INTRODUCTION
Recurrence is the most common complication of pterygium surgery and a cause of patient discontent; these are primary challenges for this surgery( 1 ). Many approaches, including beta therapy, antimetabolic agents, and subconjunctival bevacizumab, have been proposed to prevent recurrence. However, these treatments are often associated with complications( 2 - 6 ).
Tranilast inhibits the growth of pterygium-derived cells( 7 ); therefore, its use may reduce the recurrence of pterygium. Tranilast, N-[3,4-dimethoxycinnamonyl]-anthranilic acid, is an antiallergy drug that was first used to prevent bronchial asthma and allergic rhinitis. Recent studies have shown that tranilast has an antifibrotic effect, inhibiting the proliferation of fibroblasts and their subsequent transformation into myofibroblasts( 8 ). Furthermore, tranilast has been associated with decreases in posterior capsule opacification after cataract surgery and inhibition of scaring after glaucoma filtering surgery( 9 , 10 ).
The present study aimed to determine the efficacy of tranilast for preventing pterygium recurrence. In addition, this study aimed to evaluate the symptoms and presence of transforming growth factor-β (TGF-β) in excised tissues when 0.5% tranilast was administered via subconjunctival injection prior to surgery as adjunctive therapy in conjunctival autograft (CAU) for cases of primary pterygium.
METHODS
This prospective, randomized control trial included 50 patients who underwent primary pterygium treatment at the Hospital de Base (HB) of the Medical School in São José do Rio Preto between June and December 2010.
The inclusion criteria were pterygium with a horizontal length of >2 mm measured from the anatomic limbus and subjective eye symptoms (irritation, burning, excessive tearing, dry eye sensation, foreign body sensation, and hyperemia). The exclusion criteria were a lack of connective tissue, history of eye trauma, glaucoma, dysfunctional tear syndrome, rosacea, neurotrophic keratopathy, systemic or topical use of immunosuppressive drugs, age <18 years, and vulnerability related to physical or mental illness.
Pterygium was categorized according to the classification described by Tan et al.( 11 ). Patients were randomly allocated into 2 equal groups that included a Control Group (CG) treated with CAU employing fibrin glue (Tissucol®; Baxter AG, US) and a Tranilast Group (TG) treated with a 0.1-mL subconjunctival injection of tranilast solution (1.0 mg/mL). The subconjunctival injection was placed in the head of the pterygium as adjunctive therapy 30 days before CAU employing fibrin sealant (Tissucol®; Baxter AG). Tobramycin eye drops (0.3%, Tobrex®; Alcon Laboratories, Fort Worth, TX, USA) were administered 4 times daily for 3 days after the injection. Randomization was performed by means of a table of random numbers.
single surgeon (GCAJ) who was masked to the patients' group assignments performed all the surgeries. Surgical procedures were performed in an operating room using an ophthalmic microscope after instillation of 1.0% tetracaine chlorhydrate (every 5 min over 30 min and in the perioperative period if necessary). CAU was performed following the technique of Koranyi et al.( 12 ) with some modifications to cover the bare regions of the sclera. Mitomycin C (0.1 mL of 0.02%) was injected postoperatively into the remaining conjunctiva above and below the site where CAU was placed and with extreme care to prevent wetting of the ocular surface. Tobramycin-dexamethasone ointment (TobraDex®; Alcon Laboratories) was applied, and the eye was occluded using a bandage, which the patient was instructed to remove the following morning. Tobramycin eye drops (0.3%, Tobrex®; Alcon Laboratories) were prescribed 4 times daily for 7 days and dexamethasone drops (0.1%, Maxidex®; Alcon Laboratories) were prescribed every 3 h during the first week and then 4 times daily for the following 3 weeks.
The excised pterygium was stored in liquid nitrogen. After all the patients had been treated, 7 samples from each group were randomly selected for analysis. Immunohistochemistry was performed in the surgical pathology service of the HB. The pterygium tissue samples were submitted to serial 6-μm thick sectioning with a cryostat at -20°C. Histological preparations were performed on slides covered with polylysine that was fixed in cold acetone for 15 min and washed with phosphate-buffered solution (PBS) 3 times for 5 min. The slides were then treated with 0.5 peroxidase (composition: 49.17 mL PBS, 49.17 mL methanol, and 16.5 mL H2O2) for 10 min to block endogenous peroxidase and were incubated in horse serum for 30 min at room temperature to prevent non-specific binding. TGFβ1/2 primary antibody (sc-80346; Santa Cruz Biotechnology, Santa Cruz, CA, USA) diluted at 1/20 in bovine albumin was used for about 12 h at 4°C. Thereafter, the slides were washed 3 times for 5 min in PBS. The slides were then incubated in a secondary antibody (biotinylated anti-mouse antibody; ABC Staining System, sc-2017; Santa Cruz Biotechnology) for 30 min and washed in PBS. The next step was to incubate with the ABC reagent for 30 min. Next, the slides were incubated in 0.05% 3', 5'-diaminobenzidine (Sigma-Aldrich Co LLC, St Louis, USA), contra-stained using Harris hematoxylin, and washed. The negative control comprised exposure to the secondary antibody and the ABC reagent, without exposure to the primary antibody. Pig gut was used for the positive control. An experienced pathologist (DDN) blinded to the group assignments evaluated the immunohistochemical slides using an optical microscope at 400' magnification in a field-oriented assessment of the epithelial region of the pterygium. Cells with either total or partial staining of the circumference of the epithelial cytoplasmic membrane were considered positive and those that remained unstained were considered negative. The results were based on 100 cells obtained from each sample.
Components of the tranilast solution were acquired from Cayman Chemicals (Catalog 13044; Ann Arbor, MI, USA) and manufactured by Ophthalmos (Sao Paulo, Brazil). The preparations were labeled (0.2 mL of 5 mg/mL tranilast) and stored at -20°C.
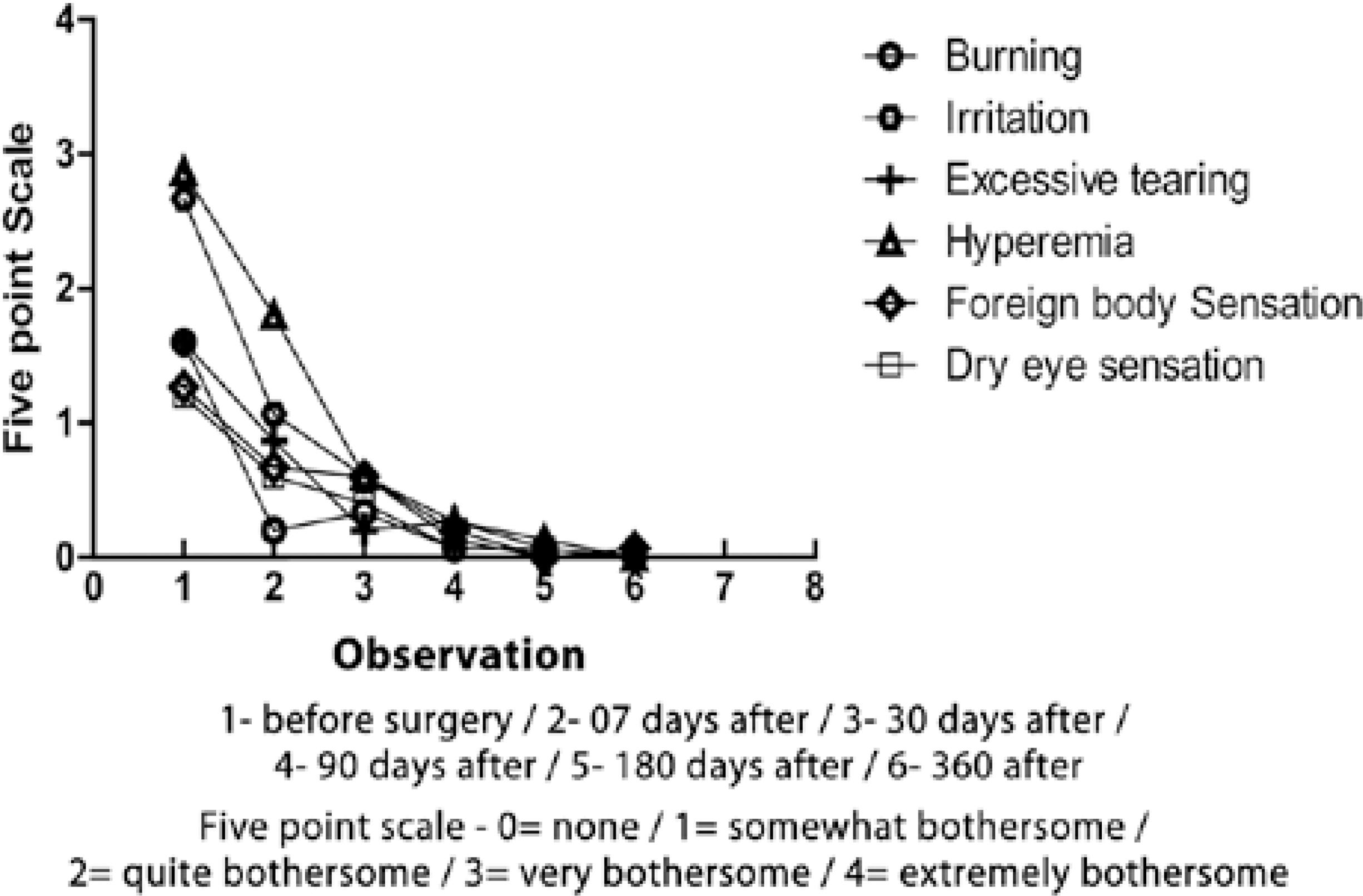
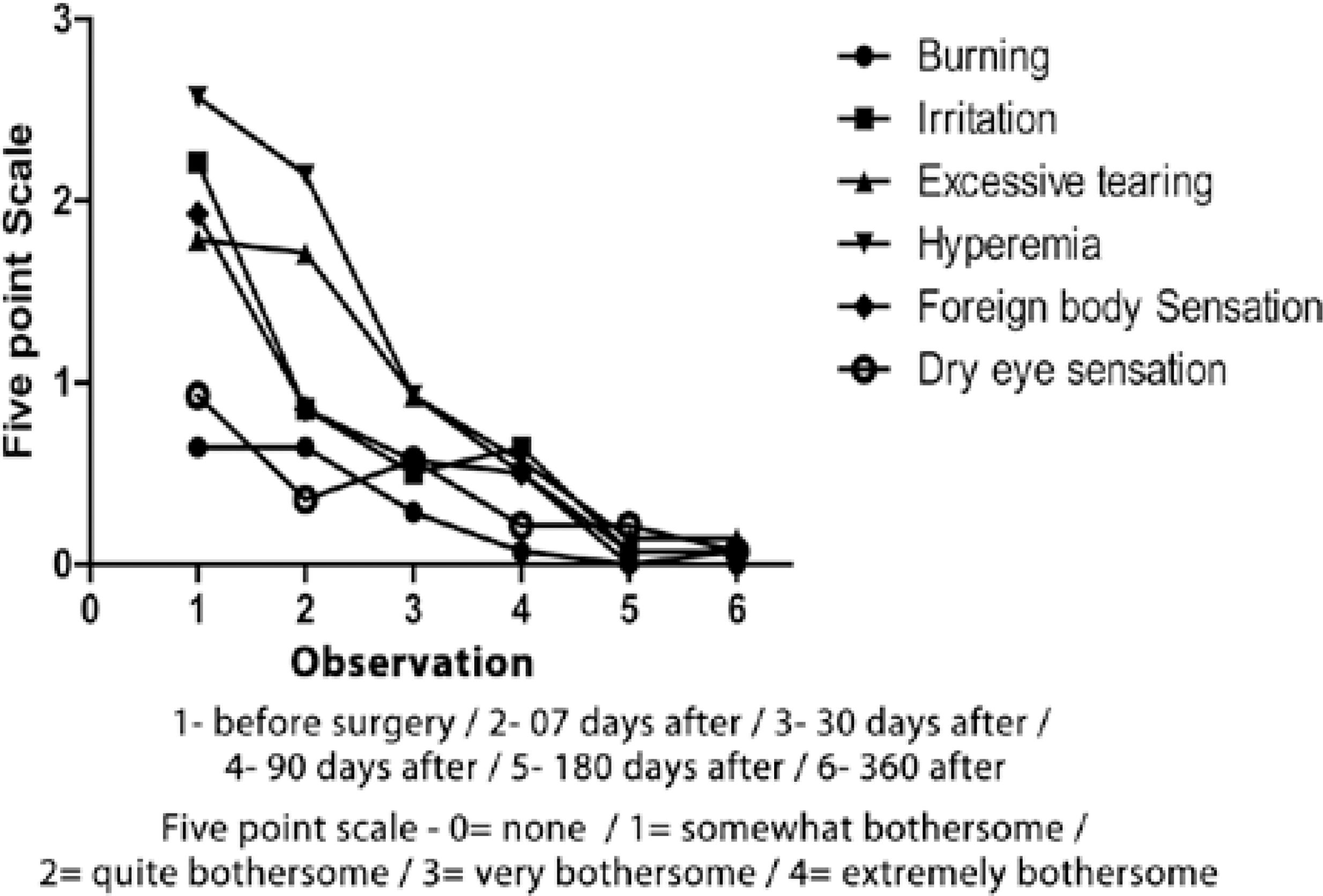
A graft was considered a success when it remained intact after surgery without recurrence. Recurrence was defined on the basis of the description provided by Sebban and Hirst( 13 ). Subjective symptoms of burning, irritation, excessive tearing, hyperemia, foreign body sensation, and dry eye sensation were assessed prior to surgery on the 7th postoperative day and during the 1st, 3rd, 6th, and 12th postoperative months. The symptoms were quantified using the following 5-point abnormal sensation scale adapted from Lim-Bon-Siong et al.( 14 ): 0) none; 1) somewhat bothersome but tolerated; 2) quite bothersome; 3) very bothersome; and 4) extremely bothersome. A non-medical professional who did not participate in the surgery conducted the interviews to avoid investigator bias. Another ophthalmologist (LA) performed the ophthalmic evaluations under a slit lamp over the 12 months of the study to assess the integrity of the graft, possible complications, and the recurrence rate.
Fischer's exact test was used to evaluate the recurrence rate at the end of the 12 month study. The Mann-Whitney U test was used to evaluate the positivity of epithelial cells with respect to TGF-β and to compare the symptoms between groups at each time interval. The Friedman test was used to analyze the symptoms evaluated within groups using the 5-point scale. Graph Pad Prism 5 (Graph Pad Software Inc., La Jolla, CA, USA) was used for statistical analysis and to build graphs. The significance level was set at 0.05.
All participants signed consent forms. The study protocol was approved by the Ethics Committee of FAMERP (#30492009) and was registered as a clinical trial with the U.S. National Institutes of Health (#NCT01003613). The authors certify that the protocol for the research project conformed to the provisions of the Declaration of Helsinki of 1995 (as revised in Edinburgh 2000) and declare no financial support or relationships that may pose a conflict of interest.
RESULTS
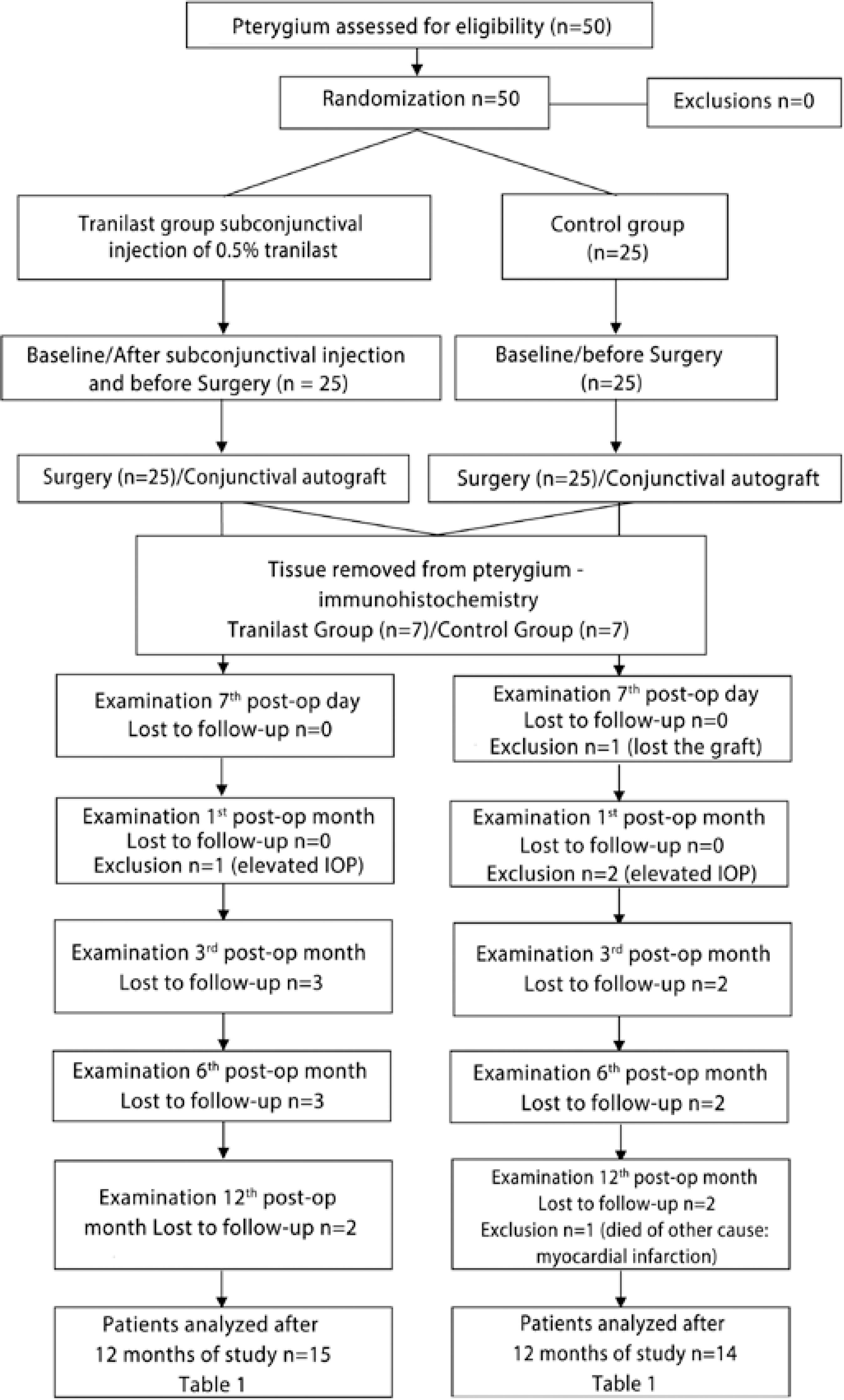
In total, 29 patients with primary pterygium were included in the study; 15 were assigned to TG and 14 were assigned to CG. A CONSORT-based diagram showing patient flow through each step of the trial is shown in figure 1.
The patients completed at least 12 months of follow-up. All pterygia were primary and located in the nasal region. As the data presented in table 1 indicate, both groups were similar at baseline in terms of gender, laterality, age, horizontal size, vertical size, pterygium classification, and length. All variables were statistically similar between the groups.
Table 1 Preoperative characteristics of the 2 groups of patients who completed the study
| Control group | Tranilast group | p-value | |
|---|---|---|---|
| n | 14 | 15 | |
| Gender (male/female) | 8/6 | 5/10 | |
| Laterality (right/Left) | 9:5 | 9:6 | |
| Age (years) | 46.43 ± 13.12 (38.85-54.01) | 44.73 ± 12.16 (38-51.47) | 0.74 |
| Horizontal length (mm) | 3.82 (3.14-4.49) | 3.30 (2.87-3.72) | 0.25 |
| Vertical length (mm) | 5.30 (4.5-6.09) | 4.80 (4.22-5.37) | 0.22 |
| Pterygium Tan Grading | |||
| T1 atrophic | 0 (0%) | 0 (0%) | |
| T2 intermediate | 3 (21.43%) | 2 (13.33%) | |
| T3 fleshy | 11 (78.57%) | 13 (86.67%) | |
| Time (months) | 12.71 (12.24-13.19) | 12.93 (12.49-13.38) | 0.45 |
Pterygium Tan Grading( 11 ): Grade 1 (atrophic) - episcleral vessels under the body of the pterygium are clearly observed; Grade 3 (trophic) - episcleral vessels under the body of the pterygium are entirely obscured; and Grade 2 (intermediate) - types of pterygium that do not fit into 1 of the 2 categories described above.
Some degree of edema that was present in each graft after surgery improved with time. One patient lost a graft during the study and was therefore excluded. Three patients who presented with elevated eye pressure were also excluded from the study. Thirteen patients were lost to follow-up, 3 evolved with granuloma that required extended treatment with corticosteroids, and 1 died of myocardial infarction. Thus, 21 patients were lost to follow-up and 29 patients completed the study.
Both groups used 0.1 mL mitomycin C (0.2 mg/mL) in the subtenonian region near the upper and lower conjunctive areas of the donor conjunctiva, and there were no complications during the first 12 months. Recurrence occurred in 2 CG patients and 1 TG patient after a year (p=0.59). The TG patient and 1 CG patient presented with small (0.5 mm) fibrovascular invasions in the limbal region. The other CG patient was diagnosed with conjunctival recurrence.
None of the patients presented with symblepharon. Both groups showed significant improvement in subjective symptoms at the end of the 12-month follow-up period, but there were no significant differences in the 6 subjective symptoms between the 2 groups (Figures 2 and 3).
The percentage of cells expressing TGF-β in TG (mean: 7.85%; range: 2.56-13.15%) was lower than that in CG (mean: 18.14%; range: 11.53-24.56%, p=0.01; Figure 4). Figure 5 shows how calculations for the expressed TGF-β cells were performed using images from a patient in CG. The esthetic results were very similar between the 2 groups (Figure 6).
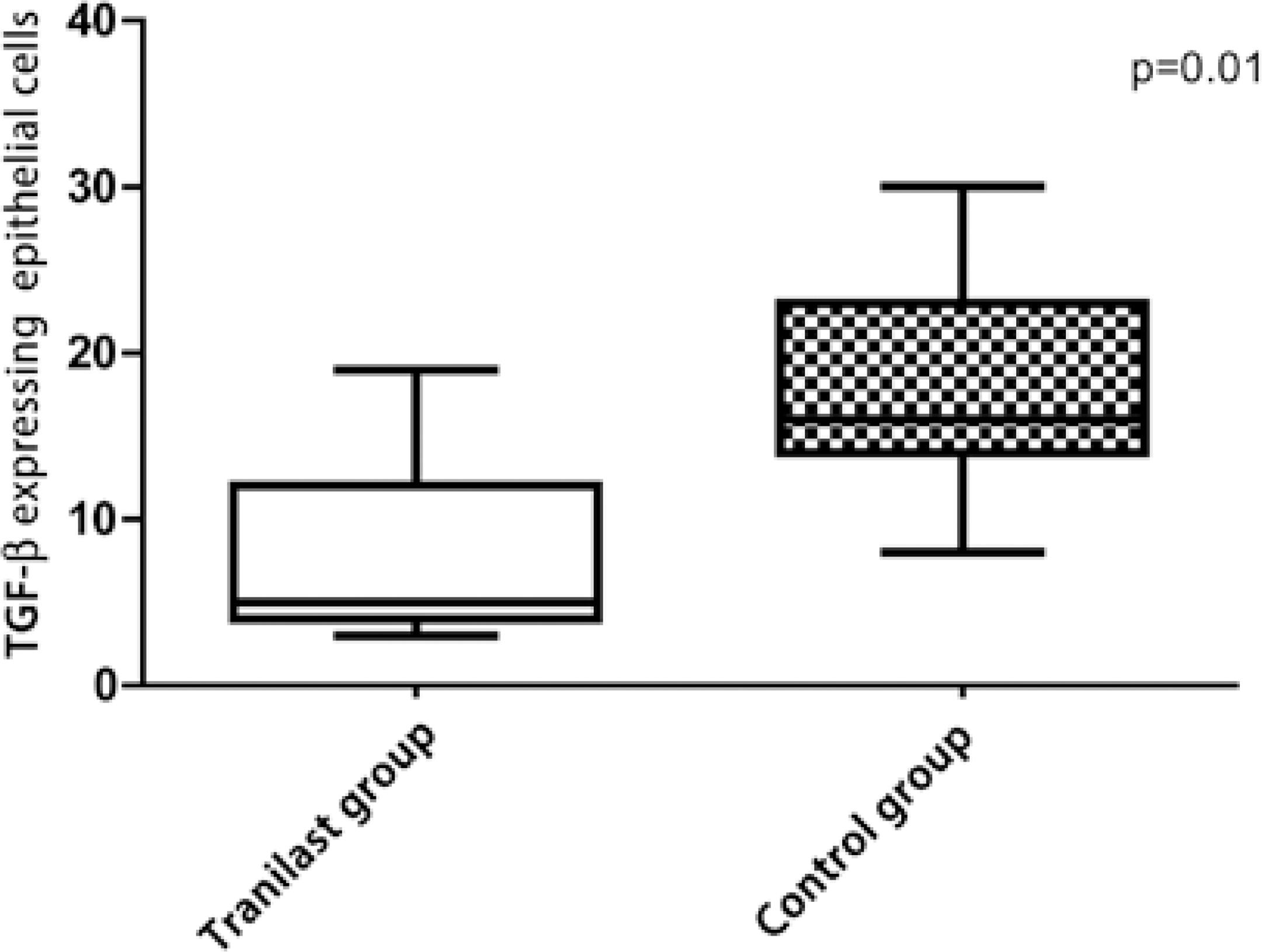
Figure 4 Expression of TGF-β in the epithelial cells of the pterygium in the control group (CG) compared with the tranilast group (TG).
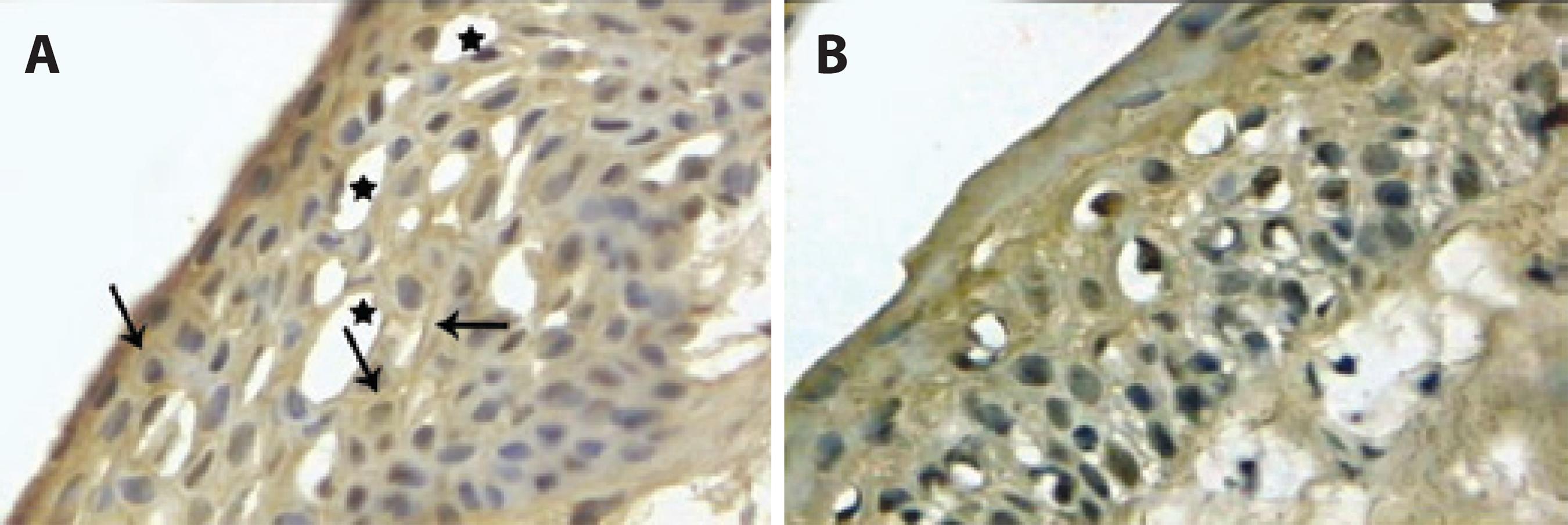
Figure 5 A) Positive immunohistochemical staining for TGF-β in the cytoplasmic membrane (arrows), with predominance in the superficial and middle portions of the conjunctival epithelium of the pterygium. The basal portion of the epithelium is scarcely marked [frozen slides with focal artifacts (star). Magnification: 400×]. B) Negative immunohistochemical staining for TGF-β. The cytoplasmic membrane was not stained. [frozen slides. Magnification: 400×].
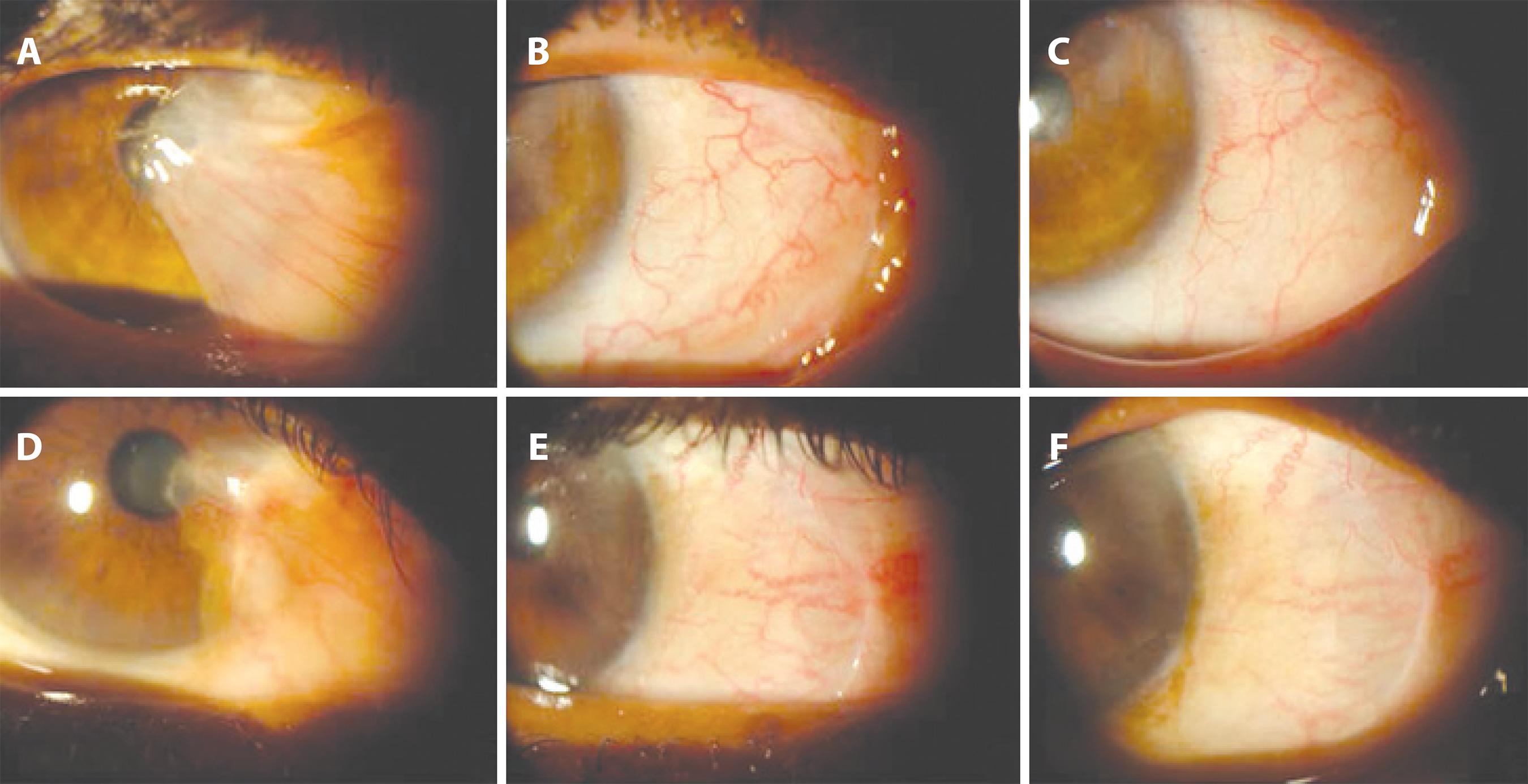
Figure 6 The upper 3 pictures are from a patient in the tranilast group (TG) and the lower 3 pictures are from a patient in the control group (CG). (A) Before surgery, (B) 3 months after surgery, and (C) 6 months after surgery. (D) Before surgery, (E) 6 months after surgery, and (F) 12 months after surgery.
DISCUSSION
The recurrence rates in this study, 6.66% for TG and 14.28% for CG, were similar to other reports using different preoperative and intraoperative regimens with adjuvant mitomycin C. Recurrence rates of 4.54% and 5.4% have been reported in 2 separate studies( 15 , 16 ). Another study reported a recurrence rate of 15% after 4 years of follow-up( 17 ).
The mean age of the patients in this study was 46.43 years for CG and 44.73 for TG. The difference in mean age may explain the higher recurrence rate in our study compared with the patients treated in another study who had a mean age of 60 years( 15 ) because the recurrence rate of pterygium is higher in younger individuals( 18 ).
In a previous study, the 4-year recurrence rate of CAU alone was shown to be 15%, whereas the recurrence rate after the application of mitomycin C on bare sclera alone was 38%( 17 ). In the current study, CAU was combined with mitomycin C in an attempt to combine and enhance the effects of each treatment.
However, it is important to note that the number of samples in each group was too small to determine the efficacy of tranilast. Furthermore, the loss to follow-up was very high (Figure 1), and the power of the study for the variable recurrence was approximately 50%.
Anduze(19) also examined the effect of 0.1 mL of mitomycin C (0.2-0.4 mg/mL) applied directly under the conjunctival flaps postoperatively using a similar procedure to that used in the current study.
Rubinfeld et al.( 6 ) described 10 cases with severe complications that were associated with mitomycin C use after pterygium surgery. The safe dosage of mitomycin C is lower than 0.3 mg/mL( 20 ), and it appears that the drug's effective concentration overlaps with the concentration capable of causing adverse reactions.
The mechanism of action of tranilast differs from that of mitomycin C. Tranilast is safe to use even when the 2 agents are used concurrently, as observed in the present study. Tranilast can inhibit the proliferation and chemotaxis of pterygium-derived fibroblasts( 7 ), as well as collagen synthesis of keloid fibroblasts( 21 ).
There were some concerns in the present study regarding the toxicity of mitomycin, especially for late postoperative complications. However, no complications associated with its use were observed. One patient in CG lost the graft during the early postoperative period, which was possibly due to scratching of the eye. Other complications were granuloma formation and increased eye pressure secondary to corticosteroids.
One case report, in which tranilast ophthalmic solution was used, reported its effectiveness in preventing pterygium recurrence and inhibiting symblepharon and granulomas without adverse reactions( 22 ). However, few studies reported in the literature have assessed both the preoperative and postoperative symptoms associated with pterygium surgery. In the present study, there were no significant differences in the symptoms between the groups and the symptoms typically disappeared 30 days postoperatively (Figures 2 and 3).
TGF-β, which is present in the epithelial cells, stromal cells, vascular endothelial cells, and vascular basal membrane of pterygium tissue, is a multifunctional protein that regulates cell migration, proliferation, differentiation, and apoptosis of many cell types( 23 ). In the normal conjunctiva, positive immunolabeling for TGF-β is much weaker than in pterygium tissue( 24 ). The present study demonstrated moderate expression of TGF-β in pterygium epithelial cells in CG compared with expression in TG (Figure 4).
Although a previous study found that an increase in TGF-β levels in the pterygium was comparable with that in normal conjunctiva( 25 ), the immunohistochemical analysis reported here was similar to the findings of that study, showing that TGF-β was mainly expressed in the pterygium epithelial cells (Figure 5). The numbers of stained epithelial cells were significantly different between the 2 groups (p=0.01; Figure 4). Therefore, tranilast inhibits the secretion of TGF-β1 from conjunctival cells( 26 ).
To the best of our knowledge, this study is the first to report subconjunctival injection of tranilast 30 days prior to pterygium surgery. Tsuji et al.( 22 ) described other options, that include similar administration such as the administration of mitomycin C in the postoperative period, that may be viable.
Based on the above findings, we consider that tranilast ophthalmic solution administered by conjunctival injection before pterygium surgery may effectively decrease TGF-β in epithelial pterygium tissue. In contrast, we routinely use topical steroids and topical antibiotics after most eye surgeries. Therefore, we cannot ignore the possibility that steroids affected the postoperative outcome because they also have strong anti-inflammatory effects, and theoretically, could reduce recurrence after pterygium excision. However, pterygium recurrence often occurs with topical steroids, suggesting that their anti- inflammatory effect is insufficient to prevent recurrence completely.
This study has some limitations, including the absence of a control injection of the tranilast vehicle. TGF-β may interact directly or indirectly during the pathogenesis of pterygium, though this remains to be proven( 24 ).
Subconjunctival tranilast was effective in decreasing the expression of TGF-β in pterygium epithelial cells.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

