INTRODUCTION
Posterior capsule opacification is the most common complication of cataract surgery and results from the proliferation and migration of residual lenticular epithelial cells(1-3). Opacification may be diminished by atraumatic surgery, complete cleaning of cortex residues, polishing of both anterior and posterior capsules, or the use of specific intraocular lens (IOL) designs(1,4). The overall incidence of posterior capsule opacification (PCO) approaches 50% at 5 years following cataract surgery(5-7) and disproportionately affects younger patients due to higher cell proliferation rates(8). PCO decreases visual acuity and contrast sensitivity leading to disability as a result of glare(9,10). Nd:YAG laser capsulotomy has utility in the treatment of PCO; however, a number of complications of this procedure have been reported including IOL dislocation leading to hyperopia, IOL subluxation or luxation, IOP elevation, cystoid macular edema, and retinal detachment(11-13).
A number of Nd:YAG laser capsulotomy shapes and sizes may be utilized. Cruciate and circular shapes are most commonly performed with a wide range of opening sizes (3-6 mm). Specific capsulotomy shapes and sizes confer particular advantages and disadvantages(14,15). In this study, we evaluated the effect of Nd:YAG capsulotomy size and shape on visual outcomes.
METHODS
The study protocol was approved by the local ethics committee. Informed consent was obtained from patients prior to the procedure. The study was carried out in accordance with the tenets of the Declaration of Helsinki.
We retrospectively evaluated 85 eyes of 67 patients treated with Nd:YAG laser posterior capsulotomy for PCO between November 2011 and July 2012. Phacoemulsification and IOL implantation surgery had previously been performed on all eyes, although at different times.
All patients reported blurred vision prior to surgical intervention. All Nd:YAG laser capsulotomy procedures were performed by a single surgeon (SC) under topical anesthesia using an ophthalmic Nd:YAG laser (Visulas YAG II, Zeiss, Germany) with capsulotomy contact lenses (Double aspheric capsulotomy lens, Volk, USA). One drop of a dorzolamid-timolol maleate combination was applied both before and after the procedure to prevent immediate increases in IOP following the procedure. A topical steroid (1% dexamethasone sodium phosphate, Dexasine, Liba, USA) was prescribed for use 4 times a day for one week following the procedure.
Full ophthalmological examinations, including uncorrected visual acuity, best-corrected visual acuity (BCVA), refractive measurements, IOP measurements, biomicroscopic evaluation, and fundus examination, were performed both before and after the procedure. Patients with ocular or systemic diseases likely to affect vision were excluded from the study.
Patients were divided into 4 groups according to the shape and size of capsulotomy performed. Groups comprised patients with cruciate shape capsulotomies with openings of less than or equal to 3.5 mm (Group 1, 20 eyes) or greater (Group 2, 23 eyes) and patients with circular shape capsulotomies with openings of less than or equal to 3.5 mm (Group 3, 19 eyes) or greater (Group 4, 23 eyes).
SE, BCVA, and IOP were compared within groups and between groups prior to and at 1 month following capsulotomy. The number and energy of laser firings, and the number of patients reporting floating bodies, were also evaluated.
All statistical analyses were performed using commercially available statistical software (SPSS version 22, SPSS, Inc., Chicago, IL). Data were compared using the Chi-Square test, Wilcoxon Signed Ranks test, Mann-Whitney U test, or Kruger Wallis test as appropriate. P values of less than 0.05 were considered statistically significant.
RESULTS
Eighty-five eyes of 67 patients were included in this study. Thirty-two patients were male (47.7%) and 35 were female (52.3%). Forty-nine patients had unilateral PCO (73.1%) and 18 patients had bilateral PCO (26.9%). The mean age was 57.57 ± 9.26 years (38-75). The mean interval between surgery and Nd:YAG laser capsulotomy was 26.09 ± 7.08 months (10-38). No significant difference in the interval between surgery and Nd:YAG laser capsulotomy was observed between groups (p=0.97). No statistically significant differences in age or gender were observed between groups (p=0.254 and p=0.49, respectively).
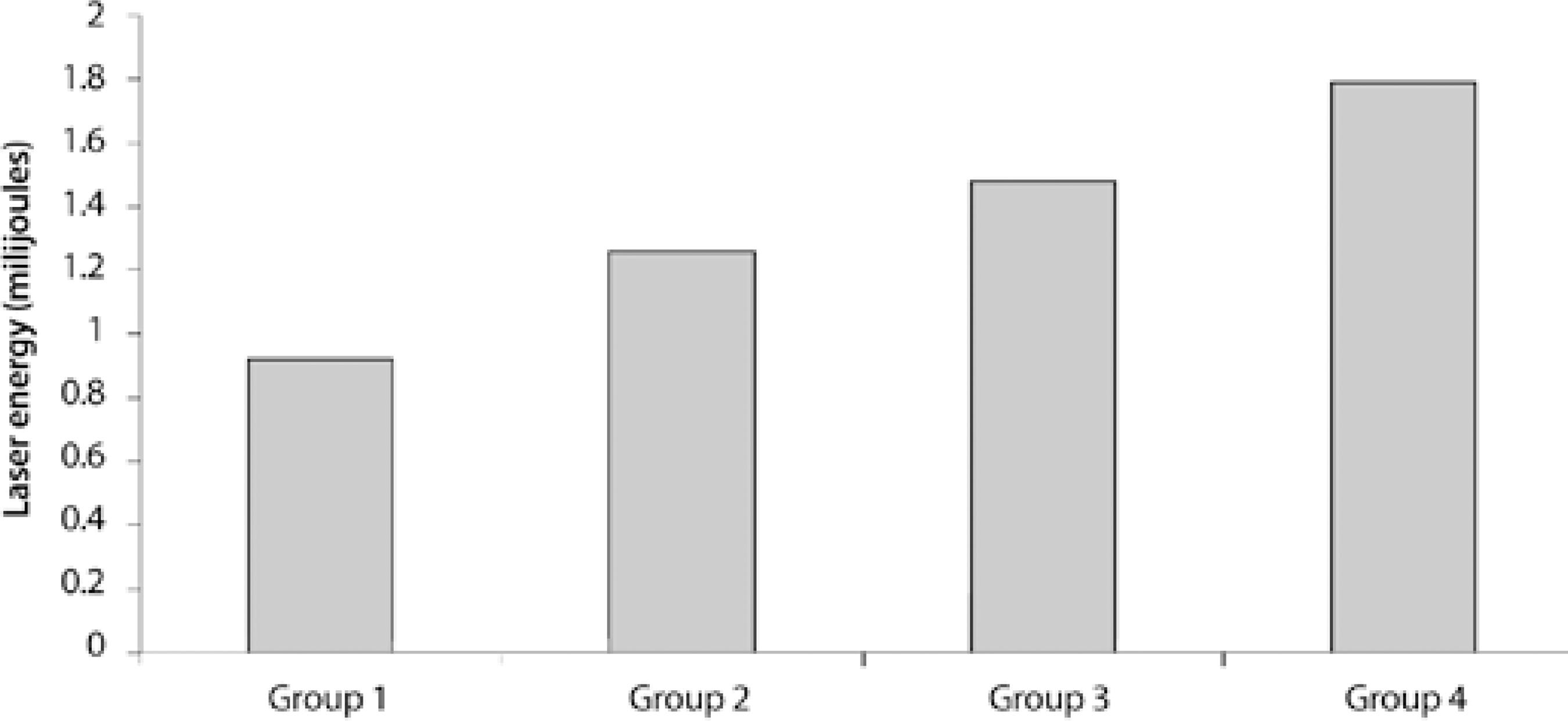
The mean applied laser energy in Group 1 was 0.92 ± 0.12 milijoules (0.8-1.2), 1.26 ± 0.15 milijoules (0.9-1.5) in Group 2, 1.48 ± 0.19 milijoules (1.00-1.8) in Group 3, and 1.79 ± 0.25 milijoules (1.2-2.00) in Group 4. The mean applied laser energy was significantly greater in Group 4 compared with that in other groups (p=0.01). The mean applied laser energy in Group 1 was significantly less compared with that in other groups (p=0.01, Figure 1).
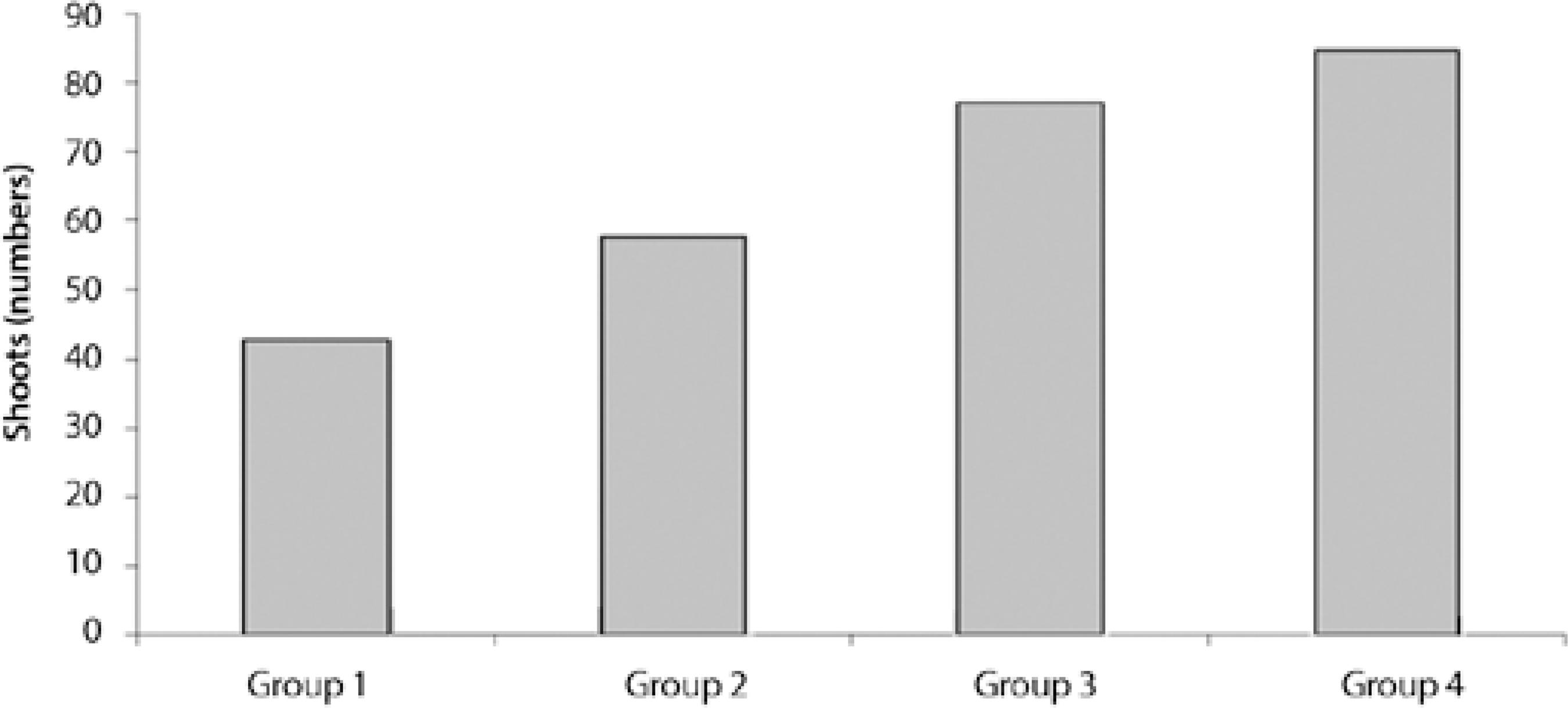
The mean number of laser firings was 42.65 ± 11.62 (32-72) in Group 1, 57.60 ± 10.54 (35-83) in Group 2, 77.15 ± 13.17 (50-99) in Group 3, and 84.69 ± 13.44 (65-110) in Group 4. The mean number of laser firings was significantly higher in Group 4 compared with that in other groups (p=0.00). The mean number of laser firings was significantly lower in Group 1 compared other groups (p=0.00, Figure 2).
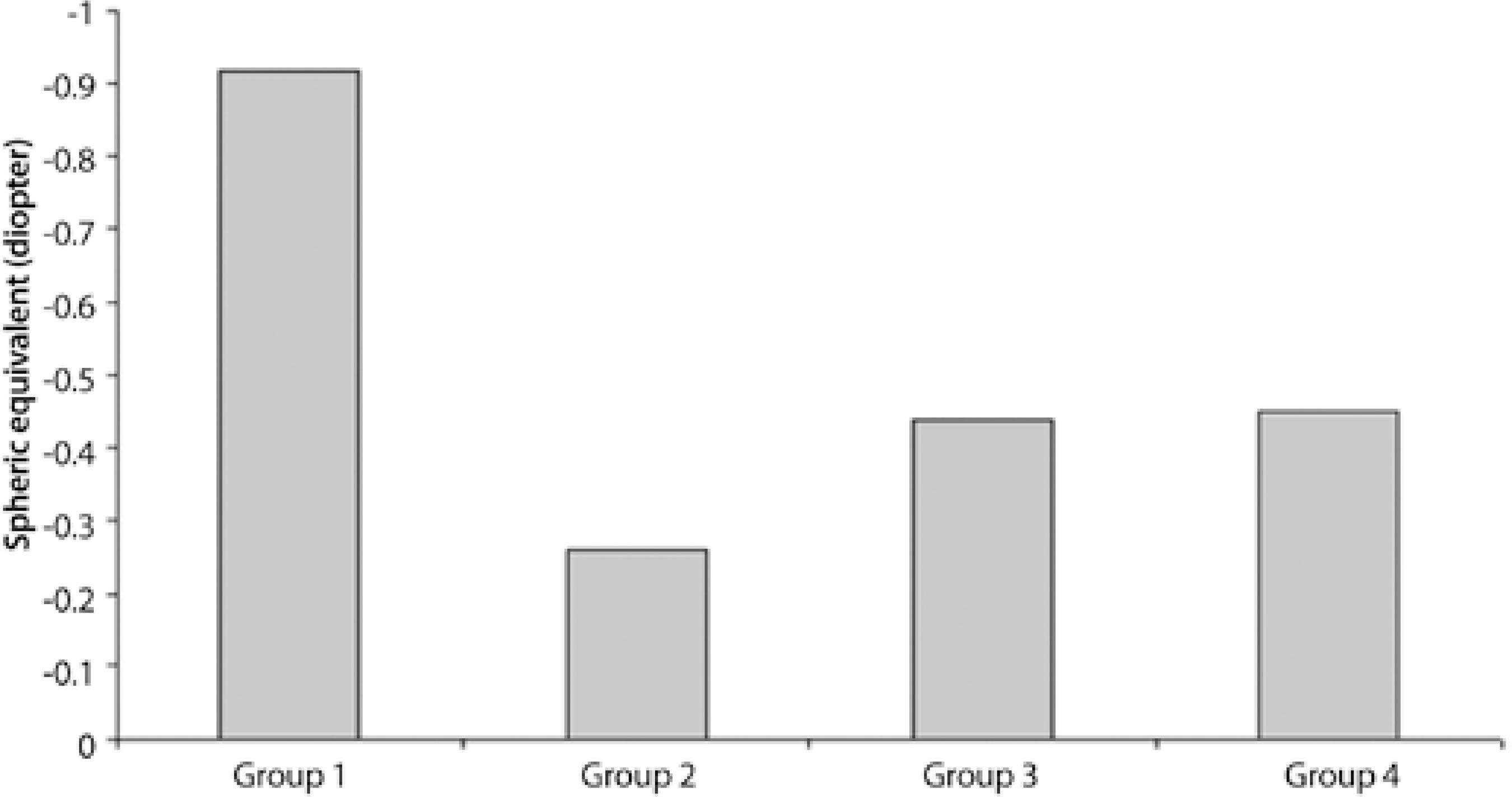
The mean pre-procedural SE was -0.92 ± 0.67 diopter (0.00-2.00) in Group 1, -0.34 ± 0.41 diopter (0.00-1.00) in Group 2, -0.50 ± 0.52 diopter (0.00-1.50) in Group 3, and -0.50 ± 0.67 diopter (0.00-2.00) in Group 4. The mean pre-procedural SE was significantly higher (more myopic) in Group 1 (p=0.026). The mean post-procedural SE was -0.92 ± 0.74 diopter (0.00-2.00) in Group 1, -0.26 ± 0.42 diopter (0.00-1.00) in Group 2, -0.44 ± 0.55 diopter (0.00-1.50) in Group 3, and -0.45 ± 0.65 diopter (0.00-2.00) in Group 4. The mean post-procedural SE was significantly higher (more myopic) in Group 1 (p=0.011, Figure 3). No significant change in SE following capsulotomy was observed in any group (p=0.074).
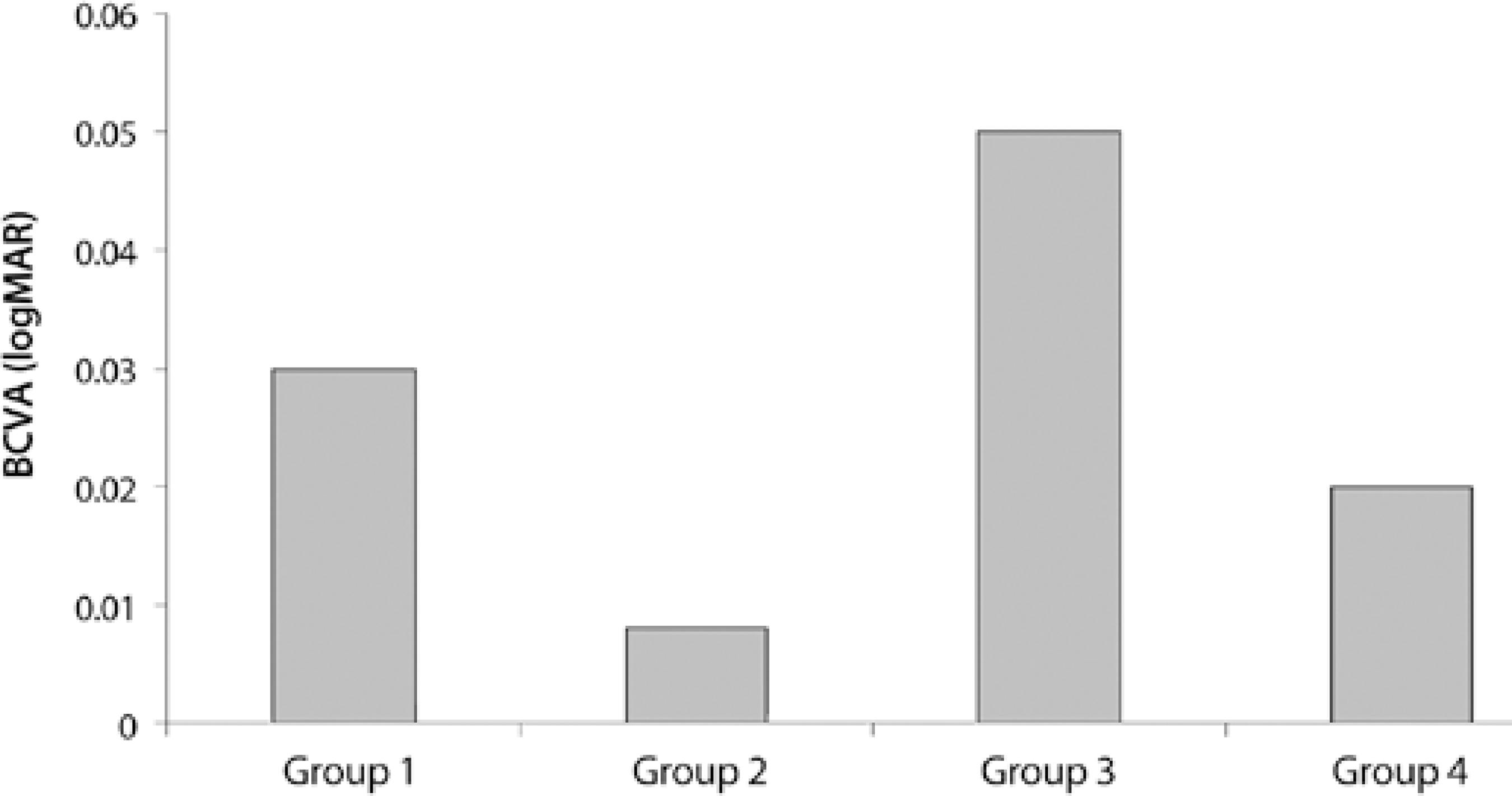
The mean pre-procedural BCVA was 0.54 ± 0.22 logMAR units (0.20-0.90) in Group 1, 0.58 ± 0.12 logMAR units (0.20-0.80) in Group 2, 0.54 ± 0.23 logMAR units (0.20-0.90) in Group 3, and 0.51 ± 0.20 logMAR units (0.20-0.90) in Group 4. There was no statistical difference between groups (p=0.44). The mean post-procedural BCVA was 0.03 ± 0.06 logMAR units (0.00-0.20) in Group 1, 0.008 ± 0.02 logMAR units (0.00-0.10) in Group 2, 0.05 ± 0.07 logMAR units (0.00-0.20) in Group 3, and 0.02 ± 0.05 logMAR units (0.00-0.20) in Group 4. There was no statistical differences between groups (p=0.108, Figure 4). BCVA significantly improved in all groups following capsulotomy (P<0.01).
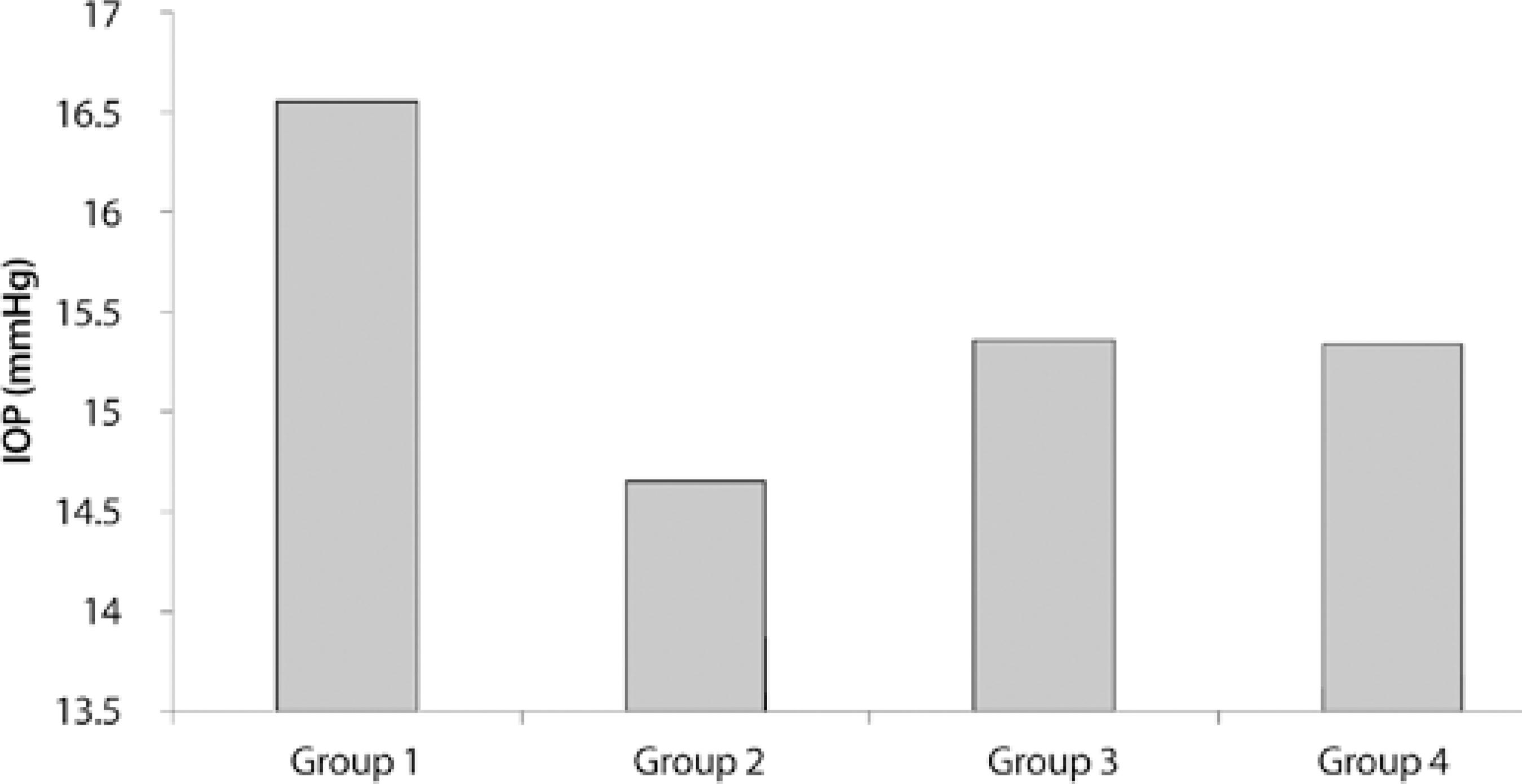
The mean pre-procedural IOP was 16.15 ± 2.71 mmHg (10-20) in Group 1, 14.86 ± 2.63 mmHg (11-19) in Group 2, 15.31 ± 3.59 mmHg (9-21) in Group 3, and 15.43 ± 1.94 mmHg (2-19) in Group 4. There was no statistical differences between groups (p=0.452). The mean post-procedural IOP was 16.55 ± 2.48 mmHg (11-21) in Group 1,14.65 ± 2.56 mmHg (10-18) in Group 2, 15.36 ± 3.23 mmHg (11-21) in Group 3, and 15.34 ± 1.96 mmHg (12-19) in Group 4. There was no statistical differences between groups (p=0.125, Figure 5). No significant change in IOP following capsulotomy was observed in any group (p=0.856).
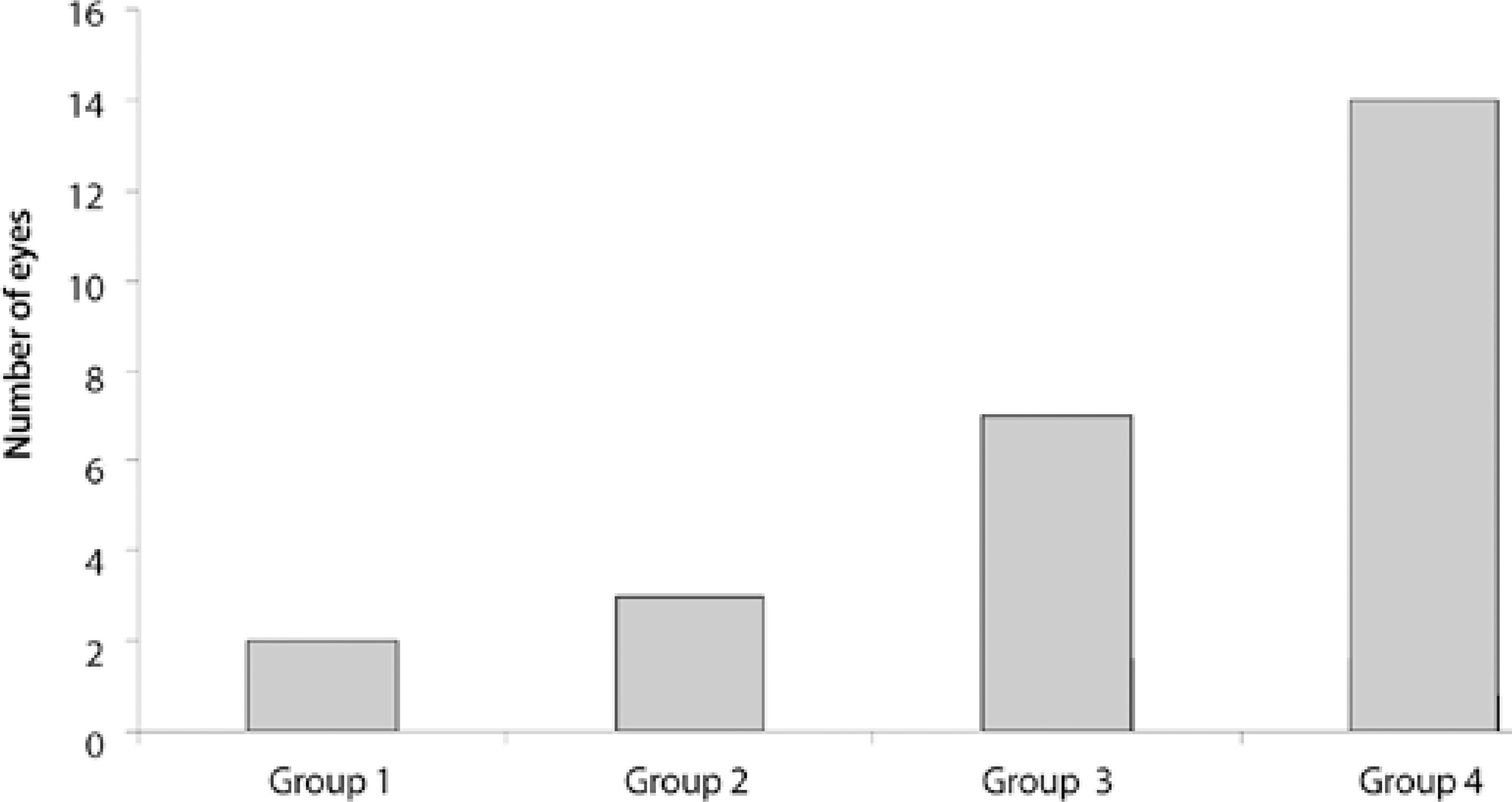
Floating bodies were reported in 2 eyes (10%) in Group 1, 3 eyes (13%) in Group 2, 7 eyes (36%) in Group 3, and 14 eyes (60%) in Group 4. Floaters were reported in a significantly higher proportion of eyes in Group 4 than in other groups (p=0.001). Floaters were reported in a significantly lower proportion of eyes in Group 1 than in other groups (p=0.001), however, no significant difference in the frequency of floating bodies was observed in Group 2 (p=0.759) or Group 3 (p=0.05) compared with that in Group 1 (Figure 6).
DISCUSSION
The main goal of Nd:YAG laser capsulotomy is to increase visual acuity, however improving contrast sensitivity and decreasing disability due to glare are also important(9,10,12). Smaller capsulotomy openings limit visual acuity by diffraction and result in light passing through the unopened region of the capsule being scattered causing glare and decreasing contrast sensitivity. Capsulotomy opening should therefore be equal to, or larger than, the size of pupil in scotopic conditions(10,16). However, capsulotomy openings should be large enough to ensure good visualisation of the peripheral fundus, particularly in patients with retinal disease.
On the other hand, larger capsulotomy openings may increase risk of cystoid macular edema, vitreous prolapse, and retinal detachment(11,17)or cause posterior IOL dislocation leading to hyperopia(18). In addition, a higher amount of energy is required that may increase the risk of retinal detachment(19).
Refractive changes and visual acuity are usually not affected by the size and shape of capsulotomy(13-15). However, floaters are more frequently reported, and the amount of energy used is higher, in circular shape capsulotomies(15).
In our study we did not observe any complications related to Nd:YAG laser capsulotomy. Our study found no significant changes in refraction, visual acuity, or IOP in any groups following Nd:YAG capsulotomy. However, the amount of energy used, the number of laser firings, and the proportion of patients complaining of floaters were significantly higher in Group 4 (large, size circular shape capsulotomy). More energy and thus more laser firings are required to form larger circular shape capsulotomies resulting in more floating bodies in the anterior vitreous. Additionally, the amount of energy used, the number of laser firings, and floater complaints were significantly lower in Group 1 (small size, cruciate shape capsulotomy), however floater complaints in this group did not significantly less differ from Group 2 (big size, cruciate shape capsulotomy) or Group 3 (small size, circular shape capsulotomy).
In conclusion, cruciate shape capsulotomy with an opening of 3.5 mm or less provides the greatest improvement in visual function with minimal complications.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

