INTRODUCTION
Keratoconus is a common, non-inflammatory, progressive corneal disorder with a typical onset in early adulthood(1). Keratoconus that is characterized by thinning and protrusion of the central cornea frequently leads to a mild-to-severe decrease in best-corrected visual acuity (BCVA). Loss of visual acuity can be improved with contact lenses or spectacles in the early stages of the disease; however, patients may eventually require corneal grafting as their condition progresses. Keratoconus is the single most common reason for keratoplasty in the developed world(1-3).
Penetrating keratoplasty is associated with a high success rate and continues to play an important role in keratoconus management. However, it is also associated with significant complications, including immunological rejection, secondary cataract, glaucoma, and microbial keratitis(4,5). Moreover, visual rehabilitation or recovery of visual acuity following transplantation may be slow and unsatisfactory. There is a growing interest in treatment options that may delay or defer corneal grafting, including the use of intrastromal corneal ring segments (ICRS)(6).
Originally used to correct mild-to-moderate myopia, ICRS exert an ''arc-shortening" effect on the corneal lamellae, thus reducing steepening of the central cornea(3). This decreases refractive errors and improves corneal surface regularity. Moreover, there is evidence to suggest that implanting an ICRS may delay the requirement for penetrating keratoplasty(7-9).
There are several commercially available ICRS that vary with regard to curvature, width, and zone of implantation(3). One such ICRS is the Keraring (Mediphacos, Belo Horizonte, Brazil), a small, arc-like segment made of polymethyl methacrylate. It is characterized by a unique prismatic design that flattens the cornea and reduces the incidence of glare and halos. Several clinical studies have demonstrated their efficacy in improving visual function, reducing the magnitude of corneal astigmatism, and flattening the central corneal surface(10-14). Although previous studies have evaluated ICRS efficacy in patients who were intolerant to rigid contact lenses (and therefore potential candidates for a corneal transplant)(15-17), to the best of our knowledge, there are no published data regarding Keraring ICRS efficacy in patients with keratoconus who were already scheduled for penetrating keratoplasty. Consequently, we performed a small case series study to determine whether Keraring ICRS implantation might represent a surgical alternative to corneal grafting in patients with keratoconus who were awaiting penetrating keratoplasty.
METHODS
We conducted a retrospective observational case series study on the basis of an analysis of records of patients included in the State of Goiás corneal graft waiting list. These patients underwent Keraring ICRS implantation as a potential alternative to keratoplasty. All procedures were performed by the same surgeon at the Centro de Referência em Oftalmologia UFG, Goiânia, Brazil between June and December 2008. Written informed consent was obtained prior to study and data collection.
The study included 18 patients (19 eyes) with a mean age of 23.36 ± 6.22 years and with keratoconus varying from Grade II to IV (Amsler-Krumeich scale). Patients were included if they had evidence of topographical alteration that was compatible with keratoconus, a minimal corneal thickness of 380 µm, low BCVA with spectacles, and intolerance to contact lenses. Exclusion criteria included topographic curves over 70 D, apical opacity, and external ocular infection. Baseline characteristics of the patients are summarized in table 1.
Table 1 Patient characteristics
| N (%) | |
|---|---|
| No patients | 18 |
| Gender | |
| Female | 12* |
| Male | 6 |
| Nº of eyes | 19 |
| Right eyes | 9 |
| Left eyes | 10 |
| Age (years) | |
| Mean | 23.36 e 6.22 |
| Range | 14-32 |
*= one female was subject to bilateral implantation with ICRS.
Prior to ICRS implantation, all patients underwent a detailed preoperative clinical assessment, including the measurement of BCVA (logMAR), applanation tonometry, biomicroscopy, fundoscopy, pachymetry, and corneal topography. Patients were postoperatively evaluated for BCVA.
ICRS selection was based on the Mediphacos nomogram for the Keraring®calculation system (Belo Horizonte, Brazil). All surgeries were performed on an outpatient basis under topical anesthesia (5 mg/mL proxymetacaine HCl and 5% povidone iodine). The ICRS tunnel was manually created. The center of the visual axis on the cornea was marked, and an initial perpendicular corneal incision was made at the 5-7-mm zone with an adequate depth for each case. This was followed by radio intrastromal channelization. Appropriate ICRS was finally placed inside the corneal tunnels.
Following the procedure, patients were administered Maxitrol® eye drops (Alcon Laboratories, Brazil) every 2 h for 2 weeks, followed by Florate®(Alcon Laboratories, Brazil) four times daily, also for 2 weeks.
Postoperative outcomes were evaluated at postoperative days 1, 7, 30, 90, 180, and eventually 2 years following implantation. BCVA was measured and biomicroscopy and applanation tonometry were performed at each follow-up visit, whereas fundoscopy was performed at the 6-month follow-up visit. The effectiveness of ICRS in terms of preventing corneal grafting was evaluated at the 2-year follow-up visit.
RESULTS
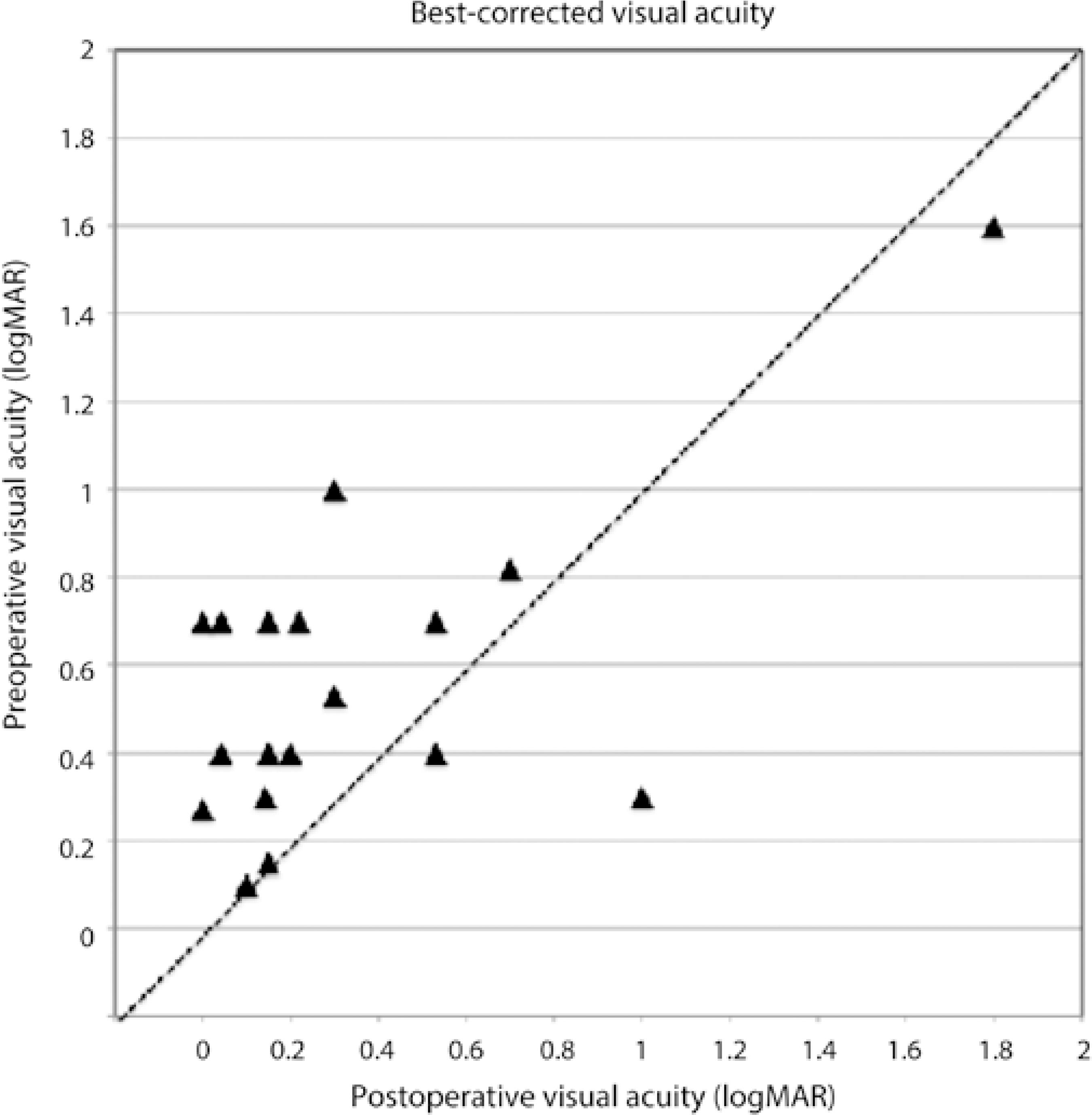
Pre- and postoperative BCVA (logMAR) data of each patient are displayed in table 2. Mean preoperative BCVA was 0.59 ± 0.35. At the 2-year cut-off point following ICRS implantation (mean follow-up, 28.72 ± 4.71 months), mean BCVA was 0.35 ± 0.45 (Figure 1). This improvement in BCVA was statistically significant (p<0.01). One patient developed infectious keratitis on postoperative day 1. Consequently, this patient had his corneal rings removed, and his data excluded from the statistical analysis of BCVA. The patient subsequently underwent corneal grafting.
Table 2 BCVA (logMAR) pre- and post-ICRS implantation
| Eye | Preoperative BCVA | Postoperative BCVA* |
|---|---|---|
| 1 | 0.15 | 0.15 |
| 2 | 0.53 | 0.30 |
| 3 | 0.30 | 1.00 |
| 4 | 1.00 | 0.30 |
| 5 | 0.70 | 0.22 |
| 6 | 0.70 | 0.53 |
| 7 | 0.30 | 0.14 |
| 8 | 0.70 | 0 |
| 9 | 1.60 | 1.80 |
| 10 | 0.40 | 0.15 |
| 11 | 0.27 | 0 |
| 12 | 0.40 | 0.53 |
| 13 | 0.82 | 0.70 |
| 14 | 0.10 | 0.10 |
| 15 | 0.70 | 0.15 |
| 16 | 0.70 | 0.04 |
| 17 | 0.40 | 0.04 |
| 18 | 0.40 | 0.20 |
*= two-year cut-off point (mean follow-up, 28.72 ± 4.71 months); NB= one of 19 eyes included in the study was excluded from BCVA statistics.
At the 2-year cut-off point, 3/19 eyes (15.8%) were still considered candidates for penetrating keratoplasty because they did not achieve significant corneal applanation or regularity. However, the remaining patients (84.2%) maintained BCVA with spectacles (52.6% patients) or contact lenses (31.6% patients). Apart from one case of infectious keratitis, no other relevant complications occurred.
DISCUSSION
Although initially approved by the US Food and Drug Administration as a treatment for myopia, ICRS has become a mainstay in managing keratoconus. Since Colin et al. first reported regarding the use of ICRS in keratoconus more than a decade ago(7), a plethora of studies have demonstrated their ability to effectively reduce refractive errors and safely improve corneal surface regularity. While there is also increasing evidence to suggest that ICRS may delay the requirement for penetrating keratoplasty(5,18), published evidence describing ICRS effects in patients with keratoconus already scheduled to undergo penetrating keratoplasty is limited.
The results of our case series of 18 patients (19 eyes) who awaited corneal grafting suggest that ICRS may be an efficacious alternative to penetrating keratoplasty. At the 2-year data cut-off point, we noted that 84% eyes maintained BCVA with spectacles (52.6%) or contact lenses (31.6%), whereas 3/19 eyes (15.8%) still required keratoplasty because they did not achieve significant corneal applanation or regularity.
Data from a previously published, one-year, 50-eye study demonstrated that Keraring ICRS implantation improved both uncorrected visual acuity and BCVA in patients with keratoconus (17). Similarly, in a 35-eye study, Coimbra et al. demonstrated that Keraring ICRS improved visual acuity and topographic data in patients with secondary corneal ectasia at a 3-month postoperative follow-up(11). However, to the best of our knowledge, no reports on the use of Keraring ICRS as a treatment for patients who have already been triaged for corneal transplantation are available. Consequently, it is somewhat difficult to discuss our findings within the context of others. However, there is a comparative case study of 76 eyes with advanced keratoconus. These patients received either ICRS implantation or deep anterior lamellar keratoplasty. ICRS effected a statistically significant increase in visual acuity (corrected and uncorrected distance visual acuity) from baseline to postoperative 24 months (p<0.001)(19). Similarly, data from a study by El-Husseiny et al., which included 20 eyes of 16 patients, revealed that ICRS (Intacs, Addition Technology, Inc, Sunnyvale, CA) provided a viable alternative to early penetrating keratoplasty for patients with keratoconus having a clear central cornea and a history of contact lens intolerance. Specifically, the data revealed that after 6 months of follow-up, the mean uncorrected distance visual acuity improved from 0.07 ± 0.07 preoperatively to 0.6 ± 0.26 postoperatively, whereas mean BCVA changed from 0.4 ± 0.15 preoperatively to 0.9 ± 0.29 postoperatively(20).
Although data from our small study suggests that ICRS may be a surgical alternative to keratoplasty in some patients with keratoconus, longer-term follow-up is required to determine for how long ICRS adequately maintain BCVA and whether patients for whom ICRS implantation was effective will eventually require penetrating keratoplasty.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

