INTRODUCTION
Myelomeningocele, a type of spina bifida, is a developmental defect in the vertebral arches of the spine. It is caused by incomplete closure of the neural tube resulting from inadequate proliferation of ectodermal cells during the fourth week of embryogenesis( 1 , 2 ). This condition may involve areas from the neck to the sacrum and is associated with severe neurological defects, such as flaccid paraplegia and sensory changes below the lesion and hydrocephalus, as well as urologic and orthopedic conditions, which can increase significantly the morbidity and mortality of the disease. It is one of the most common birth defects, occurring in approximately 1 per 1000 live births. The etiology is variable and may involve genetic and environmental factors such as folic acid deficiency during neurulation( 2 - 4 ).
The importance of involving ophthalmologists in the care of children with myelomeningocele has only recently become evident. Ocular changes, particularly strabismus and amblyopia, are very common in these patients( 5 ). The few published articles on this topic show a frequency of strabismus ranging from 52% to 61% in this group, especially in patients with associated hydrocephalus. A-pattern anisotropia also has a higher incidence in this population( 5 , 6 ).
Because it is the most frequent neural tube defect( 7 ), understanding the neurological signs and the ophthalmologic conditions in patients with myelomeningocele is extremely important for appropriate multidisciplinary management. Although strabismus is commonly associated with myelomeningocele, the surgical outcomes of strabismus in these patients were not reported in any studies. Therefore, the purpose of this study was to find the indications for strabismus surgery in patients with myelomeningocele and to evaluate the results achieved with postoperative surgical correction.
METHODS
This study was performed at the Ophthalmology Orthoptics Section of the AACD (Associação de Assistência à Criança Deficiente). The project was approved by the Ethics Committee of the same institution (Approval number 374.105; date: 07/30/13). The principles of the Declaration of Helsinki were followed.
We retrospectively reviewed the records of all patients with myelomeningocele who underwent surgery for strabismus correction between January 2008 and January 2013.
The analysis of the records included (1) classification of myelomeningocele, (2) presence or absence of hydrocephalus and the need for a shunt, (3) ectoscopy, (4) presence or absence of anomalous head position, (5) visual acuity, (6) refraction under cycloplegia, (7) indirect ophthalmoscopy, (8) preoperative ocular motility testing, (9) type of strabismus surgery performed and (10) postoperative ocular motility testing.
For the visual acuity, teller cards in non-verbal and non-collaborative, Snellen optotypes ("E" chart, numbers or letters), or Light House were used. These acuities were transformed into log/MAR (log of the minimum angle resolution)( 8 ) and averaged. The resultant value was converted back into a Snellen notation, which produced the geometric mean.
The refraction under cycloplegia (30-40 min after the instillation of 1% cyclopentolate and 1% tropicamide) was also analyzed. Hyperopia was defined as spherical equivalent refractive errors ≥2.00 D, astigmatism as cylinder refractive errors ≥0.75 D, and myopia as spherical equivalent refractive errors of -0.5 D or more( 9 , 10 ).
The ocular alignment before and after surgery was obtained by the use of cover-uncover and alternate prism-cover testing in the primary position (fixation at a distance of 6 m and 33 cm) and in the cardinal gaze positions. In patients with poor visual acuity, the corneal light reflex combined with prisms was used to access ocular alignment. Ocular ductions were measured using a 4-point scale.
The surgical results were graded as excellent when the patients presented with a postoperative horizontal deviation of ≤10 prism diopters (PD), and there was a correction of the alphabetic pattern to ≤10 PD for an A-pattern and ≤15 PD for a V-pattern. The results were considered satisfactory when the postoperative horizontal deviation ranged between 11 and 19 PD in primary position. When there were deviations ≥20 PD and a residual alphabetic pattern of >10 PD for an A-pattern and >15 PD for a V-pattern, the results were considered unsatisfactory.
Pre- and postoperative measurements were calculated and presented as mean (standard deviation), and compared with the Wilcoxon signed rank test. P-values <0.05 were considered statistically significant. All analyses were done using Stata v.11 (College Station, Texas, USA).
RESULTS
We identified forty-four patients with myelomeningocele who underwent strabismus surgery between January 2008 and January 2013 at AACD, São Paulo. We excluded three records because of incomplete charts. Three authors (MFC, MKUT, and NTK) performed the surgeries of the remaining 41 patients (20 males). The age of the patients at the time of the procedure ranged from 23 months to 17 years (mean, 7.89 years).
The thoracic level myelomeningocele was the most frequent type (43.9%) found in the study. The second most frequent type was the lumbar level lesion (34.1%); in this group, the high-lumbar level was more evident (64.3%). Other types observed were the asymmetric (19.5%) and occipital (2.5%) myelomeningoceles.
Hydrocephalus was present in 38 patients (92.7%), of which only one did not require a shunt.
The mean corrected visual acuity was 0.18 logMAR (SD 0,22). Best corrected visual acuity was 20/40 or better (Snellen) in 62 eyes (75.6%) and worse than 20/40 (Snellen) in 20 eyes (24.4%).
The most frequent refractive error was astigmatism, found in 32 eyes (34.4% hyperopic, 34.4% mixed and 31.2% myopic astigmatism). Hyperopia was found in 14 eyes (17.07%), myopia in 12 eyes (14.63%), and 37 eyes (45.12%) were emmetropes.
Fundoscopy revealed bilateral optic disc pallor in 5 patients (12.2%) who all had a previously shunted myelomeningocele.
Nystagmus was observed in 16 patients, of which 9 (56.25%) had anomalous head positions to neutralize the eye movements.
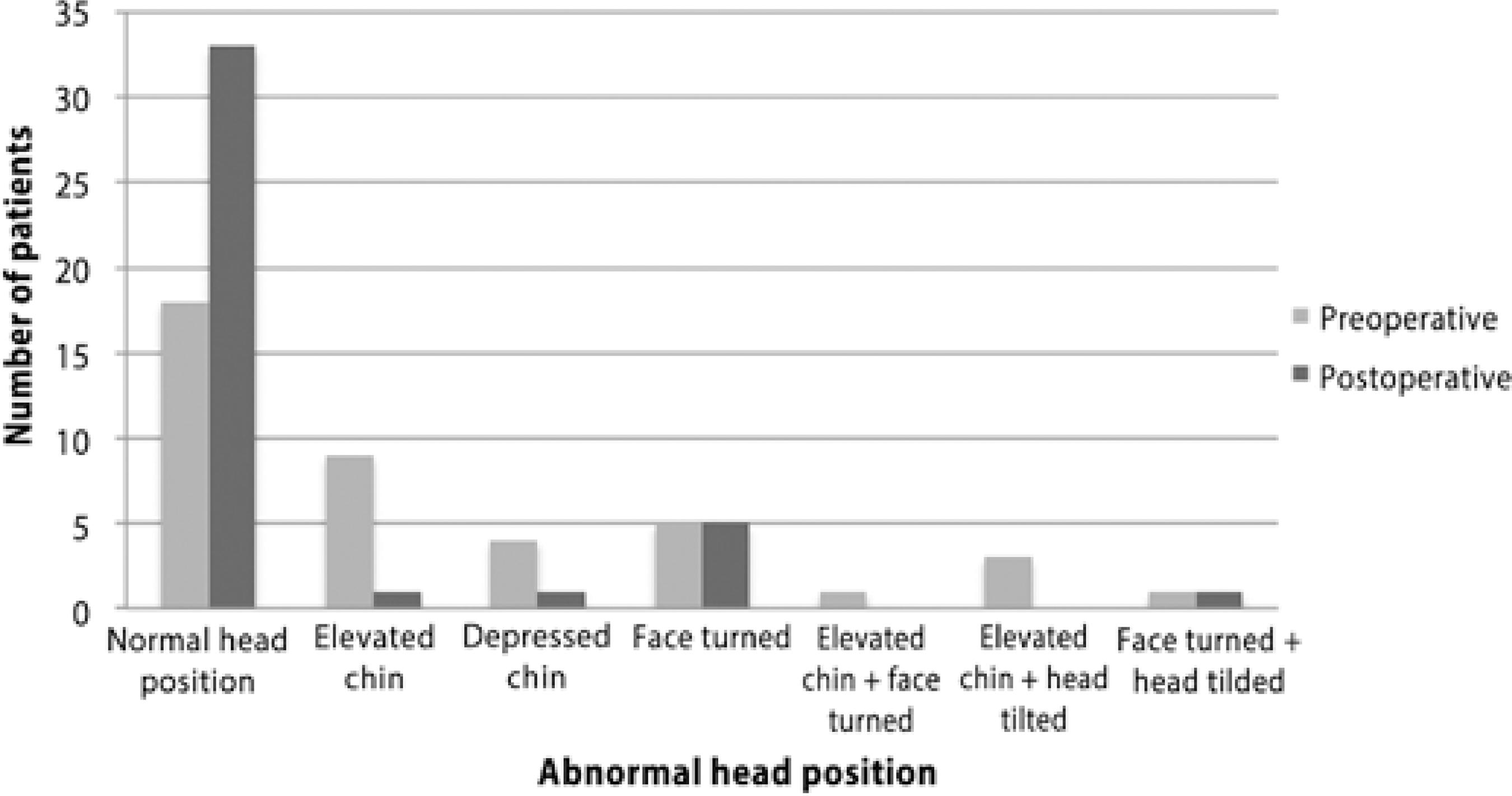
Before surgery, 56.1% of the patients had anomalous head positions (Figure 1). The main cause of an abnormal head turn was strabismus in 60.9% of the patients. From these patients with strabismus and anomalous head turn, 21.4% were due to crossed fixation (esotropia) and 78.6% were due to anisotropia with alphabetic pattern.
Nystagmus caused abnormal head turn in 34.8% of the patients; nystagmus was associated with strabismus in 4.3% of the patients.
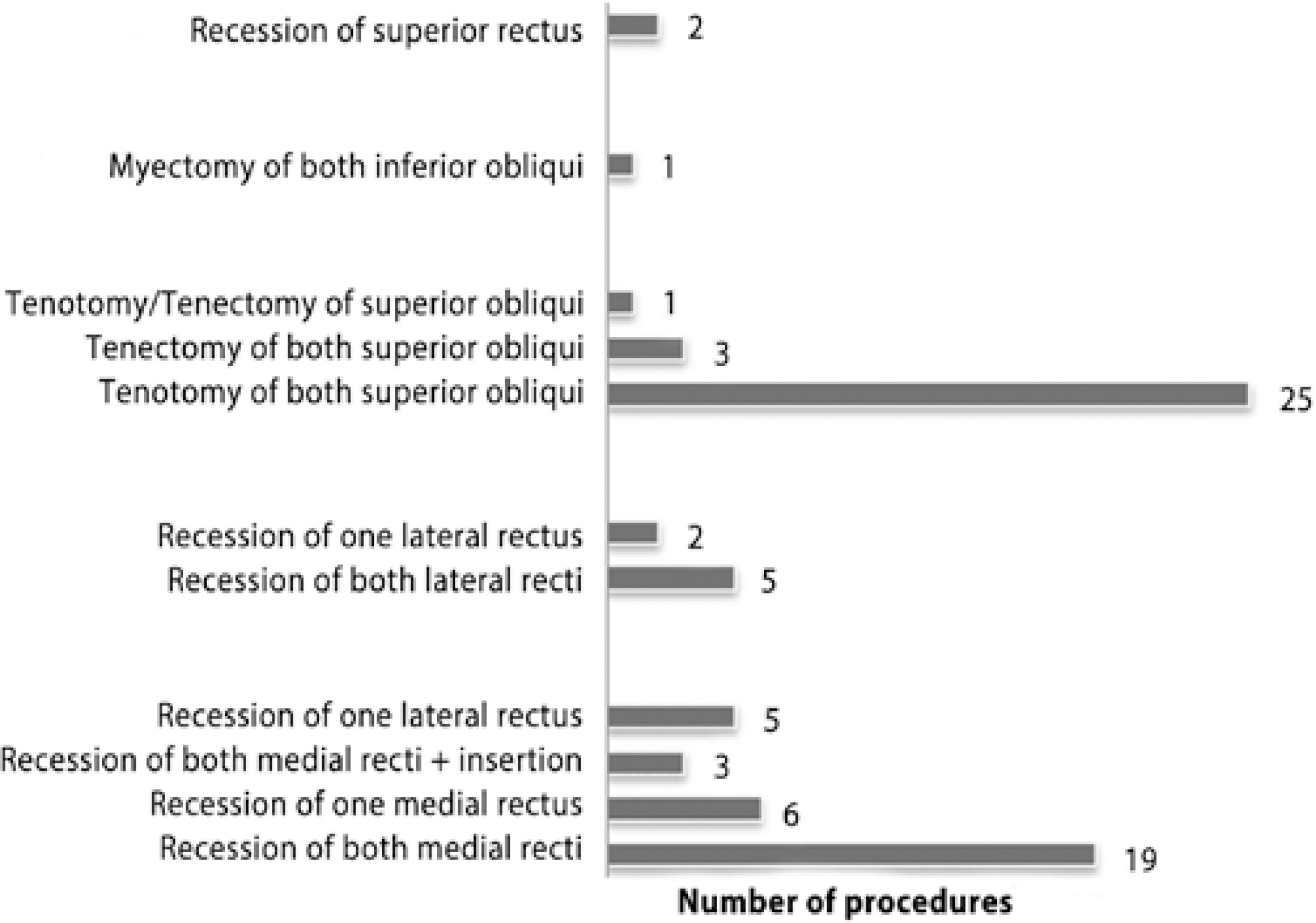
The main strabismus profiles observed were esotropia (ET), present in 31 patients (mean deviation 32.4 PD, SD 13.15), and A-pattern anisotropia in 34 patients (mean deviation 23.8 PD, SD 13.9). Exotropia (XT) was observed in eight patients preoperatively (mean deviation 33.75 PD, SD 22.16) and vertical deviations in two patients. Of the surgeries performed, 82.9% required correction of A-pattern anisotropia exceeding 10 PD. Two patients required two strabismus surgeries during the study period. Superior oblique overaction was observed in 37 patients and inferior oblique underaction in 24.
Table 1 and figure 2 show pre-and postoperative characteristics and surgeries performed. The average postoperative evaluation time was 28.9 months (range 0.5-70 months).
Table 1 Pre-and Postoperative characteristics
| Alignment | Preoperative (%) | Postoperative (%) |
|---|---|---|
| Deviation ≤10 PD in primary gaze | 0% | 60.9% |
| Esotropia | 75.60% | 26.8% |
| Exotropia | 19.50% | 9.7% |
| Vertical deviation | 4.88% | 0% |
| A pattern anisotropia | 82.90% | 12.2% |
| V pattern anisotropia | 2.40% | 2.4% |
| No alphabetic pattern | 14.60% | 85.4% |
The surgical results were excellent in 60.9% patients, satisfactory in 12.2%, and unsatisfactory in 26.9%. Eleven patients were orthotropic after surgery. The mean esotropia was 11.25 PD (SD 6.1), and exotropia was 18 PD (SD 15). A-pattern anisotropia was still present in 5 patients (mean deviation 15.2 PD, SD 5.6). V-pattern was observed in only one patient postoperatively (15 PD).
In patients who were previously ET, pre-and postoperative differences were statistically significant (p=0.0001). A clinically significant A-pattern was present in 5 patients after surgery (p<0.001). Although the V-pattern and XT correction were clinically satisfactory postoperatively, they were not statistically significant when compared with the preoperative deviations (p=0.3248 and p=0.4565, respectively).
There was an anomalous inferior insertion of the medial rectus in 5 patients, and of the lateral rectus in 2 patients.
DISCUSSION
This study provides the first data on strabismus surgical outcomes in patients with myelomeningocele. We found a large number of patients with esotropia and A-pattern anisotropia in this group.
The distribution of the medullar lesion level in those patients that required strabismus surgery was very similar to what was found in a previous study involving all patients with myelomeningocele at AACD( 3 ). In that study, the thoracic level was the most common lesion site, followed by the lumbar level. In addition, the prevalence of shunted hydrocephalus in the patients in our study was similar to the prevalence in patients with spina bifida in general (97.4% versus 95.2%).
A visual acuity of 20/40 or better (Snellen) was observed in 75.6% of the patients in our study. This is reasonably better than the acuities Cronemberger et al. found in patients with spina bifida at the same institution (53%)( 6 ) and the acuities found by Andersson et al. in patients with hydrocephalus (VA between 20/40 and 20/125 in 34% of the patients)( 11 ).
The most frequent refractive error observed was astigmatism, followed by hyperopia and myopia. This differs slightly from results reported by others( 6 , 11 ). In our patients, emmetropia predominated, and we found a higher prevalence of astigmatism and a lower frequency of hyperopia. Nevertheless, refractive error was not found to be an important cause of deviation in patients with spina bifida. Some authors have suggested that the strabismus in these patients has a paralytic etiology( 12 ).
Fundoscopy showed bilateral optic disc pallor in 5 patients (12.2%), similar to what was observed by Cronemberger et al.( 6 ) (12.5%) and Altinta et al. (8%)( 13 ). Several years ago, it was postulated that optic atrophy in these patients might be due to "stretching of the optic nerves" and by pressure exerted on them that led to compromised local blood supply( 12 ).
Nystagmus was another frequent condition in our patients (56.1% before surgery). Andersson et al. also detected a similar prevalence of nystagmus in patients with hydrocephalus( 11 ). In 1965, Goddart studied the ocular changes in patients with hydrocephalus, most of whom had spina bifida She also observed this condition in her group and suggested that it could be attributed to a "central lesion in the pathways responsible for maintenance of ocular position"( 14 ).
Abnormal head posture is not an unusual sign in pediatric populations, especially in those with myelomeningocele, and may involve not only extraocular muscle disorders but also skeletal, muscular, neurologic, otolaryngologic, and some eye disorders. The incidence is 5.6% in ophthalmological practice and 3.2% in pediatric ophthalmological practice( 15 ). The abnormal head postures are adopted to improve visual acuity, maintain binocular single vision, center residual visual field with the body, or even for cosmetic reasons. Face turn is the most frequent abnormal head posture in children; its most frequent ocular causes are congenital nystagmus, superior oblique paresis, dissociated vertical deviation, Brown syndrome, and refractive errors. Chin-up or chin-down postures are most commonly caused by A- and V-pattern strabismus, palpebral ptosis, nystagmus, and refractive errors( 16 , 17 ).
Abnormal head position was present in 56.1% patients in this study. We did not consider it an isolated indication of surgery, but it was present in many patients, predominantly to compensate A-pattern anisotropia and nystagmus. It definitely had an influence on the indication of surgical correction. Previous studies did not include this variable in their analyses. This condition improved considerably after strabismus surgery.
In cases of abnormal head compensation of nystagmus, many authors suggested that simply tenotomizing the horizontal recti may improve the condition, even if the muscles are reattached in their original insertions. This would happen due to the afferent proprioceptive loop, producing a damped peripheral oculomotor response to the small nystagmus signal( 18 ). Therefore, in our study we could assume that in patients with abnormal head turn due to nystagmus, the strabismus surgery itself may have had some impact on the nystagmus and, subsequently, on the head turn.
The type of strabismus encountered was very similar to what several other authors found before( 6 , 11 , 14 , 19 ). It is evident that the frequency of esotropia and A-pattern anisotropia is high in patients with myelomeningocele.
No case of third or sixth cranial nerve palsy was observed, although these conditions may occur in a higher incidence in patients with hydrocephalus.
The surgeons determined that the horizontal rectus muscles had a particularly inferior insertion in 7 patients. Although not reported before, this alteration may contribute to the anisotropias.
The presence of A-pattern in patients with hydrocephalus may also be explained by the enlargement of the head with frontal bossing. This can cause an anterior displacement of the trochlea, and thus a reverse relationship as described for plagiocephaly between the planes of the superior oblique tendon, the inferior oblique muscles, and the optic axis. The superior oblique muscles become more effective as depressors, and increased abduction in downward gaze causes the A-pattern often seen in patients with hydrocephalus( 20 ).
The authors adopted a different surgical result graduation in this study. These kind of patients are seldom re-operated in case of residual deviations in primary position <20 PD, or residual alphabetic patterns of <10 PD (A-pattern) and <15 PD (V-pattern). This particularity is not only for the systemic condition of these patients, but also because we assume the functional result within these values was good.
Excellent and satisfactory postoperative results were achieved in 73.1% of the patients. This is in accordance with non-adjustable strabismus surgeries in general, where the reoperation rate due to unsuccessful results is >20%( 21 ). In addition, the correction of A-pattern was satisfactory.
In conclusion, the main indications for strabismus surgery in patients with myelomeningocele were esotropia and A-pattern anisotropia. Strabismus surgery in this population had an elevated percentage of excellent and satisfactory results, not only for the ocular deviation, but also for improvement of abnormal head posture.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

