INTRODUCTION
Multiple evanescent white dot syndrome (MEWDS) was first described by Jampol et al.(1), and in the same year by Takeda et al.(2). Its pathophysiology is believed to be characterized mainly by photoreceptor layer disruption(3). It is an uncommon choroidoretinal syndrome that usually presents as a unilateral multifocal retinitis, and more commonly affects women in a 4:1 female:male ratio(1,2). Considering this information, we analyzed the fluorescein angiography (FA) data from the retina department and compared the data with the existing literature.
The symptoms usually start with flu-like complaints, followed by photopsias, scotomas, and low vision. Ophthalmoscopy is the most common diagnostic method, although FA, electroretinogram, visual field test, and optical coherence tomography (OCT) may also help to confirm the diagnosis.
The typical presentation of this syndrome includes the presence of multiple white dots at the fundus extending from the posterior pole to the near peripheral retina, with some cases followed by discrete vitritis and foveal granularity. The latter characteristic is highly indicative of MEWDS when associated with white dots and/or spots(4).
MEWDS is often a self-limiting condition, which evolves to complete resolution and visual acuity recovery, although there may be retinal sequelae in a few cases(4).
Angiographic characteristics may vary in eyes with similar clinical signs of MEWDS. This variation may reveal the different anatomic structures involved during the natural course of the disease. The FA of the white dots exhibit a fine halo appearance in a wreath-like swirl configuration to some of the white dots, and this halo diffuses in the later stages of the angiogram, first developing a stippled pattern of fluorescence, and then becoming a diffuse white spot that only mildly leaks fluorescein. There may be fluorescein leakage from the optic nerve, and occasionally, there may be late staining of the retinal blood vessels due to a mild vasculitis. Incidentally, final recovery is not related to the initial angiographic lesions(5).
Considering its good prognosis, we aimed to study the epidemiology of MEWDS to confirm the usefulness of FA as a complementary tool that is accessible at most ophthalmic clinics, which could allow MEWDS-like lesions to be identified more easily, thus ensuring good prognosis, and avoiding unnecessary treatment.
METHODS
The study consisted of a cross-sectional retrospective analysis of all the FA performed at the retina department from July 2006 to October 2012, including 6111 patients. All exams were analyzed, then the MEWDS-like angiograms were selected. All the cases diagnosed as MEWDS were examined by the retina coordinator, and their FA were reviewed for both the patients’ eyes, thus determining the frequency of this disease in the study population and allowing analysis of the angiographic aspects (FA patterns: presence of punctuate hyperfluorescent dots, patchy spots, optic disc leakage of fluorescein, and foveal granularity) detected in each exam. The patients were referred from the ophthalmic emergency room, and those who needed low visual acuity investigation underwent FA exam on the same day, which allowed early-stage lesions to be detected.
Epidemiological data were collected in terms of the patients’ age, sex, affected eyes (uni or bilateral), and the chief complaint, including the length of the clinical symptoms.
RESULTS
Among the 6,111 FA studied, only 0.24% (15 patients) were diagnosed with MEWDS; 60% were male (nine patients) and 40% were female (six patients). The female/male ratio was 0.7/1, which differs from the existing literature(1).The age of the patients ranged from 13 to 42 years.
Chief complaints varied, and included photopsias, central scotomas, and diffuse blurred vision, which disappeared within 1 to 8 weeks from the first symptom until total recovery.
The best-corrected visual acuity varied from 20/20 to 20/200, evolving to 20/20 in 14 (93.3%) of the patients (Figure 1). The only patient who did not recover his visual acuity presented multifocal choroiditis (MFC) and MEWDS with permanent macular damage.
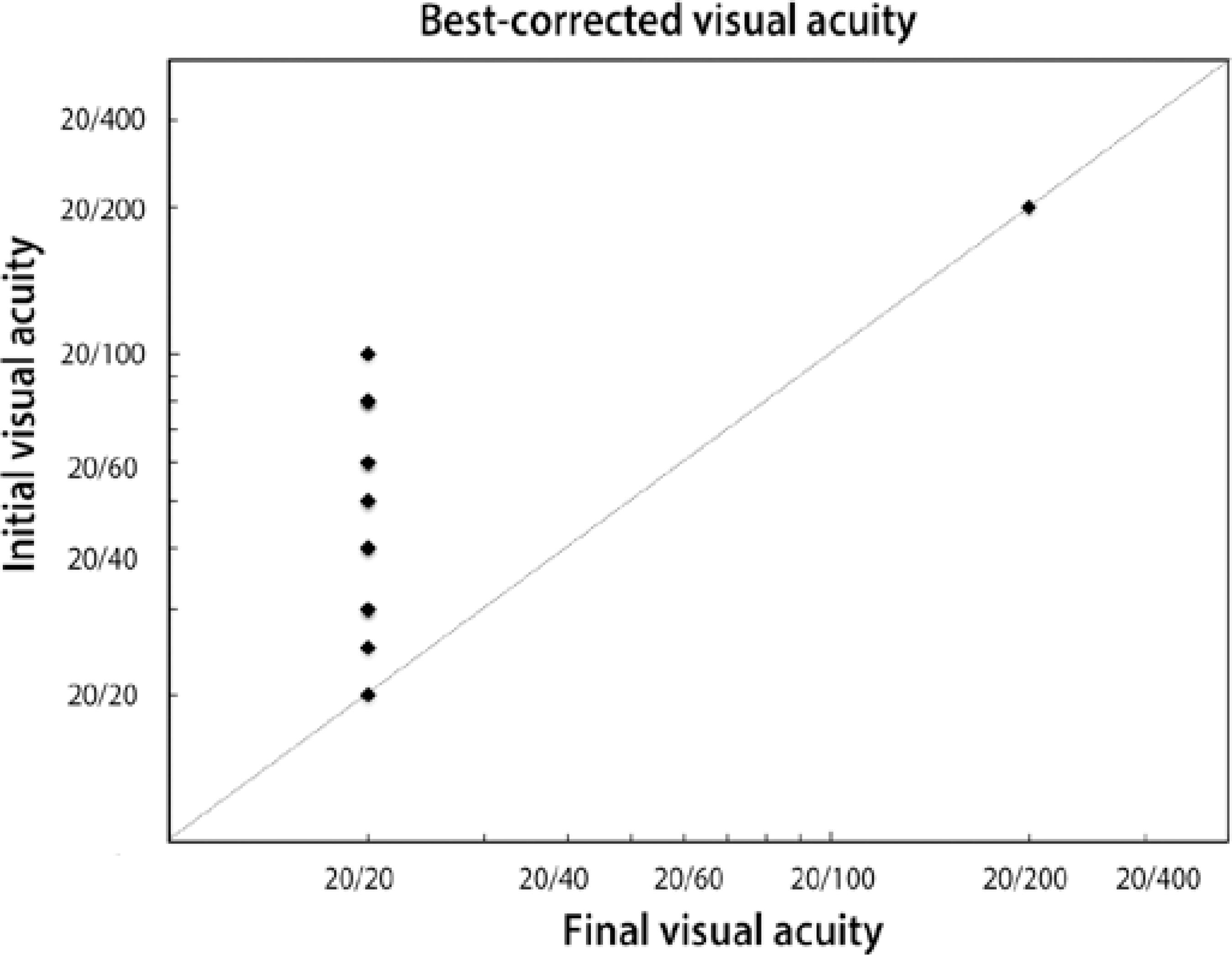
Figure 1 Change in initial visual acuity to final visual acuity in each of the 15 patients diagnosed with MEWDS.
The main angiographic findings included: only hyperfluorescent dots (26.6%, four patients), only hyperfluorescent patchy spots (33.4%, five patients), and both dots and spots (40%, six patients). Atypical findings such as optic disc hyperfluorescence were detected in 66.6% (10 patients). Foveal granularity was detected in 46.6% (seven patients), with 57.1% (four patients) of these being female. Multifocal choroiditis association and vasculitis were found in 6.6% (one patient) (Table 1, Figures 2 and 3). Notably, bilateral hyperfluorescent lesions were detected in all of the patients in this study, even without any symptoms in the fellow eye.
Table 1 Distribution of the typical and atypical fluorescein angiography lesion patterns observed in patients with MEWDS
| Fluorescein angiography findings | Patients | |
|---|---|---|
| Typical | ||
| Hyperfluorescent dots | 26.6% | |
| Hyperfluorescent patchy spots | 33.4% | |
| Associated dots and spots | 40.0% | |
| Atypical | ||
| Optic disc hyperfluorescence | 66.6% | |
| Foveal granularity | 46.6% | |
| Multifocal choroiditis | 6.6% | |
| Vasculitis | 6.6% | |
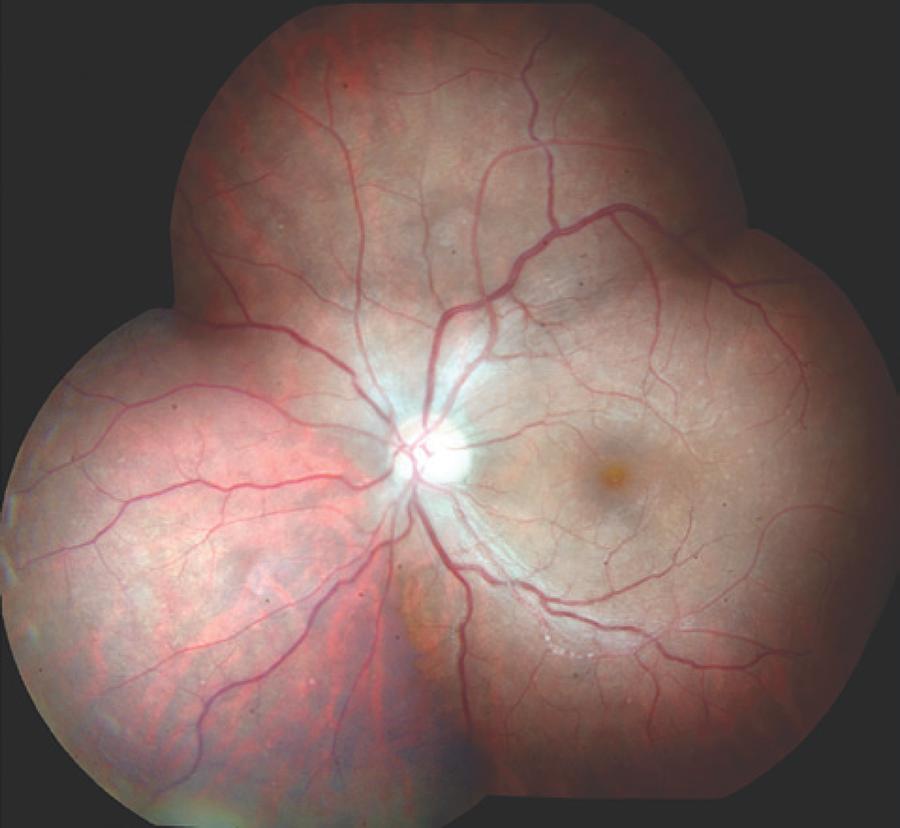
Figure 2 Young male presenting photopsias and blurred vision lasting 4 days (best-corrected visual acuity: 20/40 Snellen). Note the white dots at the posterior pole and associated inferior vasculitis. Total vision acuity recovery was achieved in 4 weeks (author's archive).
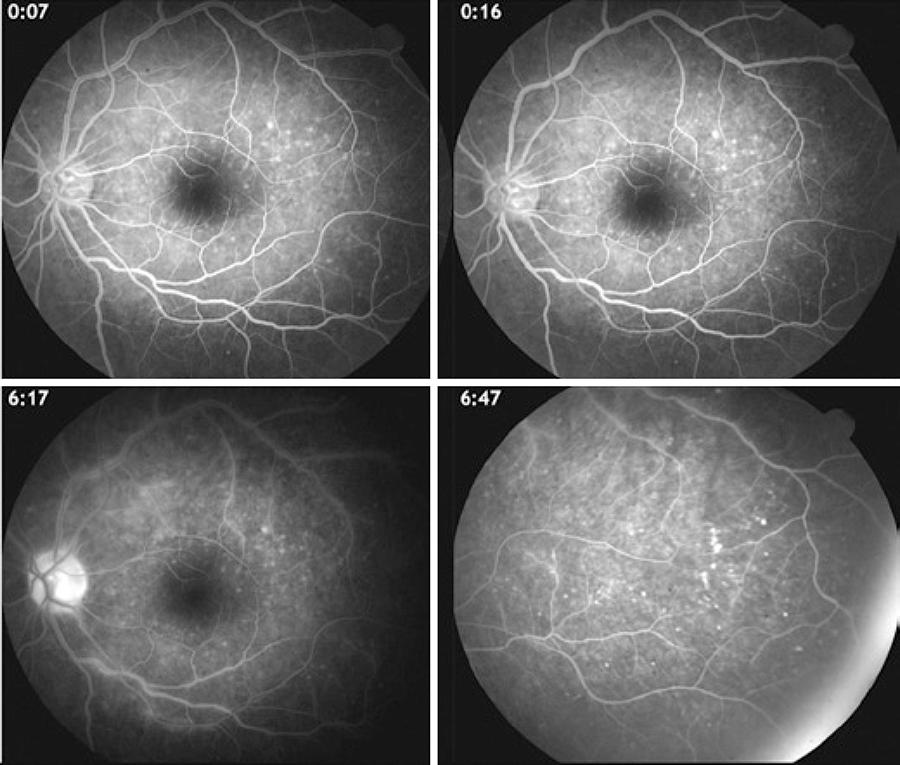
Figure 3 The same patient from figure 2, showing hyperfluorescent dots in a wreath-like swirl configuration at the posterior pole and temporal periphery. Note the perivascular hyperfluorescence at the inferior blood vessel adjacent to the optic disc (author's archive).
DISCUSSION
Characteristic FA findings in MEWDS might contribute to its diagnosis, although some atypical FA aspects, such as foveal granularity without the typical white dots and associated vasculitis, were found in this study (Figures 2 and 3)(6,7).
Besides FA, other complementary exams can reveal MEWDS-like lesions, including indocyanine green angiography and autofluorescence exams showing hypocyanescent and hypo-autofluorescent lesions, respectively, which correspond to the white dots and other lesions not detected during ophthalmoscopic examination(8-11).
OCT has been used to study the MEWDS macular lesions, to demonstrate that all abnormalities at the inner-outer photoreceptor segments recovered during the course of the disease(12). Spectral domain OCT can detect very small ruptures in the photoreceptor layer in MEWDS cases(13,14). However, there is strong evidence that, even with unilateral symptoms, the photoreceptor layer changes in both eyes, restoring itself spontaneously, as was shown in most of the FA findings in this study(15).
Studies on the association of MEWDS with other diseases have mainly focused on MFC, revealing cases of simultaneous MEWDS and MFC, although MFC can sometimes occur months after MEWDS(15-17). MEWDS has also been associated with acute idiopathic blind spot enlargement syndrome, acute macular neuroretinopathy, and acute zonal occult outer retinopathy(18-20).
There are rare and isolated cases of postvaccinal MEWDS related to hepatitis B, meningitis, and human papillomavirus vaccines, although there is no confirmed infectious etiological relationship(21,22).
In terms of the low frequency of MEWDS in our study population, with 15 MEWDS patients diagnosed from the 6111 FA performed (0.24%), larger studies and meta-analyses may be necessary in order to follow up these patients and ensure good prognosis. This is important because some patients can relapse, sometimes years after the first episode(6). An interesting feature found in this study was the higher frequency in male patients (60% male to 40% female), which contradicts the female predominance found in the existing literature(18).
The angiographic characteristics, either from FA or indocyanine green angiography, can vary in patients with similar visual complaints. According to previous studies, the reason for this is that there are many other ocular structures involved in the physiopathology of this disease(5). Moreover, it is important to highlight that, in apparently normal fundoscopy patients with scotomas and photopsias, dots and spots at the near peripheral retina can be found via FA, suggesting MEWDS. In this study, both eyes were affected in all of the patients, even without any symptoms in the fellow eye. The eyes without symptoms showed discrete lesions (hyperfluorescent dots and spots), thus also suggesting MEWDS. Therefore, careful examination by an experienced retina specialist is imperative in order to detect discrete lesions during clinical examination.
On the other hand, many types of infectious retinitis may be masked by MEWDS. This could be true for some patients in this study that were not followed up after recovery, thus resulting in data that differs from those in previous reports(21–23).
MFC associated with MEWDS has been detected in some studies, and was also found in the present study (6.6% of the patients studied). On the other hand, MEWDS lesions are known to disappear spontaneously, while MFC leaves choroidoretinal scars. The relationship between MFC and MEWDS may indicate a common etiological factor(16). In these cases, multifocal electroretinogram can help to differentiate MFC from MEWDS, with deep wave depression in MFC and an initial focal loss in MEWDS, followed by full recovery of retinal function at about 7-14 days(24,25).
CONCLUSION
MEWDS is an uncommon but self-limiting disease with good prognosis, which can be associated with other immunological diseases. In this study, 93.3% of the patients recovered total vision, confirming the good prognosis of this syndrome.
FA needs to be emphasized as a useful complementary tool for MEWDS diagnosis, even to confirm or to exclude differential diagnoses such as acute posterior multifocal placoid pigment epitheliopathy, Birdshot chorioretinopathy, diffuse unilateral subacute neuroretinitis, and the other diseases that comprise the white dot syndromes. The present study allowed easier detection of MEWDS-like lesions through FA in association with the patient’s clinical history and follow-up, thus characterizing the course of the disease, which has a good prognosis. Note that FA patterns might vary in each patient, including hyperfluorescent dots and/or patchy spots, hyperfluorescent optic disc, and foveal granularity, which were the most common FA findings in this study. Possible variations from the complementary exams should also be considered. In conclusion, MEWDS is not often diagnosed in Rio de Janeiro, which is probably due to patients’ later arrival for ophthalmic assistance and lack of recognition at the emergency fundoscopy examination. Nevertheless, it is important to consider the methodological weaknesses of retrospective studies.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

