INTRODUCTION
Epithelial ingrowth is an infrequent but a potentially devastating complication of laser in situ keratomileusis (LASIK) surgery. Although the development of post-LASIK ingrowth is significantly reduced with femtosecond laser-assisted flap preparation, its rate markedly increases following LASIK enhancement(1,2). Intraoperative epithelial defect, flap integrity problems, hyperopic corrections, and diabetes mellitus have been identified as other risk factors in the development of post-LASIK epithelial ingrowth(3). Flap lifting and manual debridement of the epithelial sheets with adjunctive sutures, anti-metabolites, and tissue adhesives have been used in the treatment of advanced cases of post-LASIK ingrowth(4-6).
Ayala et al suggested an alternative, noninvasive approach in the treatment of post-LASIK epithelial ingrowth with Neodymium: Yttrium-Aluminum-Garnet (Nd-YAG) laser(7). They reported a success rate of 80% in 30 eyes of 25 patients without any complication over a 2-year follow-up. Herein we report Nd-YAG laser treatment outcome in a patient with recurrent post-LASIK epithelial ingrowth. To the best of our knowledge, the effect of Nd-YAG laser treatment in cases of multiple recurrences of post-LASIK epithelial ingrowth and a resultant flap melt have not been reported before.
CASE REPORT
A 35-year-old male patient with a history of bilateral LASIK performed 6 months earlier at another clinic presented with decreased vision and foreign body sensation in his right eye. The patient had undergone three successive flap lifts and epithelial cell scrapings in the past 2 months prior to his referral to our institution. There was no medical record of any preoperative readings or laser techniques being used for our patient.
The uncorrected distance visual acuity (UDVA) was 20/80 and the corrected distance visual acuity (CDVA) was 20/30 with a manifest refraction of -0.75 -2.75 × 95 in the right eye. Slit lamp examination was unremarkable with a visual acuity of 20/20 in the left eye. In the right eye, slit lamp examination demonstrated a significant epithelial ingrowth extending from the inferior flap edge and threatening the visual axis (Figure 1 A). Corneal topography demonstrated central and inferior flattening of the cornea consistent with previous myopic ablation in both eyes (Figure 2 A). Scheimpflug images demonstrated a wide side cut angle, indicating microkeratome-assisted flap preparation in our patient (Figure 2 B).
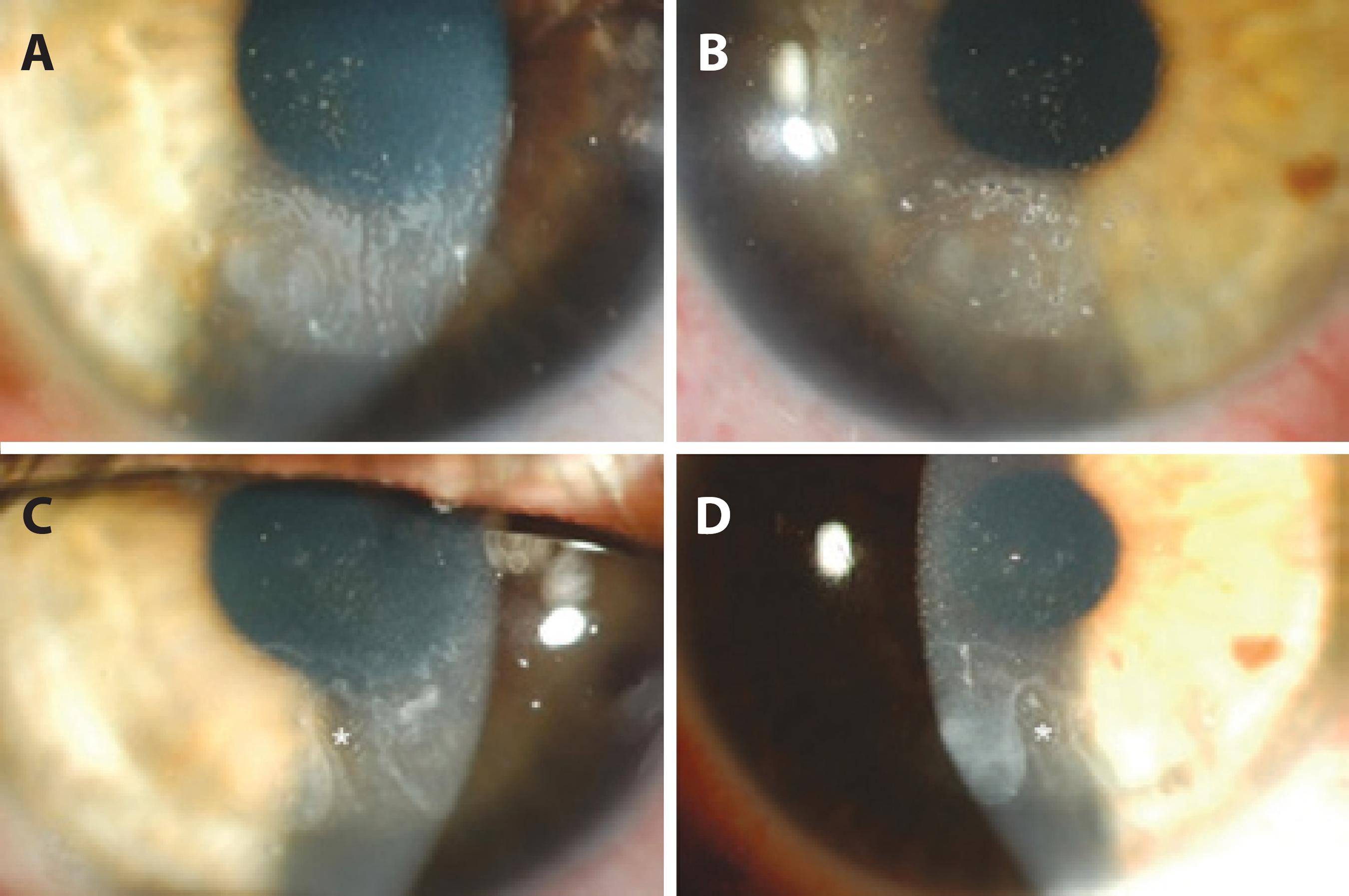
Figure 1 Slit lamp images showing, A) epithelial ingrowth, B) bubbles created by Nd-YAG laser during treatment, C) regressed ingrowth and flap melt one month after treatment, D) no recurrence at the 15-month follow-up. (Asterisk, area of flap melt).
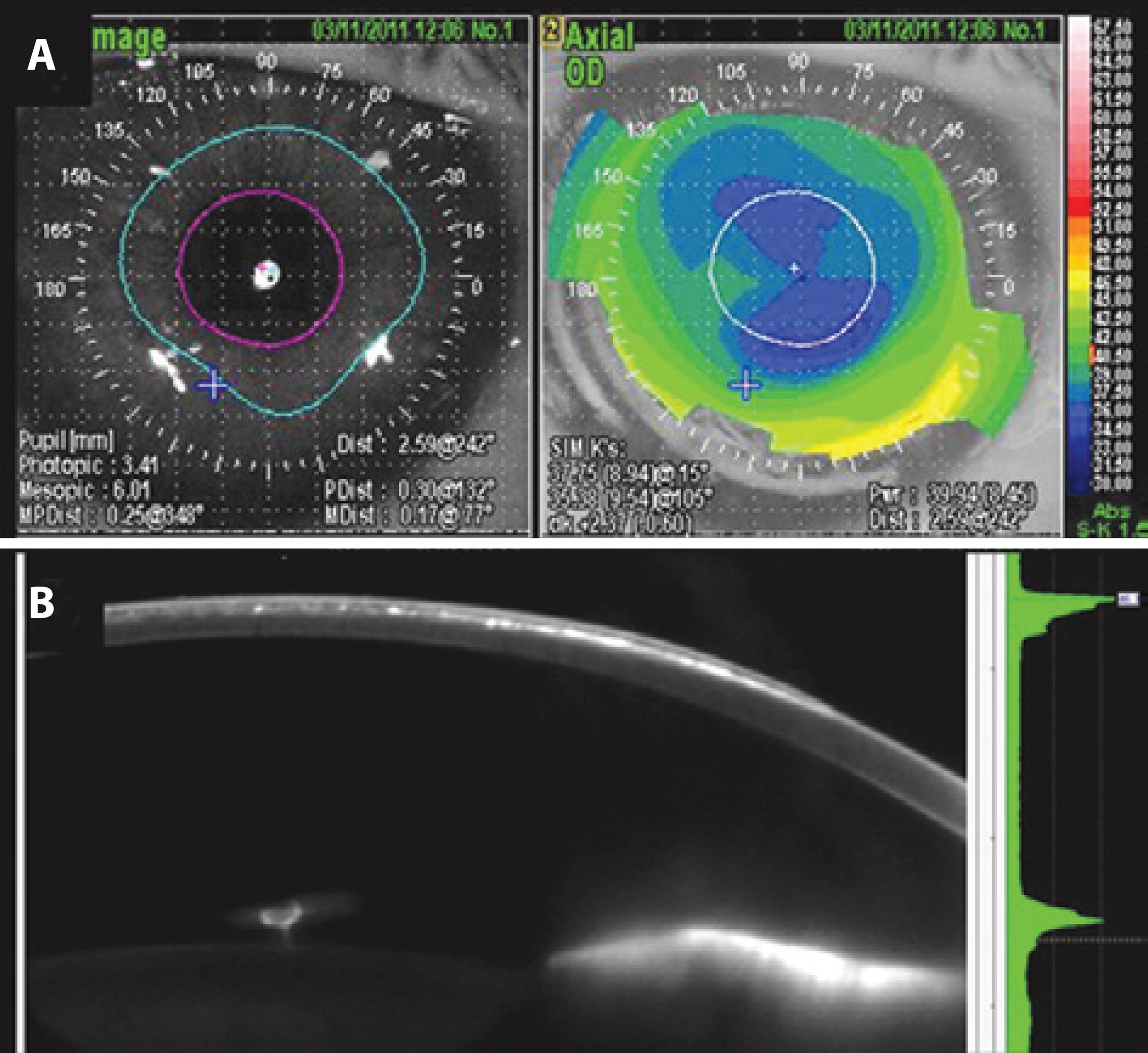
Figure 2 A) Preoperative topography demonstrating irregular astigmatism, B) Scheimpflug image indicating prior LASIK flap preparation.
The risks and benefits of various treatment options of managing epithelial ingrowth were discussed, and we proceeded with Nd-YAG laser treatment. Informed consent was observed. Laser treatment was performed under topical anesthesia. Nd-YAG laser was focused on the flap interface using the aiming beam of the laser system. We used a 1064-nm infrared Nd-YAG laser with an approximately 8-µm spot size with a 670-nm red diode laser as aiming beam (Visulas YAG III, Carl Zeiss Meditec Inc., USA). The treatment was started from the center of the epithelial ingrowth area. The energy level was set at
0.6 mJ and bubble formation was observed at the flap interface after treatment (Figure 1 B). The treatment was continued to cover the entire area of epithelial ingrowth. A total of 65 shots were performed. Topical fluorometholone drops (FML, Allergan, Istanbul) q.i.d. was used for 2 weeks.
One month after laser treatment the patient presented with total regression of the epithelial ingrowth. There were stromal haze at the flap interface with epithelial ingrowth and localized melt at the peripheral part of the flap (Figure 1 C). There was no foreign body sensation in the right eye; UDVA was 20/40 and CDVA was 20/30 with -0.50 -2.50 × 90 correction. At the 15-month follow-up visit, slit lamp findings and visual acuity of the patient were unchanged (Figure 1 D). There was no recurrence of the ingrowth at the last follow-up.
DISCUSSION
Our case demonstrates that Nd-YAG laser treatment is effective in cases with recurrences of post-LASIK epithelial ingrowth. Nd-YAG laser treatment resulted in complete resolution of the ingrowth and achieved significant improvement of symptoms without recurrences in our patient. However, we have also noted a localized melting in the peripheral part of the flap.
Probst and Machat reported a classification system classifying epithelial ingrowth into three grades: Grade 1, ingrowth limited to within 2.0 mm of the flap edge with no associated visual changes; Grade 2, thicker ingrowth at least 2.0 mm from the flap edge but with a normal edge anatomy; and Grade 3, pronounced ingrowth of >2.0 mm from the flap edge, often with anatomic abnormalities in the edge itself(8). Although observation appears sufficient for treating Grade 1 lesions, treatment is generally recommended for Grade 2 and 3 epithelial ingrowth because these lesions may cause disabling visual symptoms. The clinical properties of our patient were compatible with Grade 3 epithelial ingrowth. The reported high success rate with Nd-YAG laser in cases of primary post-LASIK epithelial ingrowth encouraged us to proceed with this procedure(7). In their initial report, 80% of the eyes showed complete resolution and the remainder (20%) showed partial resolution without any complications. Retreatment was required in 40% of the cases. The main differences between their and our cases were the history of multiple flap lifts performed and recurrences developing prior to Nd-YAG laser treatment. There are other reports showing promising results without any complications related to recurrences of post-LASIK ingrowth(9,10). We herein for the first time report flap melting as a treatment-related complication.
Recurrence of epithelial ingrowth and the presence of an excessive amount of epithelial cells at the flap interface are known factors increasing the risk of flap melt in post-LASIK epithelial ingrowth. The role of Nd-YAG laser treatment in the development of flap melt is not clear. Nd-YAG laser functions on the principle of creating small vacuoles at the focal point, which merge, thus producing large vacuoles, and the resulting acoustic waves disrupt the nearby tissue. The proposed mechanisms for flap melt as the disruption of the balance of proteolytic enzymes at cellular level and the damage to the nearby tissues related to microkeratome flap creation may be applied to Nd-YAG laser treatment(11,12). Laser energy levels or number of laser shots performed in the same area may determine the development of flap melt in our patient. Flap melt likely could have been prevented by using more than one laser session with fewer laser shots.
In conclusion, Nd-YAG laser treatment is a promising alternative for treating recurrent post-LASIK epithelial ingrowth. However, the exact role of the Nd-YAG laser in the development of localized flap melt in our case could be elucidated. Therefore, we believe that this novel technique needs to be studied further to determine the limitations of indications and laser settings to prevent flap melt or other undesirable outcomes. Moreover, performing repeated laser shots in the same area may increase the risk of flap melt in this novel technique.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

