INTRODUCTION
Persistent hyperplastic primary vitreous (PHPV) is a vitreoretinal malformation characterized by defects in the primary vitreous regression(1). It is a non-heritable disease(2). Most cases are unilateral and sporadic, with no differences of incidence between males and females. It is the second most common cause of acquired cataract during the first year of life(3).
The hyaloid artery becomes impermeable to blood flow during the seventh month of pregnancy, until its complete regression during the following month(4). Bergmeister's papilla arises from the primitive epithelial papillary cells. This papilla forms a glial sheath around the proximal one third of the hyaloid artery, which begins to atrophy during the seventh month of pregnancy. Failure of complete regression results in Bergmeister's papilla(4).
PHPV is classified as anterior and posterior types, or a combination of both. Anterior PHPV is characterized by the presence of a retrolental membrane or mass (Mittendorf dot) and corresponds to 25% of cases. This type is caused by residual fetal anterior vascular system, located in the site of anastomosis of the hyaloid artery and tunica vasculosa lentis in a microphthalmic eye. Patients with anterior PHPV also present with early leukocoria due to the presence of retrolental membrane and cataract induced by this tissue(4). Posterior PHPV contributes to 12% of cases and occurs due to incomplete regression of hyperplastic primary vitreous. It is characterized by the presence of a dense opaque membrane, which extends from the optic disc to the peripheral retina or retrolental region. Crystalline lens is typically transparent, but becomes opaque progressively. The combination of anterior and posterior PHPV contributes to 63% of cases(4).
CASE REPORT
An eight-month-old nursing female infant was referred for ultrasonography due to congenital leukocoria in the left eye. The child was born by full-term eutocic delivery and presented normal postnatal development.
Upon eye examination, unilateral leukocoria and mild vertical deviation were observed. Left eye indirect ophthalmoscopy revealed a white mass on the optic disc involving the posterior pole and a membrane that extended from this mass to the vitreous cavity (Figure 1). The contralateral eye presented no abnormalities.
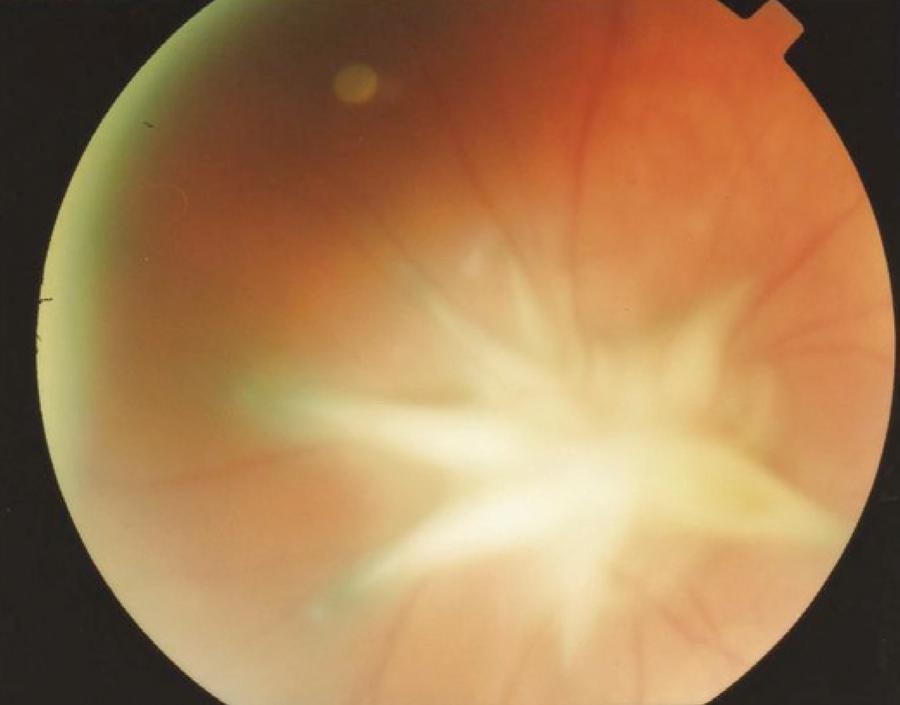
Figure 1 Left eye retinography showing a white mass on the optic nerve, which extends to the posterior pole and has a membrane adhered to it.
Ultrasonography (US) examination performed in Quantel CineScan> equipment using a 10 MHz probe showed a solid elevated lesion on the optic disc. The lesion presented medium-high internal reflectivity and extended from the optic disk to the posterior pole, with internal acoustic shadowing from the papillary area up to the lesion apex, suggesting the presence of a vessel. Also, a medium-high reflective membrane was observed. This membrane was adherent to the lesion surface, extending into the vitreous cavity and limited into its posterior third, in all meridians. The adjacent vitreous was anechoic and there was no retinal detachment. The axial length was asymmetrical: right eye (RE) 21.5 mm and left eye (LE) 19.5 mm (Figure 2).
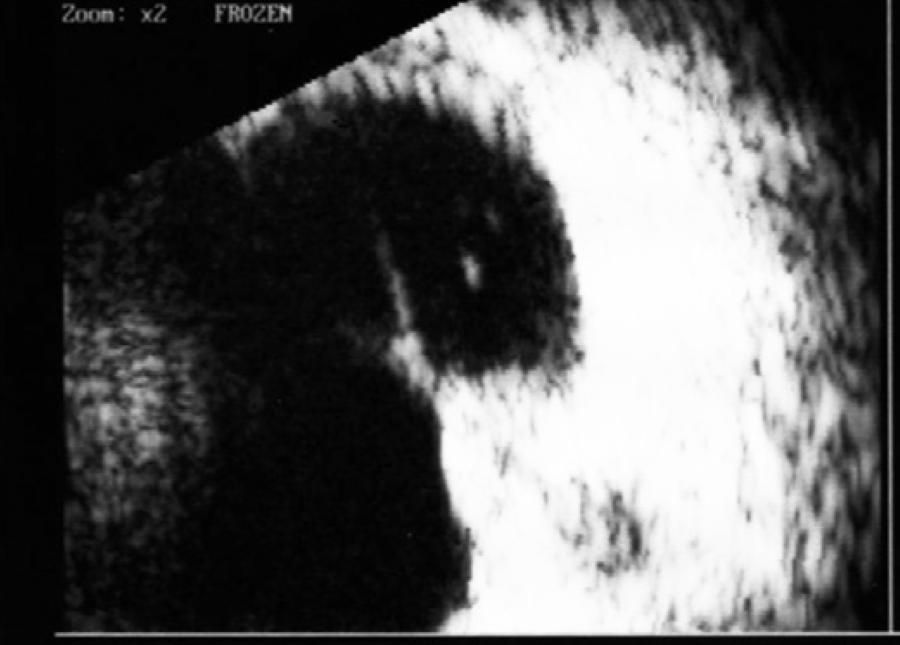
Figure 2 Left eye ultrasonography (10 MHz), showing a solid elevated medium-high reflective lesion, which extends from the optic nerve to the posterior pole. This lesion presents inner acoustic shadowing. Also, a membrane echo adhered to the lesion and extending to the vitreous posterior third is observed.
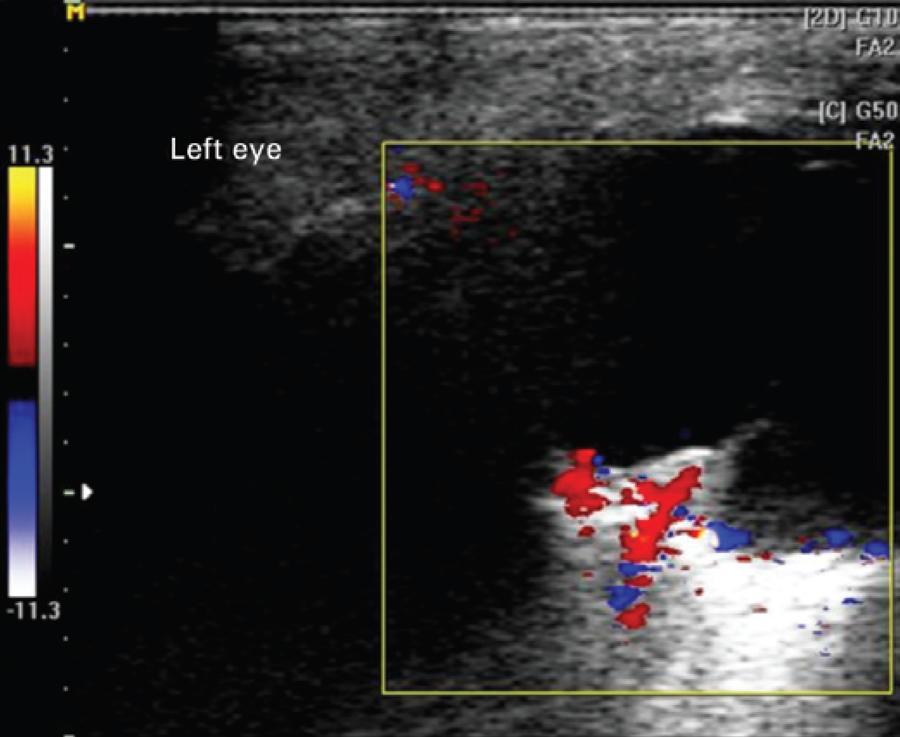
Color Doppler was performed in the Esaote My Lab 25 Gold equipment, with small parts linear probe. Results showed internal flow in the topography of the acoustic shadowing observed by conventional US, which extended to the membrane adhered to the lesion surface. These findings allowed us to reach a conclusion of PHPV diagnosis (Figure 3).
DISCUSSION
In this case, the infant presented leukocoria and small vertical deviation. Fundoscopic exam showed a white mass on the optical disc, which extended to the posterior pole. These findings suggested the following diagnostic hypotheses: PHPV associated with Bergmeister's papilla, granuloma (toxocariasis), astrocytic hamartoma, and retinoblastoma.
Clinical criteria can be associated with additional tests in order to differentiate the causes of leukocoria. These criteria include: age, sex, involvement of one or both eyes, heredity, vitreous involvement, presence or absence of calcification, and eyeball size(5).
Based on these criteria, the leading causes of leukocoria were discarded. Since the child was born after a full-term pregnancy, we discarded retinopathy of prematurity. The absence of telangiectasia, white-yellow exudates, and exudative retinal detachment excluded Coats' disease hypothesis. Thereby, we considered the main previously mentioned hypotheses(3).
The inconclusive cases, in which the clinical examination does not disclose the diagnosis, require the use of complementary exams, such as ultrasonography with or without associated color Doppler, computed tomography, and nuclear magnetic resonance imaging(1).
Although indirect ophthalmoscopy allowed the observation of a white solid mass with glial appearance involving the whole papilla and extending to the posterior pole, these findings were not sufficient for diagnostic disclosure. Thereby, we chose to perform further imaging exams.
Initially, we performed conventional ultrasonography (US), because it presents good sensitivity and specificity for diagnosis and localization, extent and characterization of intraocular and tumor lesions. Doppler ultrasonography (USD) allows the evaluation of vessel flow and can be used in the assessment of vascular lesions, intraocular tumors and orbital lesions, besides cases of membrane differentiation such as retinal detachment and posterior vitreous detachment with impregnated hyaloid(3,6-8).
Toxocariasis cases, upon US examination, present condensate hyperechoic shadows with medium-high reflective membrane extending from the lesion to the periphery. Calcifications, however, are uncommon(3), and upon Doppler examination, there would be neither flow to the lesion (granuloma) nor to the membrane. Small retinoblastoma may not present calcification. The presence of internally calcified tumors in children younger than three years old, however, leads to a diagnosis of retinoblastoma. The lesion is usually localized in the posterior portion of the globe, extending into the vitreous (endophytic) or choroid (exophytic). Upon Doppler examination, internal vessels can be observed throughout the lesion. Astrocytic hamartomas and retinal astrocytomas are rare neoplasms derived from retinal nerve fibers or, uncommonly, from the optic nerve. They represent almost 3% of childhood leukocoria cases. Upon US examination, these lesions usually are highly reflective, often calcified and present posterior acoustic shadowing. In PHPV cases, highly reflective membrane shadows are observed on the papillary area, extending to the vitreous posterior third or to the crystalline posterior capsule (incomplete or complete form)(3) and associated with reduced anteroposterior diameter. This report describes a non-typical case that includes the observation of a mass on the papillary area, extending to the posterior pole with a membrane adhered to the lesion(9). These characteristics caused diagnostic uncertainty. US examination absence of internal calcifications on lesion and anechoic adjacent vitreous. Despite these results, the retinoblastoma hypothesis could still not be completely discarded(10).
Color Doppler revealed a linear blood flow in the internal mass acoustic shadow, which extended to the membrane adherent to this mass. This linear blood flow corresponded to the permeable hyaloid artery. This finding led to the final PHPV diagnosis(6) and adequate treatment was provided.
All diagnostic methods have their own limitations, reinforcing the importance of performing complementary exams. This will help reduce evaluation errors and consequently aid to adjust the conduct.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

