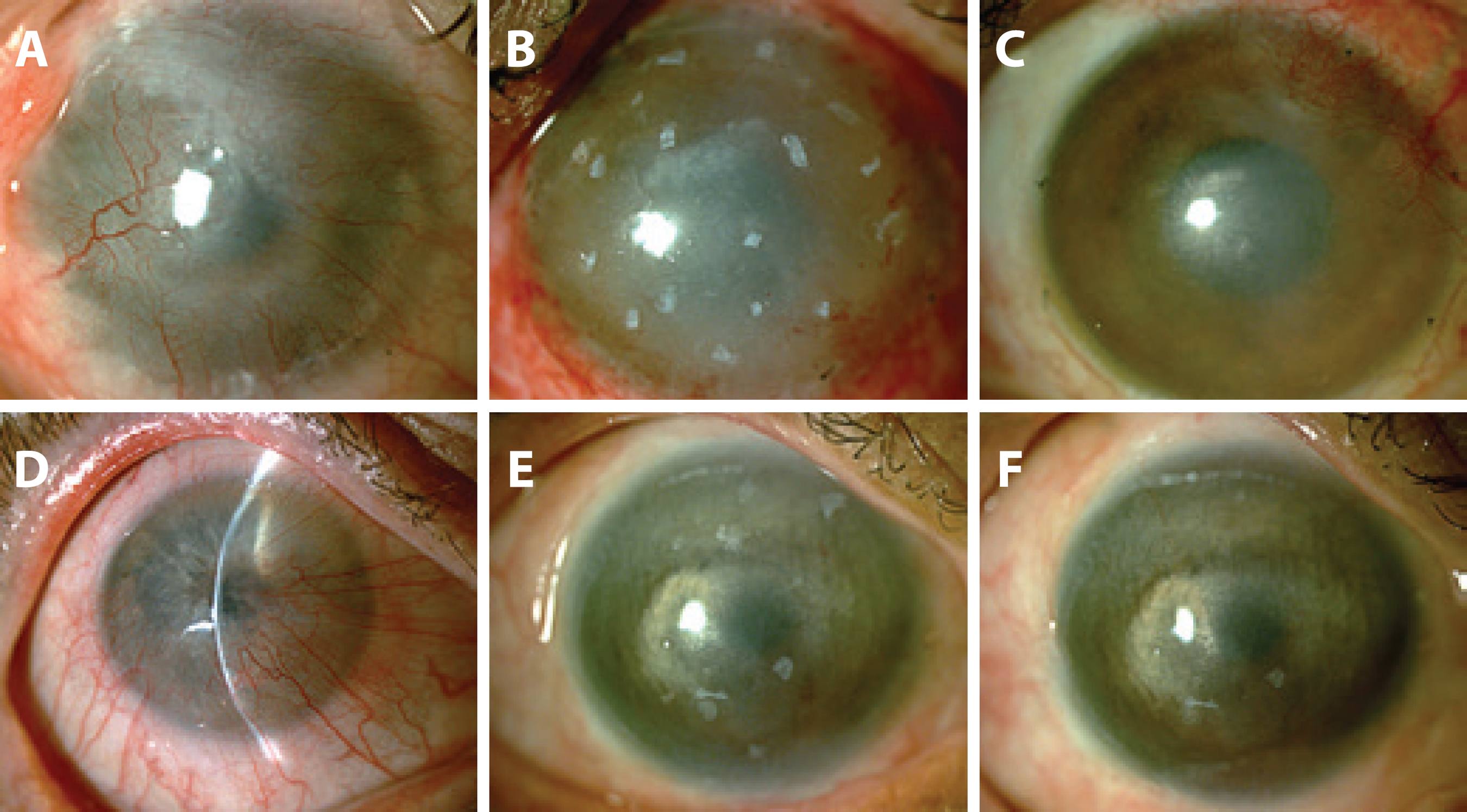
Figure 2 Series of photographs of two patients who successfully underwent SLET. (A) Preoperative appearance of case 1: male, after 6 years of an acid corneal burn in the left eye, with unilateral total limbal stem cell deficiency. (B) Postoperative appearance of case 1 (30-day follow-up): total corneal epithelialization. (C) Postoperative appearance of case 1 (90-day follow-up): total corneal epithelialization, superficial vascularization 12 to 24 hours and some fragments of limbal graft in absorption. (D) Preoperative appearance of case 2: Female patient, after 30 years of an alkali corneal burn, with unilateral total limbal stem cell deficiency. (E) Postoperative appearance of case 2 (60-day follow-up): total corneal epithelialization. (F) Postoperative appearance of case 2 (180-day follow-up): total corneal epithelialization, avascular cornea, and some fragments of limbal graft in absorption.
Table 2 Clinical and demographic characteristics of patients with limbal stem cell deficiency who underwent SLET
| Case | Age (years) |
Sex | Eye | Duration (years) |
Ocular surgery |
Initial VA | Final VA |
|---|---|---|---|---|---|---|---|
| 1 | 38 | M | L | 6 | CLAU | HM | HM |
| 2 | 55 | F | R | 30 | No | CF at 1 m | 20/80 |
| 3 | 74 | M | R | 10 | No | CF at 2 m | CF at 2 m |
| 4 | 14 | M | R | 5 | Eyelid reconstruction | HM | HM |
SLET= simple limbal epithelial transplantation; L= left eye; R= right eye; M= male; F= female; CLAU= conjunctival autograft transplantation; VA= visual acuity; HM= hand movements; CF at 1 m= counting fingers at 1 meter; CF at 2 m= counting fingers at 2 meter.
DISCUSSION
Despite good results with the conventional technique for limbal autograft transplantation (CLAU), the SLET technique may be increasingly used when considering the associated reduction in the risk of iatrogenic limbal stem cell deficiency in the donor eye. Techniques involving cell therapy represent a major advance in the treatment of ocular surface diseases. Studies have suggested that transplantation of limbal stem cells that are expanded ex vivo (CLET) is safer for the donor eye because it requires lesser tissue and has better long-term results because of the higher number of cultivated limbal cells that are transplanted(9,10). However, the costs of installing and maintaining a stem cell laboratory restrict the use of the procedure to major research centers.
The SLET technique described in this case series presents the advantages of CLAU, including a single surgical procedure and the nonrequirement for a stem cell laboratory, in addition to the same advantages as CLET, related to the use of lower amounts of donor tissue (Table 1 compares CLAU, CLET, and SLET techniques).
In this case series, we observed good results in two out of four (50%) of patients. However, no substantial improvement in visual acuity was observed because of the underlying corneal opacity. Therefore, the next step for visual rehabilitation in these patients is corneal transplantation.
Case 1 had a history of failed limbal transplantation (CLAU). It could possibly be considered that this surgery interfered with the outcome; however, the fact that CLAU failed and conjunctivalizations recurred and that SLET was associated with previous 360° peritomy and keratectomy make such a possibility unlikely.
Among the two cases in which we were unsuccessful, one case presented an early complication, including limbo-conjunctival fragments and amniotic membrane detachment, and the second case showed graft failure and recurrence of corneal neovascularization. The failure in the first case can be explained by a problem with the biological adhesive used or traumatic displacement of the graft. In the second case, there may have been damage or failure of the transplanted limbal epithelial stem cells. In addition, it is possible that, as with any surgical procedure, the learning curve has influenced our results.
Considering the first results of SLET published by Sangwan et al.(7) and the satisfactory initial results we obtained in two of our four cases, it seems that the SLET technique may be a good alternative in treating total limbal stem cell deficiency. In conclusion, these results suggest the need for larger studies to observe the long-term outcomes and to confirm the effectiveness of the SLET technique.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

