INTRODUCTION
Zika virus (ZIKV) is a neurotropic flavivirus related to the Dengue, Yellow Fever and West Nile viruses(1). Even though it was first identified in the world in 1947(1), the first autochthone transmission in Brazil was confirmed only in April 2015(2). Since then, it is estimated that more than one million Brazilians had ZIKV infection, reflecting the virus' capacity to cause large-scale outbreaks where the biological vector Aedes aegypti is endemic(2,3).
Six months following the beginning of the ZIKV outbreak, there was an unusual increase in newborns with microcephaly in Brazil. In 2015, 1,248 new suspect cases were registered, representing a twenty-fold increase when compared to recent years(3).
Maternal-fetal transmission of ZIKV has been previously demonstrated(4). In Brazil, ZIKV has been detected in the amniotic fluid of two pregnant women of babies with microcephaly and in the tissue of a newborn with microcephaly that died after birth(3). Thus, the Brazilian Ministry of Health has associated this malformation with ZIKV intra-uterus infection(3).
Our group recently published the first report on retinal findings of three infants with microcephaly and presumed ZIKV vertical infection.(5) Here we assessed more patients through a complete ophthalmological exam and report our findings.
METHODS
We report the findings of 10 infants with microcephaly, as defined by an occipitofrontal circumference more than two standard deviations below the mean for age and sex(3), with clinical diagnosis of ZIKV vertical infection, and previously diagnosed with ophthalmological abnormalities referred to the Altino Ventura Foundation, in Recife, Brazil, for ophthalmologic examination on December 14, 2015.
RESULTS
Six (60.0%) were female. Their mean age at the day of the exam was 1.9 ± 0.9 months (range: 0.7 to 2.9 months). Computerized tomography scans evidenced cerebral calcifications in all patients. They were born during the ZIKV infection outbreak, and seven (70.0%) of the mothers had dengue-like symptoms (malaise, rash and arthralgia) during pregnancy, of which six (85.7%) were in the first trimester. The mean age of mothers' at labor was 29.1 ± 7.3 years (range: 19 to 42 years). Since the infants had negative serology for Toxoplasmosis, Rubella, Cytomegalovirus and Human Immunodeficiency Virus (HIV), they were clinically diagnosed with presumable intra-uterus ZIKV infection. At birth, their mean gestational age was 38.3 ± 0.5 weeks (range: 37.6 to 39 weeks), their mean cephalic perimeter was 28.8 ± 1.5 cm (range: 26 to 31.5 cm), and their mean weight was 2,901 ± 461.6 g (range: 2,105 to 3,800 g).
The mothers' ocular examinations were normal. The infants had normal anterior segment structures; a mean axial length measured with immersion ultrasound of 18.4 ± 0.6 mm (range: 17.6 to 19.3 mm) in the right eye (OD) and 18.3 ± 0.4 mm (range: 17.6 to 19.1 mm) in the left eye (OS).
Horizontal nystagmus was observed in one infant (10.0%). Pupils were normally reactive, with no afferent pupillary defect, and Hirschberg testing revealed exophoria in four patients (40.0%) and esophoria in two (20.0%). Cycloplegic refraction showed a mean spherical equivalent of -0.40 ± 2.40 diopters (D) (range: -3.50 to +2.00) in OD and 0 ± 2.50 D (range: -3.00 to 3.50 D) in OS. The preferential looking behavior of all infants was present.
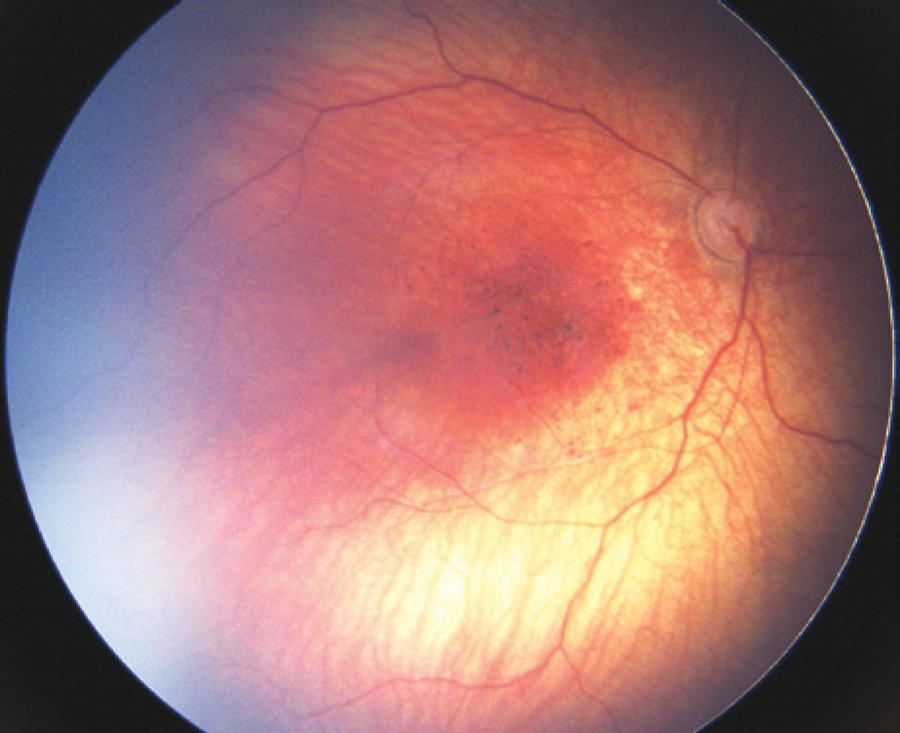
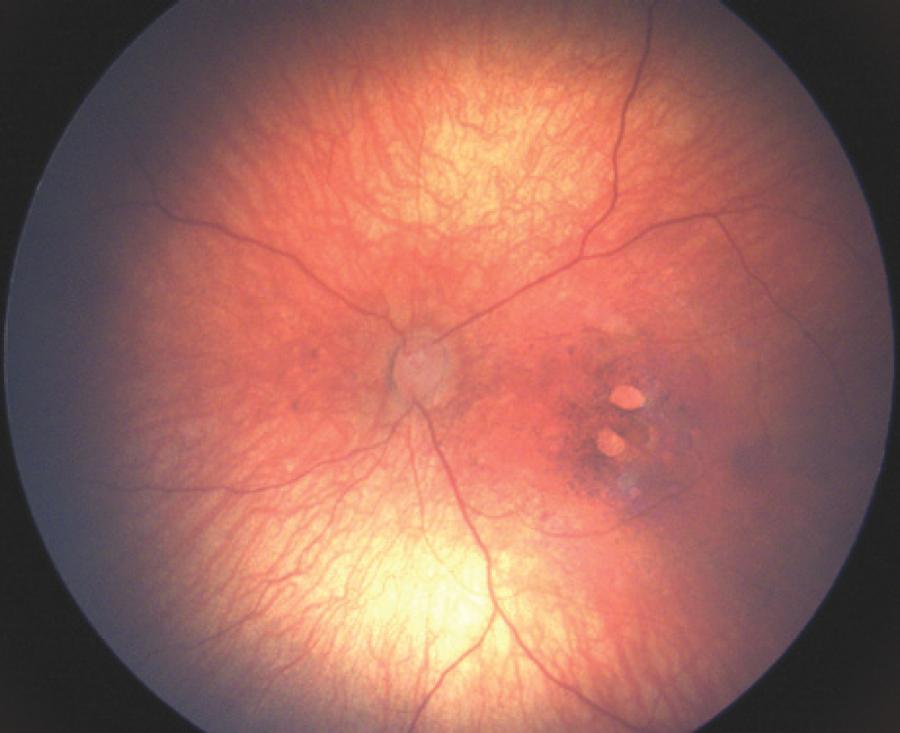
Retinal evaluation revealed, optic nerve and macular alterations were 17 eyes (85%) (Table 1). Optic nerve findings consisted of hypoplasia with the double-ring sign, pallor, and increased cup-to-disk ratio. The macular abnormalities were foveal reflex loss, mild to gross pigment mottling and sharply demarcated circular areas of chorioretinal atrophy (Figure 1-3). In all eyes, the retina and choroid were attached, and the retinal vessels had normal distribution and appearance.
Table 1 Funduscopic findings in ten infants with microcephaly and presumable intra-uterus Zika virus infection
| Infant | 1 | 1 | 2 | 2 | 3 | 3 | 4 | 4 | 5 | 5 | 6 | 6 | 7 | 7 | 8 | 8 | 9 | 9 | 10 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eye | D | S | D | S | D | S | D | S | D | S | D | S | D | S | D | S | D | S | D | S |
| Optic nerve head hypoplasia | X | X | X | X | X | |||||||||||||||
| Optic nerve double-ring sign | X | X | ||||||||||||||||||
| Optic nerve head pallor | X | X | X | |||||||||||||||||
| Cup-to-disk ratio >0.5 | X | X | ||||||||||||||||||
| Cup-to-disk ratio >0.7 | X | X | ||||||||||||||||||
| Foveal reflex loss | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||
| Mild macular pigment mottling | X | X | X | X | X | |||||||||||||||
| Gross macular pigment mottling | X | X | X | X | X | X | X | X | ||||||||||||
| Chorioretinal macular atrophy* | X | X | X | |||||||||||||||||
| No ophthalmic abnormalities | X | X | X |
*= sharply demarcated circular area of chorioretinal atrophy on the macula.
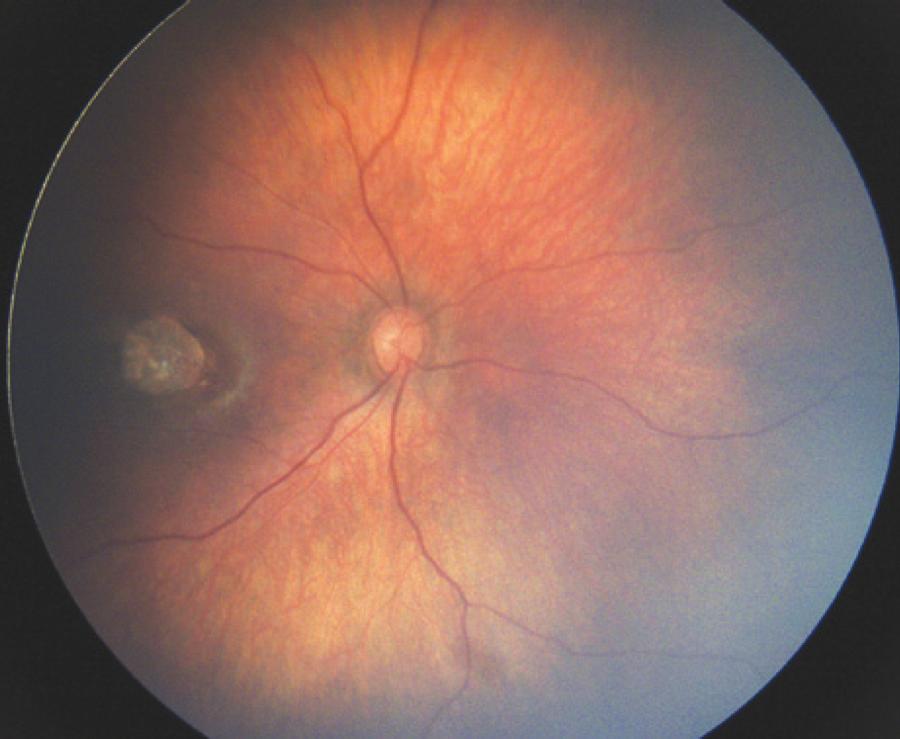
Figure 1 Wide-angle fundus image (Retcam®) of the right eye of infant number 8 showing an optic disc hypoplasia with double-ring sign associated with one sharply demarcated chorioretinal atrophy on the macula.
DISCUSSION
The 2015 Brazilian ZIKV infection outbreak was the first to have an association between this virus and the severe complication of newborns with microcephaly(2,3). In January 2016, we published the first report of funduscopic lesions related to this condition(5). In the present paper, we report the ophthalmologic assessment of 10 infants with abnormal ophthalmic exam, born with ZIKV-related microcephaly.
Seven mothers had dengue-like symptoms in the first or second trimester of pregnancy, and Toxoplasmosis, Rubella, Cytomegalovirus and HIV were ruled out by serology. Since approximately 80% of patients with ZIKV infection are asymptomatic, the lack of symptoms does not rule out the infection(3). Additionally, the only available method to diagnose ZIKV infection is real time polymerase chain reaction (PCR), which is useful to detect the virus in the acute phase of illness (first 5 days of acute infection). Since the dengue-like symptoms were present months before labor, this test is not helpful in confirming the infection in our infants(3). Thus, the diagnosis of Zika-related microcephaly was considered when the clinical criteria of the Brazilian Ministry of Health was fulfilled(3).
All patients had normal anterior segment structures and axial length(6). Four patients (40.0%) presented myopia, differently than the hyperopia usually seen in infants(6).
The West Nile Virus, another flavivirus, can cause chorioretinal scars and granularity when maternal-fetal transmission occurs(7). In our previous report of three cases of intra-uterus ZIKV infection, gross macular pigment mottling and macular chorioretinal atrophy were detected(5). Similarly, in the present report, fifteen eyes (75.0%) had these macular abnormalities, which had not been reported in other ZIKV outbreaks worldwide(5). In addition, optic nerve alterations were observed for the first time. Nine eyes (45.0%) had optic nerve hypoplasia, pallor and increased cup-to-disk ratio. Optic nerve hypoplasia has been previously associated with cytomegalovirus intra-uterus infection(8). However, in the present series, these other causes of the chorioretinal and optic nerve abnormalities were ruled out(9).
The physiopathology of the lesions presented by these infants may be related to the virus or toxin leading to an inflammatory reaction. This could result in severe cerebral findings (abnormal development and cerebral calcification), as well as ocular lesions. We hypothesize that ZIKV may cause more severe ocular abnormalities when the infection occurs in the first or second trimester of pregnancy, following the reasoning of other vertical infections, such as Toxoplasmosis, Rubella and Cytomegalovirus(9). Furthermore, other unknown factors such as the amount of viral circulation and the immunologic response of mother and fetus, may play an important role on the abnormalities observed in the newborns.
In conclusion, we reported the ophthalmologic findings of 10 infants with ZIKV-related microcephaly born during the ZIKV infection outbreak in Brazil with abnormal ocular exams. The patients had normal anterior segment structures, and important macular and optic nerve abnormalities. Further studies will assess the visual significance of these alterations, which will be important to understand the natural history of this new and devastating manifestation of the ZIKV disease.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

