INTRODUCTION
Temperature is an important health indicator and can be assessed using the wavelength of the infrared rays between 700 nm and 100,000 nm that are released by the human body as heat(1). The human body reflects its surface temperature because it is an excellent infrared energy emitter(2).
Thermography is a diagnostic imaging method that can capture and record the heat emitted from the body surface, allowing both non-invasive and safe investigation(3,4). The thermography diagnostic method is based on the detection of infrared images that are emitted from the patient's body surface in real time. A thermographic camera captures the infrared radiation emission patterns, which are invisible to the naked eye and imperceptible to touch, and translates them into information encrypted in colors that can help to detect changes in normal patients(4).
In this report, we have demonstrated the recurrent acute inflammatory process in a case of lower tear obstruction and the use of thermal imaging.
CASE REPORT
A 56-year-old woman (MAS) visited the Ophthalmology Emergency Room with a complaint of epiphora and swelling in the lacrimal sac region of the right eye. She had experienced the same symptoms on two previous occasions at an interval of 3 years and had been treated with systemic antibiotics. The patient had undergone radioiodine therapy for 6 months at the same institution due to thyroid carcinoma associated with a thyroid nodular goiter and follicular adenoma. It was first believed to be an acute case of dacryocystitis. After the prescription of 500 mg of cephalexine, 4 times a day for 7 days, she was referred to the Lacrimal System Service at the Department of Ophthalmology.
Ectoscopic evaluation revealed a substantial tumefaction of the lacrimal sac area and an apparent occlusion of both the upper and lower tear puncta in the right eye, which was probably related to the radioiodine therapy. Dacryocystography is typically the standard procedure for diagnosing this type of obstruction, but was contraindicated in this case. In order to evaluate the nasolacrimal duct, infrared thermography was used as a complementary propaedeutic.
The examination was performed with a thermal camera T650 sc model (FLIR Systems Inc., Portland, USA), which promoted high definition images (620 × 420 pixels) with high sensitivity and allowed the detection of differences at 0.03°C in tissue temperature (Figure 1). The patient was positioned in front of the camera, which was placed on a support 80 cm away from the lacrimal sac area.

Figure 1 Thermographic camera, T650 sc model (FLIR Systems Inc., Portland, USA) that is used for diagnostic thermography examinations with 620 × 420 pixel definition, and that is capable of detecting differences in temperature with 0.03°C sensitivity.
The room temperature was maintained at 23°C throughout the evaluation and the images were captured 15 min after the temperature of the patient's face matched the temperature of the environment (thermalization). One drop of saline solution (sodium chloride 0.9%) cooled to 18°C had been previously applied to both eyes; a sequence of thermographic images was then shot with the eyes open 3 s after a blink. Care was taken not to allow excessive saline solution to run onto her face, thus preventing any thermal artifact from interfering with the local thermographic images. The camera allowed image magnification of up to eight times and fusion of the thermal and visual images in 3D mode, with optimal heat contrast that corresponded with the photographic image.
The thermographic image captured hypo-radiation in the area corresponding to the dilatation of the right lacrimal sac and appeared as a blue coloration (Figures 2 A and 2 B). The hypo-radiation observed in the thermography image could be associated with the degree of edema caused by tissue inflammation. The same bluish image was not captured in the area corresponding to the left lacrimal sac. After a dynamic examination that included the instillation of cooled drops in the eyes, the left normal eye presented with lacrimal sac cooling with bluish coloration. No local cooling was observed in the right lacrimal sac.
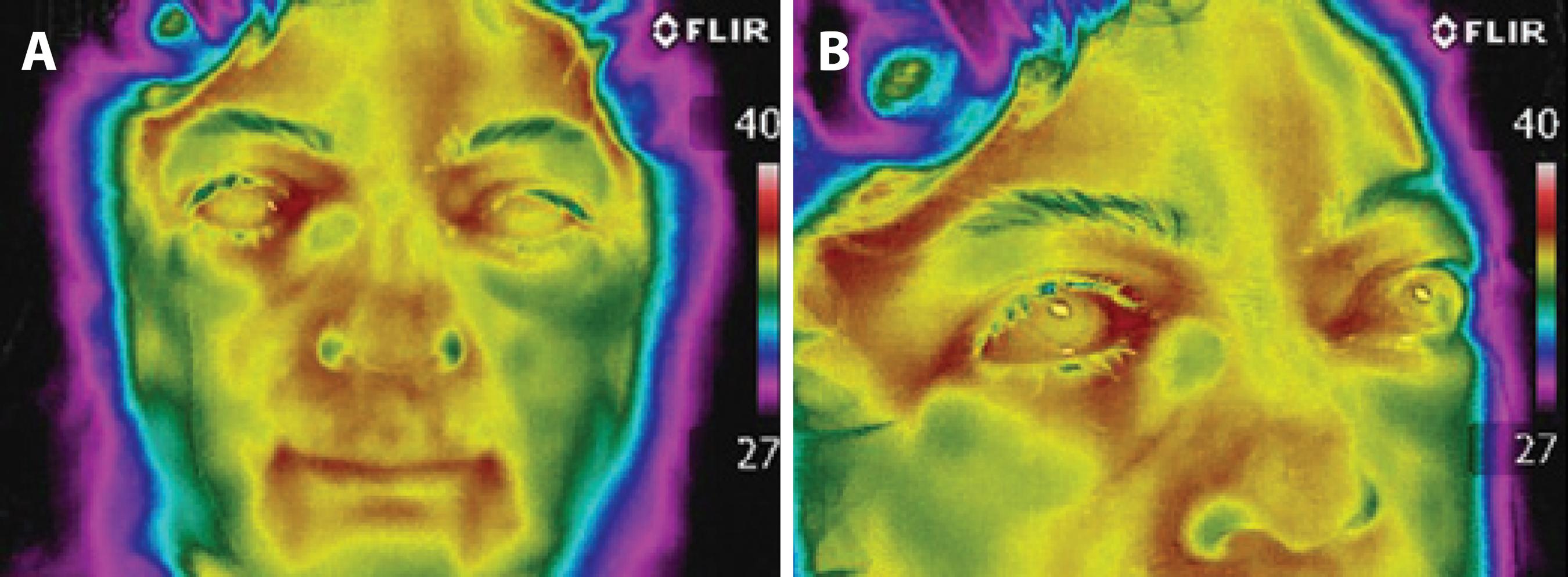
Figure 2 A) Thermographic image of the patient’s face, showing inflammation around the lacrimal sac of the right eye that reached the lower eyelid that was observed as a bluish warm halo (hyper-radiation); this corresponded to hyper-radiation or local heating, which was not observed in the lacrimal sac of the left eye. B) Magnified image of 2A, showing blue coloration where the dilatation of the lacrimal sac indicated local edema from chronic inflammation (hypo-radiation).
Diagnosed with chronic dacryocystitis, the patient was referred for surgical intervention with an external right dacryocystorhinostomy, which included the surgical opening of the upper and lower ipsilateral lacrimal puncta.
DISCUSSION
First described by Raflo et al. in 1982, the use of thermal imaging for the lacrimal system is an investigative method without known side effects(5). Unlike the dacryocystography exam, there is no need to touch the patient or to use a contrast substance. This allows for safer and faster assessment of the drainage system, with a higher degree of patient cooperation.
Blood flow is the major mechanism of heat transfer in the human body(5) and thermography can use images to document the effects on the microcirculation and vasomotor activity involved in the inflammatory process as well as in superficial tumors(6).
Thermal imaging of the lacrimal drainage allows confirmation and assessment of the degree of tissue inflammation. The thermographic images are compared to determine the bilateral asymmetry of the thermal capture and the hyper-radiation or heat. In cases of acute dacryocystitis crises, the finding of the thermal imaging will be a hyper-radiation of the lacrimal sac(7). Even when relying on an apparatus that had lower definition than that described in this case, Rosenstock et al.found a sensitivity of 42% and a specificity of 60%(8) for the detection of inflammatory processes in the lacrimal drainage system. In the case presented, the static thermal image highlighted a chronic inflammation of the lacrimal sac that already contained edema; this appeared bluish (cold) in the thermographic examination.
In this case, the dynamic examination using the cold drop was crucial. The lacrimal sac has an average diameter of 1.5 cm and is located in the tear sac at a distance of approximately 0.5 cm from the skin; these factors allow medical thermography to provide a reliable thermal evaluation(9). Cooling of the medial corner of the orbits is the expected normal response to the instillation test of cooled drops(4). When no local cooling is observed, it is identified as a pathologic finding, and may suggest the existence of an obstruction.
The clinical presentation of a lacrimal obstruction in the reported case may have been due to radioiodine therapy for thyroid carcinoma. This association has been described in the literature(10), or combined with other conditions that jointly acted to produce lacrimal obstruction.
In the present case, we chose to use the thermography method due to the presence of a tumefaction in the lacrimal sac area that could preclude cannulation in dacryocystography. This method also had the advantage of avoiding additional radiation exposure, lowering cost, and improving ease of use compared to radiologic methods such as computed tomography (CT) and magnetic resonance imaging (MRI). In the event there was any suspicion of a possible invasion of the lacrimal system by a neoplastic process, CT or MRI scans would be mandatory.
Thermography is a non-contact diagnostic technique that does not require the use of radiation and that provides objective evidence about the permeability of the lacrimal drainage system. This information is particularly useful when there is clinical suspicion of inflammation.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

