INTRODUCTION
After surgical correction of unilateral blepharoptosis, a decrease in the height of the contralateral upper eyelid may be observed(1-3). Gay et al.(4) suggested that the phenomenon may be explained by Hering’s law, which states that the muscles responsible for eye movement in each eye are innervated equally as observed in the lateral and medial rectus muscles during horizontal version. Hering’s law posits that the same amount of stimulus is transmitted to each of the two muscles in a pair. Thus, eyelid position in patients with ptosis would be analogous to the secondary deviation seen in paralytic strabismus(5).
Therefore, in the correction of unilateral ptosis, the innervational stimulus for that eyelid will be lower, causing the fall of the contralateral eyelid and demonstrating an interdependence of eyelid height between both eyelids.
Phenylephrine, a selective α-adrenergic receptor agonist, elevates the upper eyelid, simulating the effect of corrective surgery for blepharoptosis(6). Digital lifting and closure of the ptotic eyelid is also used to simulate the effect of corrective surgery and observe the compensatory change in the position of the contralateral eyelid. This digital lift test is useful in the preoperative assessment, as demonstrated in a study by Kratky and Harvey, in which 46.7% of the patients had positive test results(5).
Few studies have explored the changes in the contralateral upper eyelid produced by phenylephrine instillation in one eye. Similarly, there is a paucity of evidence in the literature regarding the efficacy of digital lift compared with instillation of phenylephrine drops to induce a decrease in the height of the contralateral upper eyelid.
The objective of the present study was to compare instillation of 10% phenylephrine drops with digital lifting of the ptotic eyelid with regard to changes in upper eyelid position in patients with bilateral senile blepharoptosis.
METHODS
The present prospective clinical study included patients with bilateral senile involutional blepharoptosis, and was conducted between June 2011 and September 2012. All patients provided informed written consent. The study was approved by the Ethics Committee for Analysis of Projects and Research at the Clinic Hospital of University of São Paulo Medical Center (HC-FMUSP) under protocol #0213/11.
Subjects presenting with bilateral blepharoptosis with a marginal reflex distance-1 (MDR1) of <2.6 mm were eligible. The exclusion criteria were: corneal changes precluding accurate measurements, use of sympathomimetic drugs or eyedrops, previous eyelid surgery, other types of ptosis (traumatic, mechanical or post-contact lens ptosis), myopathies, and untreated and/or decompensated cardiovascular disease.
At baseline, the patients underwent a complete ophthalmological evaluation, including assessment of visual acuity, pupillary reflexes, MDR1, levator palpebrae superioris muscle (LPSM) function, biomicroscopy, intraocular pressure and fundoscopy.
Subsequently, the patients underwent the following tests:
-
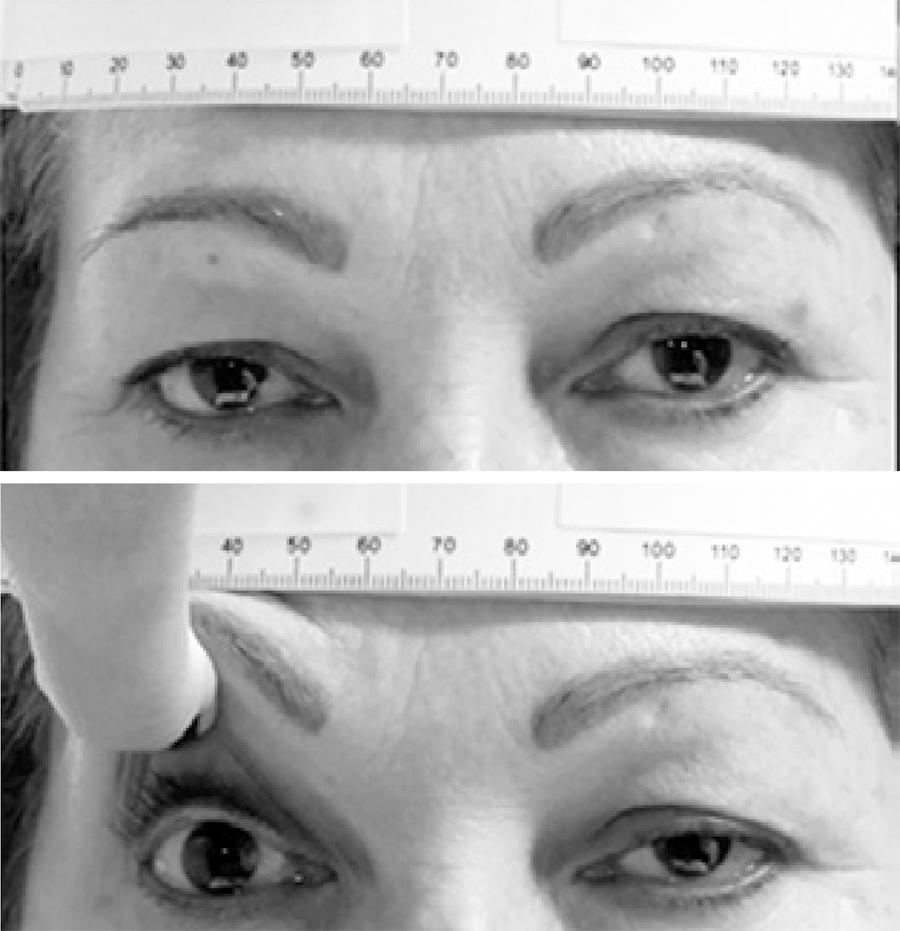
Test 1: Digital lifting of the more ptotic eyelid and observation of the effect of the intervention on the contralateral eyelid (Figure 1).
Test 2: Instillation of two drops of 10% phenylephrine (Allergan; standardized at HC-FMUSP) in the more ptotic eye and obser vation of the effect of the intervention on the contralateral eyelid.
Patients were filmed using a Sony HDR-CX150 digital video camera for 1 min before the tests, during digital lifting, and 5, 10 and 15 min after phenylephrine instillation. The patient’s head was placed on a chin rest at a predetermined distance, with a ruler measuring length in millimeters across the forehead for the calibration of eyelid position measurement. The five video frames in which the patient presented the greatest eyelid elevation were selected and the average of the measurements was calculated. The images were analyzed to determine MDR1 (Imovie software [version 8.0.6] and Image J software [version 1.43r]). The central corneal light reflex was used as reference.
A linear mixed-effects model was used in the statistical analysis because data from the same individuals were grouped and the assumption of independence among observations in the same group was not adequate (Schall, 1991; Littel, 1996). The residue was assumed to have normal distribution with a mean value of zero and constant variance (σ2). The analysis was performed with the SAS software (version 9.2) using the MIXED procedure.
RESULTS
A total of 27 patients, ranging from 52 to 82 years of age (mean 68.51 ± 8.21 years), 24 (88.88%) of whom were women, were included in the present study.
As shown in figure 2 and table 1, which present the MDR1 values of eyes instilled with 10% phenylephrine according to the time of observation, the differences in MDR1 values were significant for all comparisons, except between 10 and 15 min.
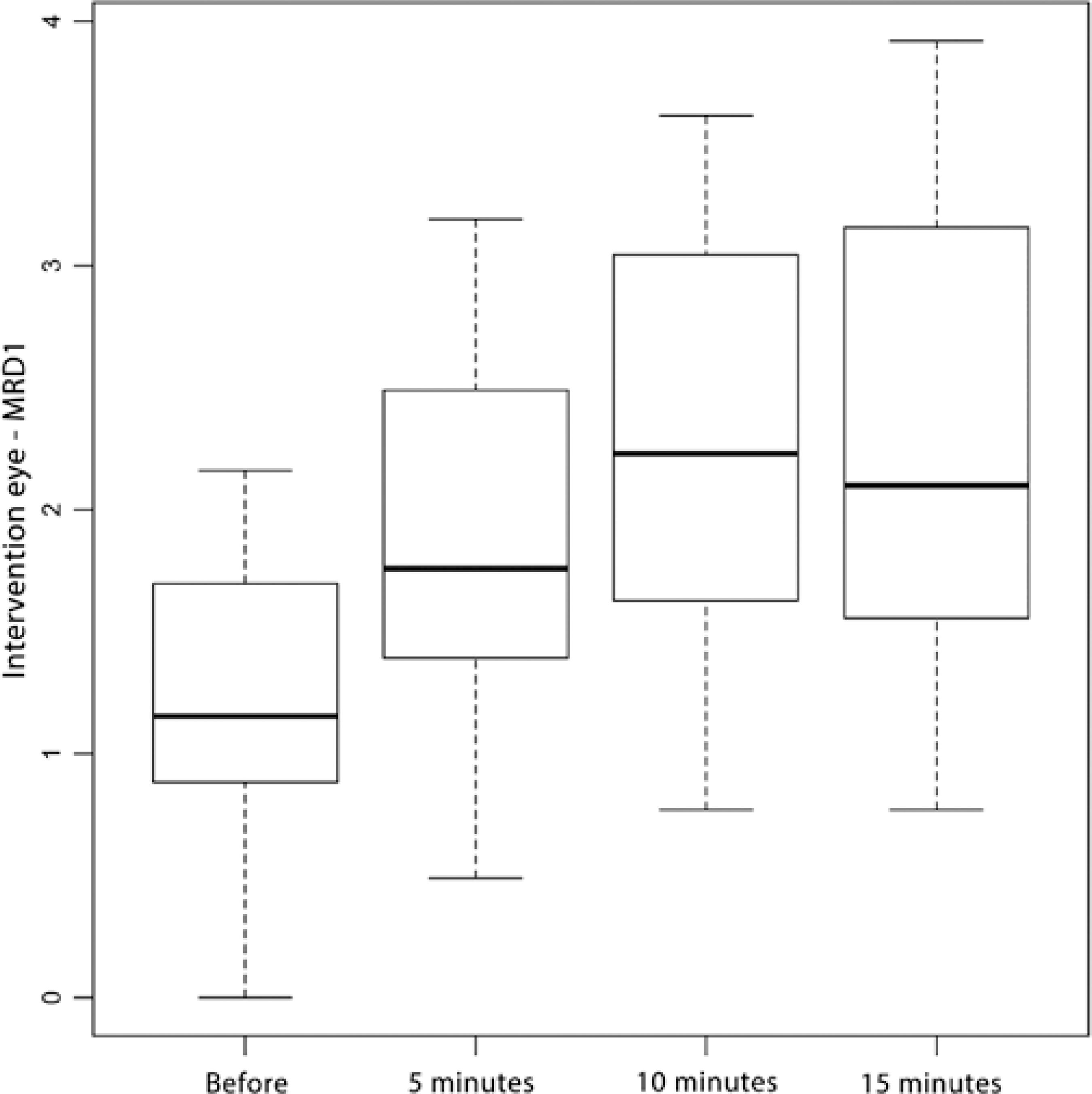
Figure 2 Boxplot showing marginal distance reflex-1 (MRD1) measures of eyes that underwent instillation with 10% phenylephrine according to time of observation.
Table 1 Distribution of marginal distance reflex (MRD1) and results of the linear mixed-effects model in eyes that underwent instillation with 10% phenylephrine according to time of observation.
| Comparison | MRD1 mean values (mm) | Estimate | p-value | LL | UL |
|---|---|---|---|---|---|
| Pre-instillation vs 5 min | 1.21 vs 1.84 | -0.64 | <0.01 | -0.82 | -0.45 |
| Pre-instillation vs 10 min | 1.21 vs 2.27 | -1.06 | <0.01 | -1.24 | -0.88 |
| Pre-instillation vs 15 min | 1.21 vs 2.42 | -1.21 | <0.01 | -1.39 | -1.02 |
| 5 min vs 10 min | 1.84 vs 2.27 | -0.42 | <0.01 | -0.61 | -0.24 |
| 5 min vs 15 min | 1.84 vs 2.42 | -0.57 | <0.01 | -0.76 | -0.39 |
| 10 min vs 15 min | 2.27 vs 2.42 | -0.15 | 0.11 | -0.33 | 0.03 |
LL= lower limit; UL= upper limit (95% confidence interval).
table 1 shows the distribution of MDR1 values for the eyes that underwent phenylephrine instillation.
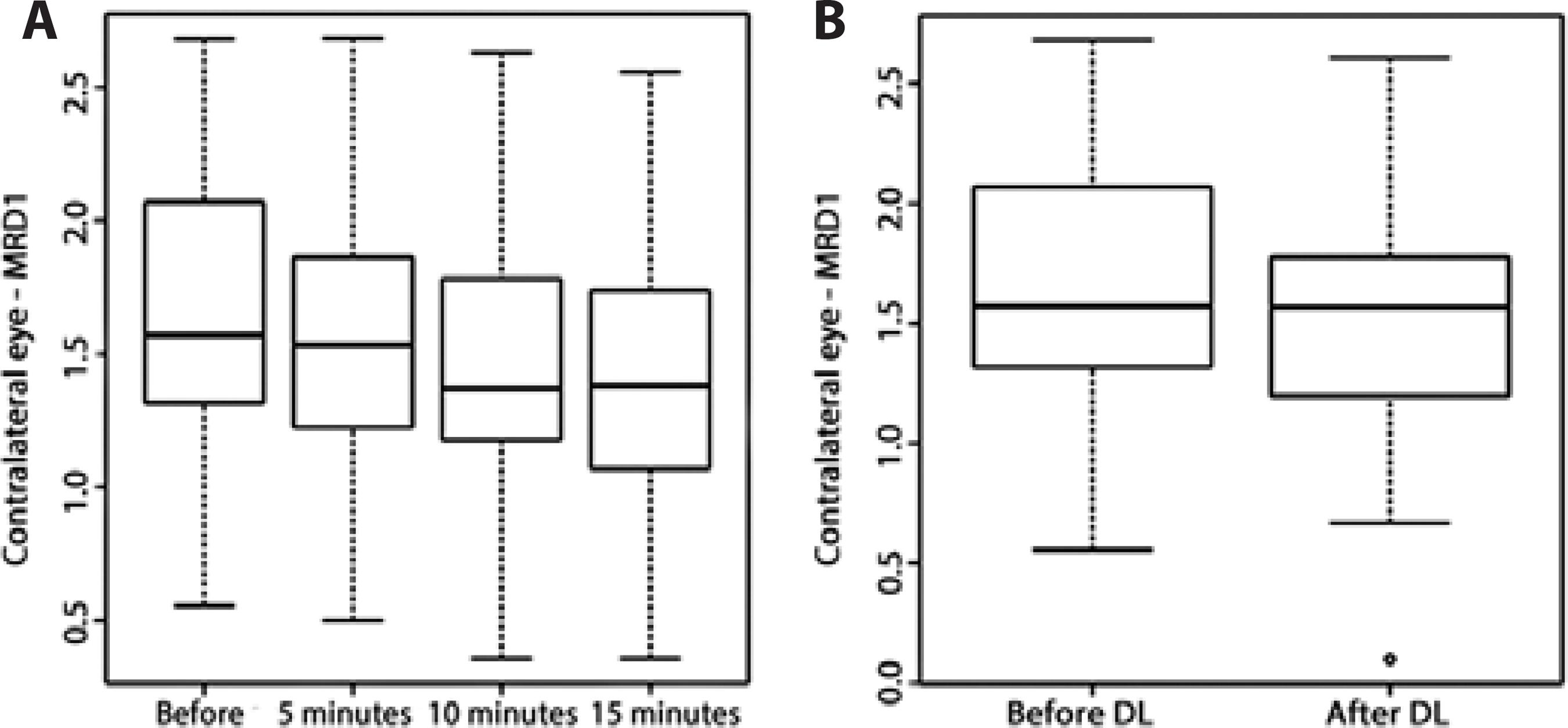
Table 2 shows the distribution of MDR1 values for the eyes contralateral to the eyes that underwent digital lifting or phenylephrine instillation.
Table 2 Marginal distance reflex-1 (MRD1) values for contralateral (non-intervention) eyes according to intervention and time
| Intervention | Mean | SD | Minimum | 1st quartile | Median | 3rd quartile | Maximum |
|---|---|---|---|---|---|---|---|
| Before test | 1.63 | 0.56 | 0.56 | 1.20 | 1.57 | 2.08 | 2.68 |
| DL | 1.51 | 0.53 | 0.10 | 1.19 | 1.57 | 1.86 | 2.61 |
| PI -5 min | 1.52 | 0.55 | 0.50 | 1.20 | 1.53 | 1.94 | 2.68 |
| PI-10 min | 1.44 | 0.56 | 0.36 | 1.15 | 1.37 | 1.79 | 2.63 |
| PI-15 min | 1.38 | 0.54 | 0.36 | 0.99 | 1.38 | 1.79 | 2.56 |
SD= standard deviation; DL= digital lifting; PI= phenylephrine instillation.
As suggested by table 3 and figure 3, the contralateral eyelid tended to be lower after phenylephrine instillation compared with after digital lifting (MDR1=1.38 versus 1.51 mm), and statistically significant differences were observed in both groups (p<0.01 and p=0.02, respectively).
Table 3 Results of the linear mixed-effects model for contralateral (non-intervention) eyes according to intervention and time of observation
| 95% CI | ||||||
|---|---|---|---|---|---|---|
| MRD1 mean values (mm) | Comparison | Estimate | p-value | LL | UL | |
| 1.51 vs 1.63 | DL vs before DL | 0.13 | 0.02 | 0.02 | 0.23 | |
| 1.63 vs 1.52 | Pre-instillation vs 5 min | 0.12 | <0.01 | 0.04 | 0.19 | |
| 1.63 vs 1.44 | Pre-instillation vs 10 min | 0.19 | <0.01 | 0.12 | 0.27 | |
| 1.63 vs 1.38 | Pre-instillation vs 15 min | 0.25 | <0.01 | 0.18 | 0.32 | |
| 1.52 vs 1.44 | 5 min vs 10 min | 0.08 | 0.04 | 0.01 | 0.15 | |
| 1.52 vs 1.38 | 5 min vs 15 min | 0.14 | <0.01 | 0.06 | 0.21 | |
| 1.44 vs 1.38 | 10 min vs 15 min | 0.06 | 0.14 | -0.02 | 0.13 | |
DL= digital lifting; LL= lower limit; UL= upper limit; CI= confidence interval; MDR1= marginal distance reflex-1.
DISCUSSION
In blepharoptosis, one or both upper eyelids droop below the normal position. According to the most widely accepted definition, the condition is diagnosed when the border of the upper eyelid covers >2 mm of the corneal limbus at the 12 o’clock position in the primary position of gaze(7). When the droop is quantified by digital elevation, eyelid measurements tend to be inaccurate. Thus, Sarver and Putterman(8) proposed to detect ptosis based on the distance between the center of the pupillary light reflex and the upper eyelid margin (MDR1), which is clinically equivalent to the distance between the upper eyelid margin and the center of the pupil. Since MDR1 ranges from 2.6 to 4.4 mm in normal individuals, values <2.6 mm are suggestive of blepharoptosis(9). However, other factors, such as facial and/or eyelid asymmetry, facial proportions and racial characteristics, should be taken into account.
Blepharoptosis may present as a simple esthetic change, or as a functional problem if the eyelid covers the visual axis or causes sight impairment in the upper peripheral field.
Patients often unconsciously attempt to compensate the droop by contracting the frontal muscles and the corrugator supercilii, or by tilting the head backwards.
The outcome of corrective surgery for blepharoptosis is difficult to predict and patients often require reoperation, even when treated by experienced surgeons(10). One of the most delicate issues is the descent of the contralateral eyelid following surgical correction of unilateral blepharoptosis.
Several tests have been proposed to predict eyelid position after correction of unilateral blepharoptosis, including digital lifting and closure of the ptotic eyelid, and instillation of phenylephrine.
Bodian(1) observed the appearance of ptosis in the contralateral eye in 9.6% of 115 patients submitted to surgical correction for unilateral blepharoptosis. Likewise, Averbuch-Heller et al.(3) observed the descent of the contralateral eyelid following the elevation of the ptotic eyelid in patients with neuromuscular blepharoptosis. To explain this phenomenon, Gay et al.(4) cited Hering’s law, which states that the muscles responsible for eye movement in each eye are innervated equally (as observed for the lateral and medial rectus muscles during horizontal version) and the same amount of stimulus is transmitted to each of the two muscles in a pair. However, in his original study, Hering did not specify whether the law of motor correspondence applies to the LPSM (Hering apud Gay et al.)(4).
Erb et al.(2 ) observed no significant difference between patients testing positive and negative for Hering’s test prior to surgery. The test involved the digital lifting of the ptotic eyelid and observation of the contralateral eye. Patients were considered to be Hering-positive when a descent of the contralateral eyelid was observed. In both groups, the MDR1 value of the contralateral eye decreased by 0.2 ± 0.8 mm following surgical correction of unilateral blepharoptosis. In other words, negativity for Hering’s effect prior to surgery was not predictive of the absence of postoperative ptosis in the contralateral eye. According to the authors, 5% of the patients required a second intervention(2).
Digital lifting and closure of the ptotic eyelid is also used to simulate the effect of surgical correction of unilateral blepharoptosis and its repercussion on the contralateral upper eyelid. Kratky and Harvey(5) evaluated two tests with the patient looking straight ahead at a distant point: the lift test, in which the examiner digitally lifts the ptotic eyelid as far as the upper limbus while observing the descent of the contralateral upper eyelid; and the closure test, in which the examiner digitally occludes the ptotic eyelid while observing the elevation of the contralateral upper eyelid. The tests may be complemented by rapid release of the position, occluding or elevating the eyelid, respectively. According to the authors, the return to the original position is more easily observed in the contralateral upper eyelid. In their study, changes in the contralateral upper eyelid were observed in 66.7% of the patients with the closure test, and in 46.7% with the lift test(5).
These observations may be explained by the fact that when the ptotic eyelid is corrected in patients with bilateral asymmetric blepharoptosis, the nervous stimulus transmitted to the LPSM on both sides decreases, causing the previously compensated eyelid to droop.
The 10% phenylephrine test is commonly used in the semiology of blepharoptosis. If the eyelid is elevated following instillation, the test is considered to be positive and the patient is referred to surgical correction with müllerectomy(6). In the present study, 10% phenylephrine drops were instilled in only one eye of each patient in order to analyze the effect of the medication on the upper eyelids of both eyes. The choice of medication and concentration was based on the commercial availability of 10% phenylephrine eyedrops and on the fact that the medication is more efficient at 10% than at 2.5%, with an average difference in eyelid elevation of + 0.2 mm, as demonstrated by other authors(11).
Both concentrations have been associated with adverse ocular and/or systemic reactions. Phenylephrine eyedrops are contraindicated in patients with closed-angle glaucoma, children with low body weight and patients potentially hypersensitive to the drug (for example, patients with insulin-dependent diabetes or individuals with a history of cerebral aneurysm, cardiovascular disease or idiopathic orthostatic hypotension)(12,13). Nevertheless, a recent study found no significant difference between the two concentrations (2.5% and 10%) with regard to systemic blood pressure or heart rate. In another study, no clinical problems were observed following the use of phenylephrine eyedrops(14). Likewise, in the present study, none of our patients experienced any local and/or systemic adverse reactions to the medication during or after the intervention.
In the present study, each case was documented using digital images, which were analyzed using a computer for greater accuracy. Eyelid position is not static; thus, to minimize image capture bias, patients were filmed rather than photographed. The method, which has been described in other studies evaluating the eyelid and related structures(15,16), was simple to apply. The semiology employed in the study is the most widely used in the evaluation of blepharoptosis and was based on the measurement of the distance between the center of the pupillary light reflex and the upper eyelid margin (MDR1) and on the 10% phenylephrine instillation test.
In our sample, patients were predominantly female (88.88%). The mean age was 68.51 years.
In eyes treated with 10% phenylephrine eyedrops, MDR1 increased from baseline to the 10 min mark, then remained stable up to 15 min after baseline (Table 1; Figure 2).
With regard to the contralateral eye, a tendency toward descent of the contralateral eyelid following digital lifting was observed, which was statistically significant (p=0.02; 95%CI=0.02-0.23) (Table 3).
As shown in table 3, the difference between the time-points was statistically significant for contralateral eyes regardless of the 10% phenylephrine instillation (p<0.01).
In other words, while changes do occur in the position of the contralateral eyelid during the digital lift test, the difference is very difficult to detect by conventional clinical evaluation.
These findings are supported by Nunes(15) who found contralateral eyelid changes to be detectable solely with the aid of digital image processing due to the greater accuracy of automated measurements. Very small differences detected in this manner may not be perceptible on ectoscopy(15).
In addition, changes in the contralateral eyelids of our patients may have been negligible because the eyelid position, MDR1 values, LPSM function and innervational stimuli tend to be similar on both sides in bilateral senile blepharoptosis.
However, the 10% phenylephrine eye drop test produced substantial changes in MDR1 values in the treated and contralateral eye, indicating clinical and statistical efficiency.
In the clinical context, Hering positivity indicates the presence of blepharoptosis in the contralateral eye as well(17). The cut-off value for bilateral surgery has not yet been defined, but it would be interesting to correlate the changes observed in the present study with Hering test results after surgical correction of unilateral blepharoptosis. However, two previous studies failed to demonstrate a correlation between preoperative Hering positivity and postoperative contralateral upper eyelid position(2,18).
In the present study, we quantified the interaction between eyelids in response to instillation with phenylephrine eyedrops and digital lifting of one of the eyelids, with focus on the effect produced on the contralateral eyelid. In theory, the existence of a feedback effect of the contralateral eyelid on the eyelid submitted to instillation may be postulated, since the palpebral descent resulting from the Hering effect could cause the upper eyelid of the tested eye to rise, thereby indirectly adding to the effect of the medication. This theory is not applicable to the digital lift test because the lifting is performed manually and cannot be measured.
CONCLUSIONS
The 10% phenylephrine eye drop test is more useful than the digital lift test in patients with bilateral senile blepharoptosis because changes in eyelid position in the contralateral eyelid are barely detectable using the digital lift test.
The currently available diagnostic tests for blepharoptosis require further study and development before they can be adequately used in the semiology and treatment of blepharoptosis in the quest for improved palpebral symmetry.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

