INTRODUCTION
Relative pupillary block (PB) is considered to be the primary mechanism for angle closure(1-3). Although laser peripheral iridotomy (LPI) remains the cornerstone of angle-closure management, it does not widen the angle in all cases, as approximately 20%-30% of these patients continue to exhibit appositional angle closure in the presence of a patent iridotomy(1-3). In these cases, non-PB mechanisms, such as lens-induced, plateau iris, and peripheral angle crowding, may be involved(4-7). Argon laser peripheral iridoplasty (ALPI) and lens extraction have been proposed as effective procedures to manage eyes with persistent occludable angles(8-10).
While dealing with cases of primary angle closure (with or without glaucoma), identification of the underlying mechanism is of the utmost importance because each may follow a different course and require a different treatment approach. Although there is extensive information in the literature regarding the main etiologies and guidelines for management of primary angle closure in Asian, North American, and European populations, there are scant data with regard to South American patients(2,11-16). In the present study, we investigated the prevalence and treatment outcomes of angle-closure mechanisms other than pupillary block in a population of Brazilian patients.
METHODS
Patients
After Institutional Review Board approval, a comprehensive chart review was conducted to evaluate consecutive patients who underwent LPI due to occludable angles at a single institution between July 2009 and April 2012. An occludable angle was defined as an eye in which the posterior trabecular meshwork was not visible for ≥180° without indentation on dark-room gonioscopy. Because some eyes may not have irido-trabecular contact even when the trabecular meshwork is not visible, an additional requirement was that corneal and iris beams of light should merge during non-indentation gonioscopy (in order to confirm the presence of irido-trabecular contact). Eyes with previous incisional surgery, with >90° of peripheral anterior synechiae (PAS), ocular trauma, uveitis, or any other form of secondary glaucoma were excluded.
Data collection and procedures
Data collected were age, gender, race, presence of glaucoma, pre- and post-laser intraocular pressure (IOP), number of antiglaucoma medications, angle status and underlying angle-closure mechanisms as determined by gonioscopy and subsequent management during follow-up. All laser procedures, pre- and post-laser gonioscopy assessments and IOP measurements were performed by two experienced glaucoma specialists (LGB and TSP). In all cases, dark-room gonioscopy was performed with and without indentation using a Posner four-mirror lens (Ocular Instruments Inc., Bellevue, WA, USA). The light beam was set at 1-2 mm to avoid illuminating the pupil, and the most posterior region of the anterior chamber angle that was visible without indentation was determined. The angle was classified as occludable or non-occludable based on the previously mentioned definition. Regarding ALPI parameters, a 500 micron spot, 500 ms duration and 250 mW power were routinely used, which could vary according to iris pigmentation and tissue response. The center of a Goldmann 3 mirror lens was used and, after the procedure, prednisolone acetate 1% was administered four times per day for one week.
In brief, the main mechanisms of angle closure could be described as follows: (1) relative pupillary block, which results from increased resistance to the flow of aqueous humor between the pupillary portion of the iris and the anterior lens surface; (2) plateau iris (Figure 1 A), which results from an abnormal anatomical configuration/relationship of the anterior chamber angle and ciliary body and is usually confirmed after a LPI failure; and (3) lens induced (Figure 1 B), which involves a normal or large lens pushing the iris forward and resulting in a reduced anterior chamber volume and angle-closure(4-7).
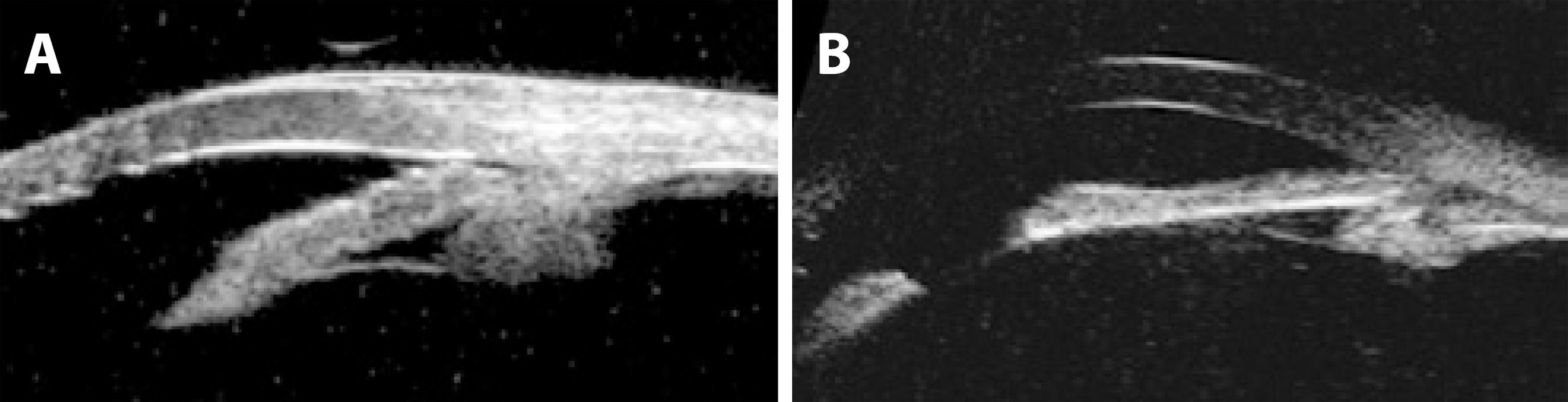
Figure 1 Ultrasound biomicroscopy images of two patients with persistent occludable angles following laser peripheral iridotomy due to plateau iris (A) and lens-induced component (B).
On indentation gonioscopy, eyes with a relatively deep central anterior chamber and irido-trabecular contact after LPI in which the “double hump sign” was identified were considered to exhibit plateau iris component. On the other hand, those with a shallower central anterior chamber in which the iris appeared to drape the anterior surface of the lens, giving rise to a “volcano-like” configuration were considered to exhibit the lens-induced component(5,8). Ultrasound biomicroscopy was used in most cases of persistent occludable angles following LPI.
Statistical analysis
Descriptive analysis was used to present demographic and clinical data. D’Agostino-Pearson’s test was performed to determine whether the data had a normal distribution. The paired-samples T-test was used to compare continuous normally distributed variables, while the Wilcoxon signed-rank test was used to compare those that were non-normally distributed. Baseline IOP was determined as the average of three measurements prior to the laser procedures. Post-laser IOP was based on a single measurement (IOP measurement on each patient’s last visit). The treatment regimen was not altered until the final follow-up visit. If both eyes were eligible for inclusion, the right eye was arbitrarily chosen for analysis. Statistical significance was set at p<0.05. Computerized analysis was performed using MedCalc software (MedCalc Inc., Mariakerke, Belgium).
RESULTS
A total of 196 eyes of 196 consecutive patients (mean age 58.3 ± 11.6 years; 133 women and 36 men) who underwent LPI were included. Primary angle-closure suspects/primary angle closure constituted 54% of the cases, primary angle-closure glaucoma 40% and acute angle-closure glaucoma 6%. In most of the cases (86%), LPI successfully opened the angle. Mean IOP was reduced from 18.3 ± 6.4 to 15.4 ± 4.5 mmHg after LPI (p<0.01).
Forty-one eyes (27 patients) had persistent occludable angles after LPI, comprising approximately 14% of the cases that had previously undergone iridotomy. Among these cases, the most common angle-closure mechanisms were plateau iris (56%) and lens-induced component (34%). Regarding the remaining 10% of the cases of persistent occludable angles (without characteristics of plateau iris or lens-induced component), most eyes had a thick peripheral iris with prominent circumferential folds, occupying a large proportion of the angle, and were classified as thick peripheral iris roll (or peripheral iris crowding)(4,5). Patients with plateau iris were mostly women (75%) and younger (mean age 55.3 years) than those with lens-induced component (mean age 64.8 years; 30% women; p≤0.03). None of the patients were taking pilocarpine prior to the laser procedures. Table 1 summarizes the clinical characteristics of these patients.
Table 1 Characteristics of patients with persistent occludable angle due to non-pupillary mechanisms*
| Variables | Patients (n=27) |
|---|---|
| Mean age (years) | 58.9 ± 11.8 |
| Gender % (men/women) | 44/56 |
| Race % (white/black/asian) | 78/15/7 |
| Presence of glaucoma (%) | 63% |
| Angle-closure mechanisms % (PIC/LIAC/others) | 56/34/10 |
| Mean IOP before ALPI (mmHg) | 17.9 ± 4.9 |
| Mean IOP after ALPI (mmHg) | 14.5 ± 4.2 |
*Data are presented as mean ± standard deviation whenever indicated. ALPI= argon laser peripheral iridoplasty; IOP= intraocular pressure; LIAC= lens-induced angle closure; PIC= plateau iris component.
Most of these cases of persistent occludable angles following LPI were treated with laser iridoplasty (85%). Regarding the four other patients, two had cataracts associated with low visual acuity and underwent phacoemulsification with intraocular lens implantation, and two were treated with pilocarpine at night-time. Treatment regimens were not changed until the final follow-up visit (mean length of follow-up, 11.4 ± 3.6 months; mean number of antiglaucoma medications, 1.7 ± 1.3). Approximately 90% of the cases showed non-occludable angles following ALPI. Intraocular pressure was significantly reduced from 17.9 ± 4.9 to 14.5 ± 4.2 (p<0.01) with no significant differences between patients with plateau iris and lens-induced components (p=0.34). Although some cases of photophobia were noted, there were no cases of peripheral anterior synechiae formation.
DISCUSSION
Recent estimates show that >67 million individuals around the world have glaucoma. Although open-angle glaucoma comprises approximately two-thirds of these cases, angle-closure glaucoma is present in one-half of patients who are blind from the disease(17,18). In addition, in populations such as Chinese, Indian and Mongolian, the prevalence of angle-closure glaucoma is as high or even higher than that of open-angle glaucoma(16,17,19-22). Therefore, angle-closure glaucoma has a considerable impact on daily clinical practice. Evaluating a large series of patients with primary angle closure (with and without glaucoma), we determined the most frequent underlying angle-closure mechanisms and the outcomes of laser treatment (both iridotomy and iridoplasty). To the best of our knowledge, the present study is the first to report on such findings in a large sample of Brazilian patients.
At this point, we believe it is important to discuss the clinical implications of our findings. Treatment of primary angle-closure is directed toward two goals: to eliminate the mechanism of angle closure and to control IOP elevation(14). Previous studies have shown that following LPI, approximately 20%-30% of these patients continue to exhibit appositional angle closure in the presence of a patent iridotomy(1-3). In our study, we found a slightly higher success rate, as 86% of the eyes showed non-occludable angles following LPI. Although these differences may be the result of a lower prevalence of non-pupillary block mechanisms in our study population, we believe that age (the mean age of our study population was <60 years and, thus, the prevalence of lens-induced component was likely low) and the fact we excluded patients with >90° of PAS should be taken into consideration.
Although laser iridotomy is currently the first line of treatment, many eyes will continue to exhibit appositional angle-closure, and an additional treatment option may be necessary(2,3). In the present large consecutive series, ALPI was highly effective in eliminating residual appositional angle closure caused by mechanisms other than pupillary block. In addition, we documented a 20% IOP reduction on average. Our results not only confirm the important role of ALPI in cases of plateau iris(8), but also suggest that it may be an effective alternative in cases involving lens-induced component. We believe that this is clinically meaningful, as not every case of lens-induced angle closure necessarily coexists with a symptomatic cataract. In fact, this appears to be the case of our study population, which is mostly composed of middle-aged patients. It is noteworthy that ALPI has also been successfully used as an initial treatment to break acute phacomorphic attacks(23). Regarding the few cases in which ALPI was not effective in our series, the proportion was similar between eyes with plateau iris and lens-induced component, and we could not identify any predictors of success or failure. As additional findings, our plateau iris patients tended to be women and younger than those with lens-induced component, and ALPI effectiveness was similar in both angle-closure mechanisms during an average follow-up period of almost one year.
We believe it is important to stress some specific characteristics and limitations of our study. First, our study is based on retrospective data and had a relative short follow-up period. Therefore, success rates, especially related to ALPI, may have been positively influenced. Second, a subjective gonioscopic criterion was adopted for each angle-closure mechanism. Moreover, ultrasound biomicroscopy images were available for most patients with persistent occludable angles following LPI, but not for every patient. These missing ultrasound biomicroscopy data could have added useful information (such as anterior chamber depth measurements) to our results. Third, ideally, different examiners should have performed pre- and post-laser gonioscopic examinations. However, the present study was retrospective, and each glaucoma specialist performed not only the laser procedure, but also baseline and post-laser gonioscopy assessments. This potential bias of data collection should be considered while interpreting our results. Fourth, although Brazil is a multiracial country, our patients were enrolled from just one center (in the city of Osasco, São Paulo). Therefore, our results may not be representative of the entire Brazilian population. However, it should be emphasized that São Paulo has a high rate of immigration and, as a result, its population is composed of individuals from all over the country.
In conclusion, our findings suggest that, in this population of Brazilian patients, several eyes with angle closure were not completely treated with LPI. In the present large series of middle-aged patients, plateau iris was the leading cause of persistent angle closure and was effectively treated with ALPI. A detailed eye examination with indentation gonioscopy should always be performed after LPI to rule out persistent angle closure due to non-pupillary block mechanisms.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

