INTRODUCTION
The first description of the resection of uveal tumors dates back to the early twentieth century( 1 ). The interest in the techniques for the resection of ciliary-choroidal tumors increased in the 1980s, when it was noted that radiotherapy resulted in many complications in the treatment of large anterior uveal tumors( 2 ).
Several researchers reported different techniques for resection of these tumors( 3 - 7 ). Most of them used scleral delamination with en bloc tumor resection and described the technique using different names, including cycle-choroidectomy, lamellar sclero-uvectomy, choroidectomy, trans-scleral resection, en bloc resection, and eye wall resection. Herein, we report five cases uveal tumors that were subjected to this procedure.
METHODS
Five eyes from five patients with uveal tumors were subjected to surgical en bloc tumor resection. The indication for surgery depended on the size and location of the tumor and preoperative visual acuity (VA). All tumors were >5 mm thick and none were located in the posterior region or in close proximity to the optical disc.
Preoperative VA was 20/40 or better in all eyes. Before surgery, a systemic evaluation was performed to discard metastatic disease, and the patients were adequately informed about the treatment to be performed.
Two weeks before surgery, laser photocoagulation was performed using three laser beams around the tumor, extending anteriorly to the ora serrata in cases with tumors involving the choroid and ciliary body. The surgery began with conjunctival peritomy and transposition of the extraocular muscles. Subsequently, tumor transillumination was performed with a transilluminator (Model OS 3000, MIRA; Waltham, USA) to precisely define the boundaries of the tumor on the scleral surface. Ocular muscles in the resection bed that were liable to damage were detached from the sclera and re-attached after tumor removal.
Scleral wall delamination was performed in two-thirds of the scleral thickness and respecting a safety margin of 2–3 mm of the tumor boundaries that were previously demarcated (Figure 1).
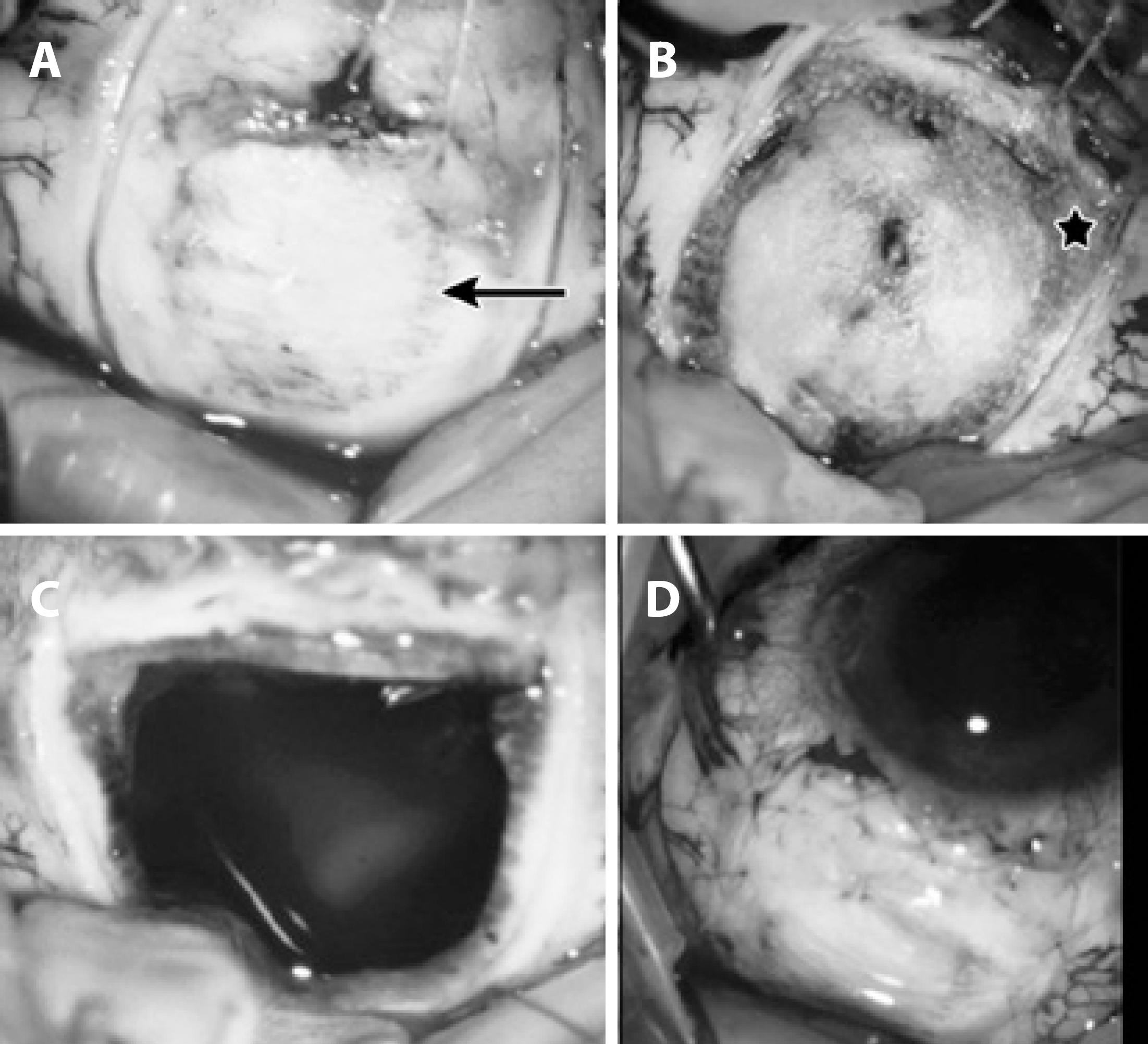
Figure 1 A) Eyeball showing sclera and inferior rectus muscle removed from the insertion. After transillumination (arrow), uveal tumor boundaries were demarcated with scleral tono-pen, and delamination was performed in two-thirds of the scleral wall respecting the tumor safety margin of 2-3 mm. B) Eyeball showing delaminated scleral flap and diathermy marks (star) at the edge of the delamination over the remaining scleral bed. C) Scleral wall was removed en bloc with the tumor and apparent vitreous humor. D) Scleral flap was sutured with nylon 9/0.
Subsequently, diathermy of the scleral bed was performed at the junction between the delaminated and non-delaminated sclera to prevent bleeding during incision (Figure 1B). A pars plana vitrectomy infusion line was placed away from the area to be resected. Subsequently, an incision in the delaminated sclera, choroid, and retina was performed for en bloc resection of the tumor (Figure 1C), and the remaining scleral flap was sutured with nylon 9/0 (Figure 1D). Finally, vitrectomy was performed to remove clots and vitreous bands attached to the incision, fluid-gas exchange, and air injection into the vitreous cavity.
After surgery, all patients were monitored by means of eye examination and oncological evaluation to detect metastases postoperatively.
RESULTS
The patients (four women and one man) were aged 31-61 years. The resected tumor diameter varied between 8 mm and 15 mm, and the thickness varied between 5 mm and 11 mm. In three eyes, the tumor involved the ciliary body and choroid, and in two eyes, it involved only the choroid. The posterior limit of the latter two eyes exceeded the eye equator (Figure 2).

Figure 2 Postoperative en bloc resection of choroidal melanoma, which extended beyond the limits of the eye equator. The white area corresponds to the remaining scleral flap.
Histopathologic examination indicated three cases of melanoma (two with spindle type B cells and one with mixed cells), one case of leiomyoma, and one case of medulloepithelioma (Figure 3). In addition, the margin of the resected area was free of tumor cells in all cases.
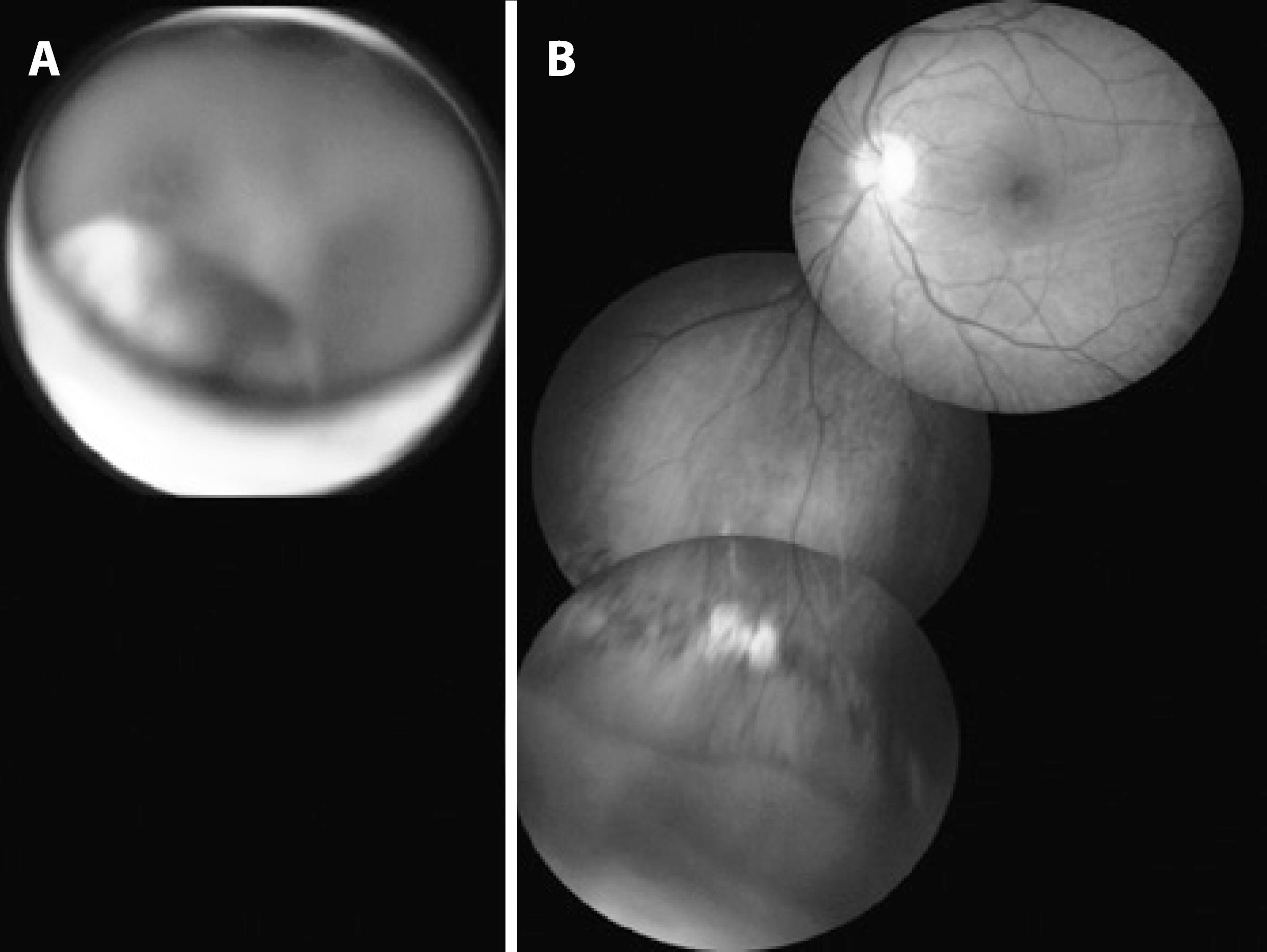
Figure 3 A) Preoperative medulloepithelioma in the ciliary body region. B) Postoperative retinal attachment; the whitish area on the periphery corresponds to tumor resection delimited by photocoagulation marks.
Patient follow-up period varied between 6 and 23 years. In all eyes, cataracts were observed between 6 and 24 months after the procedure and were successfully operated. The final VA was 20/20 in the affected eyes of three patients (Figure 4). The affected eye in the fourth patient resulted in retinal detachment 60 days after the initial surgery. Retinal re-attachment was achieved using pars plana vitrectomy and gas injection with a final visual acuity of 20/200.
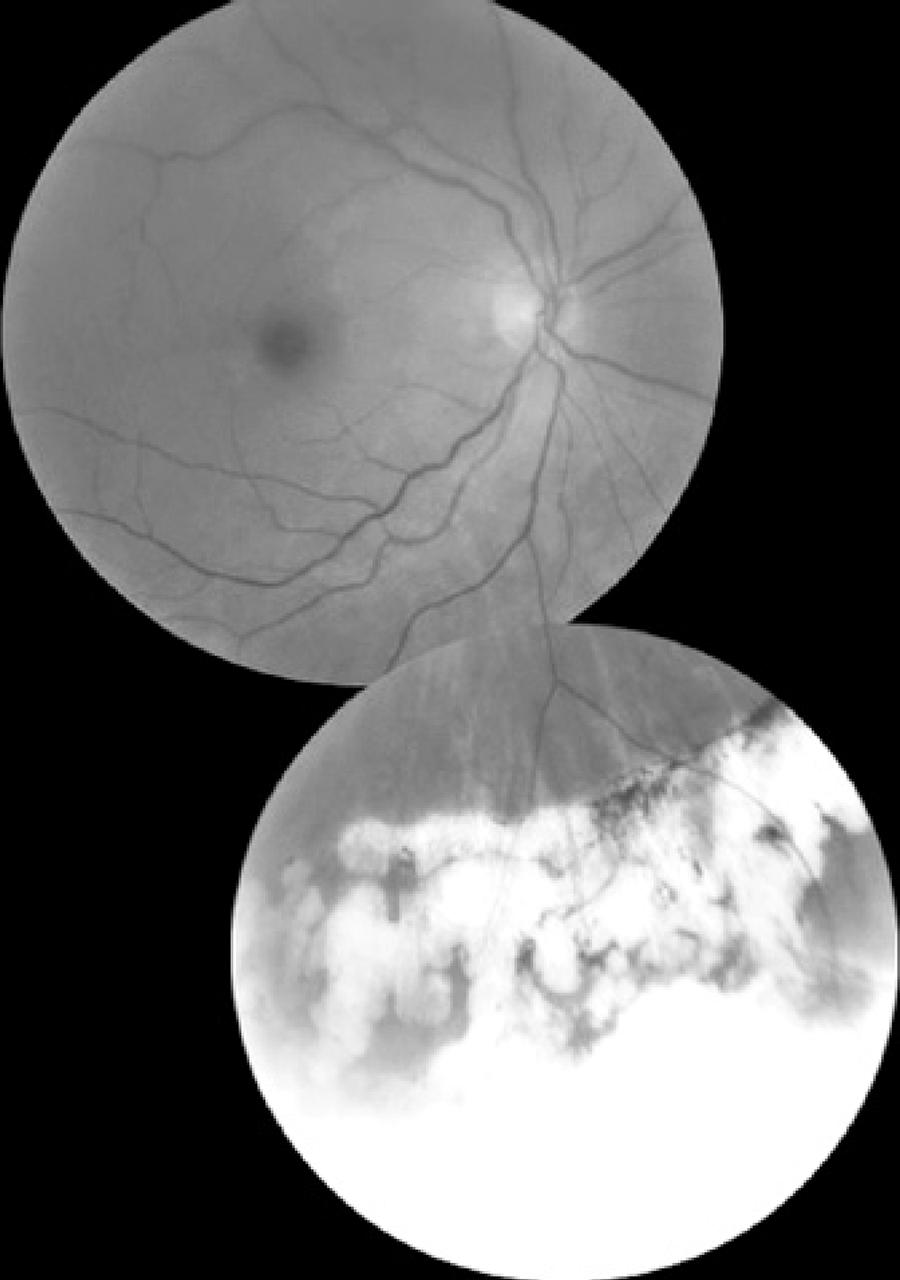
Figure 4 Postoperative melanoma resected en bloc; the whitish area corresponds to the scleral flap delimited by photocoagulation marks in the eye with VA of 20/20. This eye corresponds to the postoperative phase shown in figure 1.
The affected eye of the fifth patient was enucleated two years after the procedure because of blindness and pain due to retinal detachment secondary to vitreoretinal proliferation (VRP). This eye had the largest tumor (mixed cell-type melanoma) with a diameter of 15 mm, and this tumor was located in a posterior area of the eye. Moreover, this eye had the highest bleeding during surgery. This patient was operated two more times, with the placement of silicone oil for retinal re-attachment, but the procedure was unsuccessful. Table 1 summarizes all the observed results.
Table 1 Distribution of patients undergoing en bloc tumor resection, according to age, gender, tumor type, larger tumor diameter, location, and visual acuity (VA) during the pre-and post-operative phases and follow-up
| Age*/gender | Tumor type | Larger diameter | Location | Preoperative VA | Postoperative VA | FU (years) |
|---|---|---|---|---|---|---|
| 61/F | Spindle B melanoma | 10 mm | Choroid and ciliary body | 20/30 | 20/20 | 13 |
| 46/F | Medulloepithelioma | 10 mm | Choroid and ciliary body | 20/20 | 20/20 | 6 |
| 31/F | Leiomyoma | 8 mm | Choroid and ciliary body | 20/30 | 20/20 | 23 |
| 56/F | Spindle B melanoma | 12 mm | Choroid | 20/20 | 20/200 | 15 |
| 57/M | Mixed cell melanoma | 15 mm | Choroid | 20/40 | Enucleated | 11 |
*= age in years;
VA= visual acuity; F= female; M= male; FU= follow-up.
Tumors with a more anterior location achieved the best surgical results. No cases of metastatic disease or local recurrence of the tumor were observed during follow-up.
DISCUSSION
The cases reported herein indicate that it is possible to resect uveal tumors while retaining the eye and achieving good surgical results. We observed that four out of the five eyes were maintained and that in three eyes, the final vision was 20/20. These results were similar to those of Char et al.( 8 ), wherein the eye retention rate was 76%, and the final VA was 20/40 or better in 53% of the cases.
Scleral delamination using safety margins of 2-3 mm proved to be effective during tumor resection considering that tumor cells were not observed in the margins of the resected specimen in any case. For tumors involving the choroid and ciliary body, scleral delamination was chosen, starting at the posterior boundaries of the tumor and advancing to the anterior region in order to maintain the integrity of the sclerotic-corneal limbus. With regard to posterior tumors involving only the choroid, delamination was started in the anterior region and advanced posteriorly so that more posterior regions of the eye could be reached. Pars plana vitrectomy was performed to avoid potential complications due to retinal bleeding and vitreous traction.
In tumors with a more posterior location, the rate of local complications, including bleeding and retinal detachment, was higher. The greater intensity of preoperative bleeding in these cases occurred probably because posterior tumors involve larger-caliber uveal vessels.
During the extensive follow-up (6-23 years), no signs of metastases were observed. In a larger study conducted by Damato et al.( 4 )involving 332 eyes subjected to trans-scleral resection, the metastasis rate was 16%. Both Char et al.( 8 ) and Damato et al.( 4 ) showed that the metastasis rate was not worse in patients who had undergone this type of surgery as compared with patients treated with radiotherapy or enucleation. Conversely, Chang and McCannel( 9 ) showed that radiotherapy - using brachytherapy or beam radiation - is the method with fewer complications for treating these tumors.
None of the five patients had tumor recurrence in the operated eye. However, Char( 8 ) highlights the risk of recurrence even in the cases in which the resected specimen was histologically described as having tumor-free margins. Therefore, periodic examinations should be performed during follow-up with the aim of early detection of possible recurrences.
Our results indicate that the surgical en bloc resection of uveal tumors is effective for the maintenance of the eye and vision, and the metastasis rate associated with it is comparable to those of other treatments, making it a viable alternative for the treatment of selected cases.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

