INTRODUCTION
Pathological myopia is associated with several vision-threatening complications. The term usually refers to eyes with a large axial length (typically over 26.50 mm) and a spherical equivalent (SphE) of at least -6.0 D( 1 ). Ocular pathology in high myopia is usually caused by excessive elongation of the eyeball, which can cause changes in the fundus such as macular atrophy, tessellated fundus, diffuse atrophy, lacquer cracks, patchy atrophy, choroid neovascularization (CNV), posterior staphyloma, straightened or stretched vessels, temporal peripapillary atrophic crescent, hemorrhages, or tilting of the optic disk( 2 ).
Myopic foveoschisis (MF) is a condition commonly seen in highly myopic eyes, affecting 9 to 20% of eyes with posterior staphyloma. Its pathogenesis is not fully understood yet( 3 ). Previous studies attribute the genesis of MF to tangential traction forces on a thin retina by an epimacular structure such as a vitreous band, a vitreoschisis or an epiretinal membrane (ERM), associated with the elongation of the ocular axis and a weak attachment between the neurosensory retina and the retinal pigment epithelium in the posterior staphyloma area( 3 ). MF may itself cause visual loss or predispose to macular hole formation and retinal detachment( 4 ).
MF is diagnosed by optical coherence tomography (OCT), which can show an intraretinal cleavage( 3 ). Many studies suggest that vitrectomy is associated with removal of epiretinal traction and is an effective treatment for MF( 5 , 6 ).
We present a case of a patient with recurrent myopic foveoschisis. The definitive treatment was vitrectomy and internal limiting membrane peeling.
CASE REPORT
A 66 year-old male, with a history of high myopia, pseudophakic in both eyes, complained of decreased vision in his right eye. The axial length of the right eye was 32.01 mm; its visual acuity was 20/70. Fundus examination and optical coherence tomography (OCT) (Figure 1) showed a mild ERM and splitting of the retinal layers. Pars plana vitrectomy was performed with intravitreous triamcinolone injection, posterior hyaloid and ERM peeling and 12% perfluoropropane (C3F8) gas tamponade. Two months after surgery, his best corrected visual acuity was 20/20, and the schisis had resolved (Figure 2).
Figure 1 OCT of the right eye shows mild epiretinal membrane and splitting of the retinal layers before the first vitrectomy was performed.
Figure 2 OCT of the right eye shows resolution of myopic foveoschisis after vitrectomy and epiretinal membrane peeling, as well as retinal atrophy.
After remaining asymptomatic for 17 months, the patient reported a new episode of sudden decreased visual acuity in his right eye. At that time, his best corrected visual acuity dropped to 20/60, and the OCT exam showed recurrence of the MF (Figure 3 A and B). He underwent vitrectomy and internal limiting membrane (ILM) peeling using brilliant blue to increase visualization, and gas tam ponade using 12% perfluoropropane. After six months, the patient’s best corrected visual acuity improved to 20/25. The OCT showed a remarkable improvement on macular anatomy. Residual traction was observed along the inferotemporal arcade, which was attributed to the vessel stiffness itself. The residual traction did not jeopardize the foveal region (Figure 4 A, B, C, D).
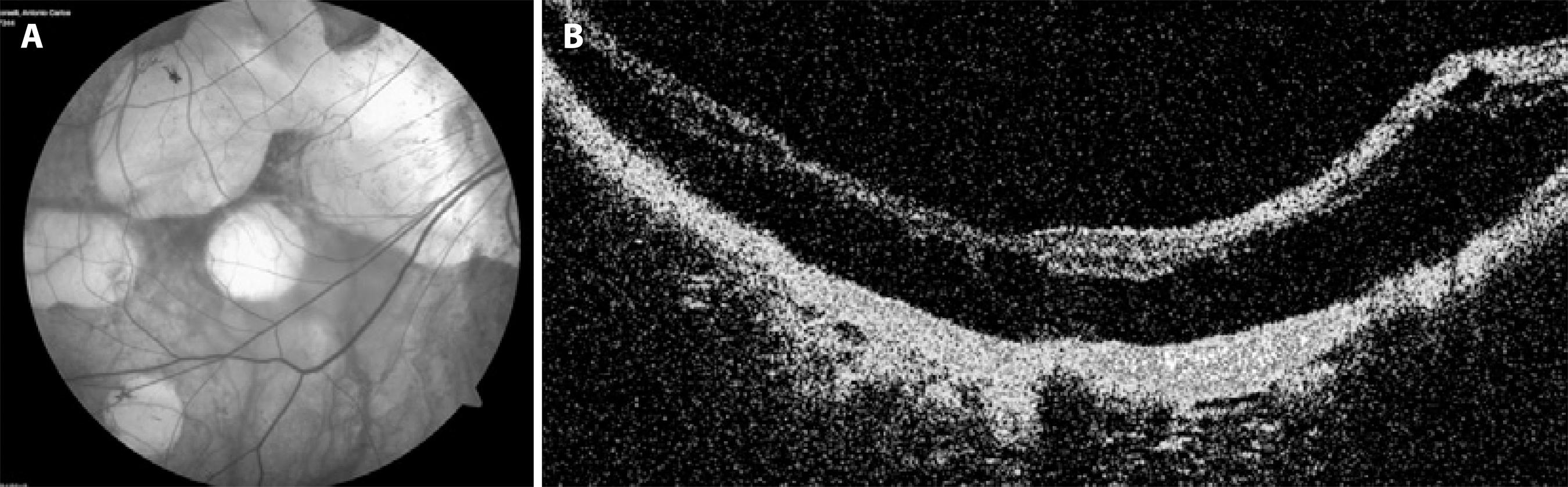
Figure 3 A) Retinography of the right eye shows recurrence of the schisis 17 months after the first vitrectomy. Fundus biomicroscopy reveals retinal thickening along the inferotemporal arcade. B) OCT of the right eye shows recurrence of myopic foveoschisis.
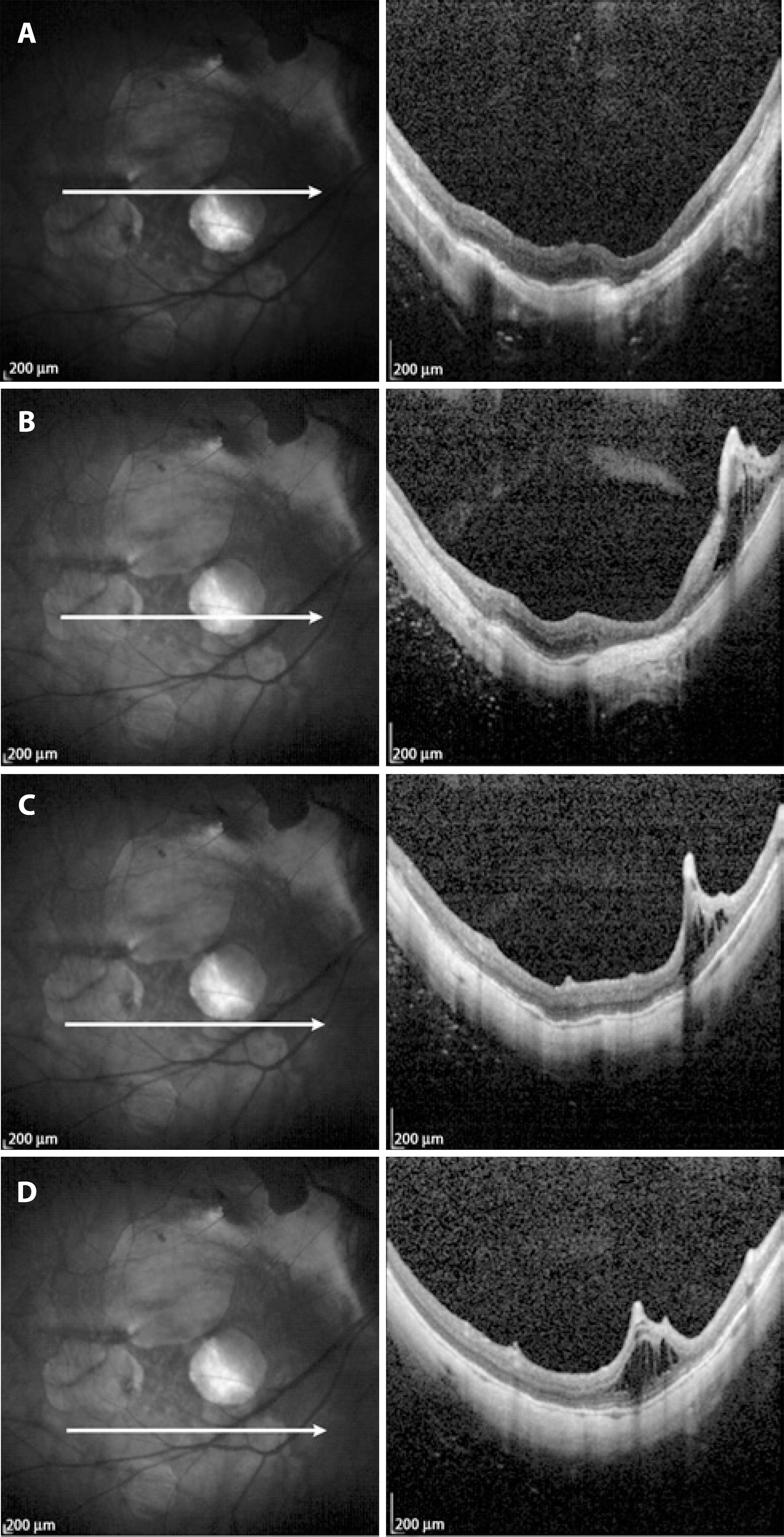
Figure 4 A) OCT after the second vitrectomy with ILM peeling shows resolution of MF. B) OCT shows residual intraretinal traction over the inferotemporal arcade despite ILM peeling. As the center of the macula was not jeopardized, the patient was just observed. C) OCT with intraretinal traction over the inferotemporal arcade. D) OCT showing intraretinal traction over the inferotemporal arcade.
DISCUSSION
Several mechanisms have been implied in the pathogenesis of myopic traction maculopathy, but the exact cause for this traction remains unclear. This term describes pathological alterations associated with highly myopic eyes, such as foveal detachment, macular hole, and macular retinoschisis. It is accepted that anteroposterior and tangential forces that stretch the posterior vitreous in the macular area in a predisposed eye are related to this condition( 5 ).
Many preretinal structures have been proposed as possible sources of traction, including ERM and a partially detached vitreous with vitreomacular adhesion( 4 ). However, some authors believe that myopic traction maculopathy is caused mainly by traction forces and tautness involving the inner retina overlying a posterior staphyloma( 7 ). A relative noncompliance or tightness associated to the inflexibility of the ILM and a possible inner retinal traction from retinal blood vessels could lead to a tangential traction( 8 ).
There is no consensus regarding the surgical management of myopic foveoschisis. Some studies have shown visual improvement after vitrectomy, and the need of ILM removal remains questionable. The probability of a successful repair increases when the major traction forces that act over the macula area are identified and relieved( 7 ).
Kim et al.( 9 ) performed vitrectomy with IML peeling to treat MF in 17 eyes, with or without gas tamponade. The study showed neither significant difference in postoperative best corrected visual acuity (BCVA) nor anatomic success between the no-gas group and the gas-treated group. However, foveoschisis resolved faster in the gas-treated group.
ILM removal in eyes with MF is challenging because of the long axial axis and poor contrast between retinal structures in those eyes. As in our case, previous studies show resolution of MF without ILM peeling( 10 ). However, in our patient a new episode of MF occurred in the same eye after 17 months. This time, ILM peeling was performed with gas tamponade. In both cases, surgery was done a few days after symptoms developed, which may explain the good final visual outcome.
Sayanagi et al.( 6 ) reported two cases of successful reoperation for persistent myopic foveoschisis, after primary surgery without ILM peeling. Although the reoperation included the ILM peeling, in both cases the MF remained unresolved after the first surgery. In contrast, retinal MF in our patient was successfully managed after the first vitrectomy.
Even if the myopic foveoschisis is fully resolved and all tangential traction in the eye is removed, OCT shows an important area of residual intraretinal traction over the inferotemporal arcade. This traction may be attributed to the vessel stiffness itself. Ikuno et al.( 8 ) showed that in eyes with MF subjected to vitrectomy with ILM peeling, the retinal arteriole may cause an inward traction force in the retina. This traction seems to be caused by insufficient flexibility of the sclerotic retinal arteriole during axial length elongation in highly myopic eyes, and may contribute to the genesis of MF.
The residual traction caused by the arcade stiffness did not affect the fovea in our case. If it threatens the fovea, and if all the tangential traction in the eye has already been removed, one could consider other surgical techniques, such as a macular buckle or a scleral shortening.
In conclusion, this is the first case in the literature describing a late recurrence of foveoschisis after initial complete resolution. The late recurrence was successfully treated with ILM peeling, with resolution of MF for over a year of follow-up. Removing the ILM is a challenging maneuver in eyes with MF, even with the use of staining techniques. Myopic foveoschisis may be resolved without peeling the ILM, but its removal should be considered if the condition recurs.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

