INTRODUCTION
Congenital dacryocystocele is a rare type of lacrimal duct obstruction. Classically, it is described as a bluish mass, 1 cm in diameter and with a cystic and firm consistency, that is located below the medial canthal tendon(1). It is important to distinguish this from other masses such as hemangioma, dermoid cyst, and nasal glioma that could appear in this region. The greatest risk in congenital dacryocystocele is the development of an infectious process by external agents, the acute dacryocystitis, which demands daily monitoring and antibiotic therapy at the first signs. In cases of dacryocystocele, the most appropriate course of action is early diagnosis before the onset of an infection, so that the block in the lacrimal duct can be removed under anesthesia.
Here, we present a case of congenital dacryocystocele diagnosed during the prenatal phase and confirmed after birth, which when treated clinically and surgically, responded with positive results.
CASE REPORT
CAL, an 11-day-old, white female, had a bluish mass of cystic firm consistency below the medial canthal tendon on her left side. A fetal morphological ultrasound scan (2- to 4-MHz transducers) performed at 40 weeks of pregnancy showed a discreet bilateral cystic swelling on the epicanthus (Figures 1 A and B).
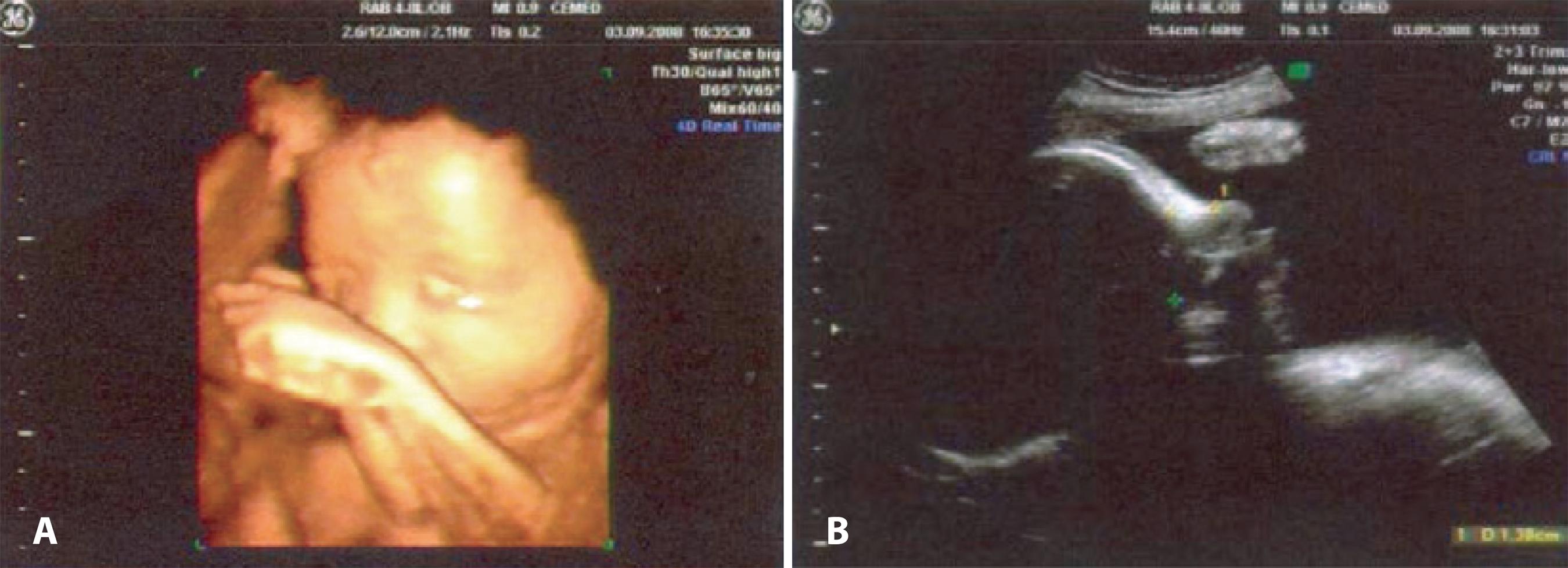
Figure 1 Intrauterine ultrasonography of a 40-week-old fetus. A) Three-dimensional reconstruction ultrasonography (2-MHz linear transducer), where a swelling can be seen in the region of the left eye epicanthus (white arrow). B) The cephalic frontal seccional image (4-MHz linear transducer) shows a cyst formation with hypoechogenic content (cross mark) that is consistent with dacryocystocele.
A computer tomography (CT) scan of the sinuses and the orbit revealed an epicenter oval formation in the left nasolacrimal duct, advancing to the nasal cavity and measuring approximately 3 cm in diameter.
Fourteen days after birth, an infectious process developed in the area (Figure 2 A), prompting a 10-MHz B-scan ultrasound evaluation of her left lacrimal sac (Figures 2 B and C). The patient was treated with 100-mg/mL liquid cephalexin (Keflex), 1.0 mL every 6 hours for 7 days. Two days after the resolution of the condition, the lacrimal duct was probed with bilateral intubation under general anesthesia. After the procedure, she was prescribed instillation of topical medication (5.45 mg moxifloxacin hydrochloride + 1.10 mg disodium phosphate) (Vigadexa eye drop, Alcon), four times a day for 7 days. The outcome of evolution was considered to be positive.

Figure 2 A) Clinical photograph of a 14-day-old nursling who presented a bluish cystic swelling in the region below the medial canthal tendon of her left eye, associated to redness, hyperemia, and local heat, characteristic of an infectious process or acute dacryocystitis. B and C) B-mode ultrasonography (10 MHz, skin contact technique) revealed a cystic cavity with an ostium that was seemingly connected to the left nasolacrimal duct, characterizing the dilatation of the lacrimal sac (5.4 x 6.4 mm) without communication with the eye. D) Clinical response after antibiotic therapy, followed by surgical probing and intubation of the left lacrimal duct, which shows a smaller and reducing local swelling.
After 15 days, the bilateral lacrimal duct intubation was removed and the left cystic lesion showed gradual involution. At one month postoperatively, there was a total regression of the lesion (Figure 2 D).
DISCUSSION
Congenital stenosis, inflammatory diseases, tumors, and malformations are the primary causes of lacrimal obstruction in newborn babies and nurslings.
Dacryocystocele, which usually develops in the first weeks after birth, is a result of the anatomical obstruction of the Hasner valve and functional obstruction of the Rosenmuller valve. These obstructions cause lacrimal sac strain, and is usually associated with a mass. When the lacrimal sac is filled with mucus it is called mucocele, and when it is filled with amnion it is called an amniocele(2).
Most cases of dacryocystocele resolve spontaneously, either during the intrauterine process or immediately after birth. Spontaneous resolution may occur in 78% of the cases before the third month after birth and in 91% before the sixth postnatal month(3). Cavazza et al., has described the predominance of unilateral lesions and a higher prevalence in females(4).
Mucocele may occur as a result of the accumulation of mucous secretion, which may extend into the nasal cavity, causing difficulties in breathing and feeding to the newborn. In these cases, the diagnosis must distinguish mucocele from choanal atresia, dacryocystitis, and nasal masses (encephalocele, glioma, and hemangiomas)(5).
Prenatal diagnosis can be made with the help of intrauterine ultrasound. This non-invasive diagnostic method allows the identification and differentiation of different masses and contributes to the future follow-up and treatment during the neonatal period.
Ultrasonography, which eliminates the need for sedation, is a reliable method for the differential diagnosis of dacryocystocele. Additionally, it allows the examination of the content of dacryocystocele, showing fluids and debris present in the lacrimal sac(6).
Other image-based techniques such as CT and magnetic resonance imaging (MRI) scans are equally effective for the diagnosis of cystic lesions. However, these methods are usually employed only when the previous diagnosis is inconclusive. The CT and MRI scans may be performed without the use of a lacrimal duct catheter, applying only a contrast medium in the conjunctive sacs. These methods are less invasive than the conventional dacryoscintilography and allow a more functional analysis of the lacrimal ducts. CT scan uses iodine contrast and MRI uses saline or gadolinium, depending on the chosen pulse sequence. MRI supports excellent characterization of the lacrimal sac content, showing whether the fluid content is more homogeneous or thick with high protein levels (consistent with inflammatory conditions). CT scan offers the advantage of allowing detailed evaluation of the lacrimal bone structure and determination of the bone components in the lacrimal obstructions(7).
Since these exams are performed during the neonatal period, they demand anesthesia. Additionally, tomography uses radiation.
Although congenital dacryocystocele could be resolved with the help of classical methods such as the local application of heat, treatment with antibiotics is required when there is an infection. Further, surgical intervention becomes necessary in cases where the clinical procedures prove to be ineffective.
The condition in our patient was diagnosed during an intrauterine ultrasonography. This exam allows doctors to detect changes in the nasolacrimal duct as early as the eighth month of pregnancy(8). In the present case, the prenatal diagnosis through ultrasonography helped minimize the potential risks of complication. Since the pathology had already been described, treatment with antibiotics began soon after detecting the infectious process. A lack of response after 14 days prompted a probe with intubation. Surgical intervention is recommended in cases of dacryocystitis, cellulitis, breathing difficulty caused by nasal cysts, and when the cyst does not fully regress after a period of employing the initial classical approach. Probing reduces the risk of dacryocystitis, improving the treatment success rates(9).




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

