INTRODUCTION
Uveal metastasis of carcinoma is the most common cause of ocular malignancy in adults(1,2). Breast carcinoma and lung carcinoma cases combined account for 71-92 % of the uveal metastases. Other malignancies such as prostate carcinoma and gastrointestinal carcinoma contribute only to a lesser extent(2). A few cases of choroidal metastasis from pancreatic carcinoma have been reported(3-6). Here we report a case of bilateral choroidal metastasis of pancreatic cancer and its clinical presentation.
CASE REPORT
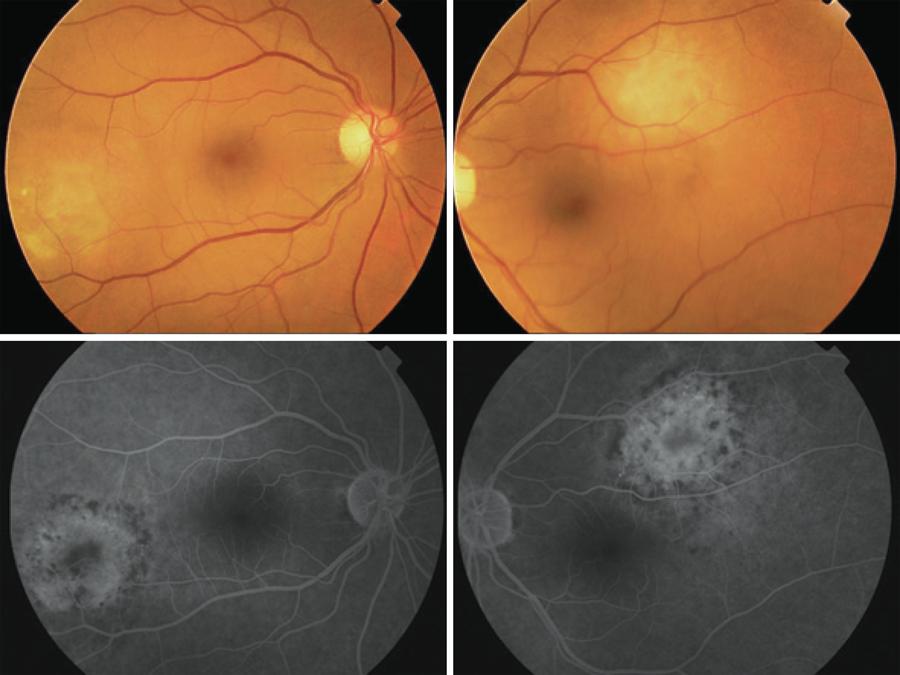
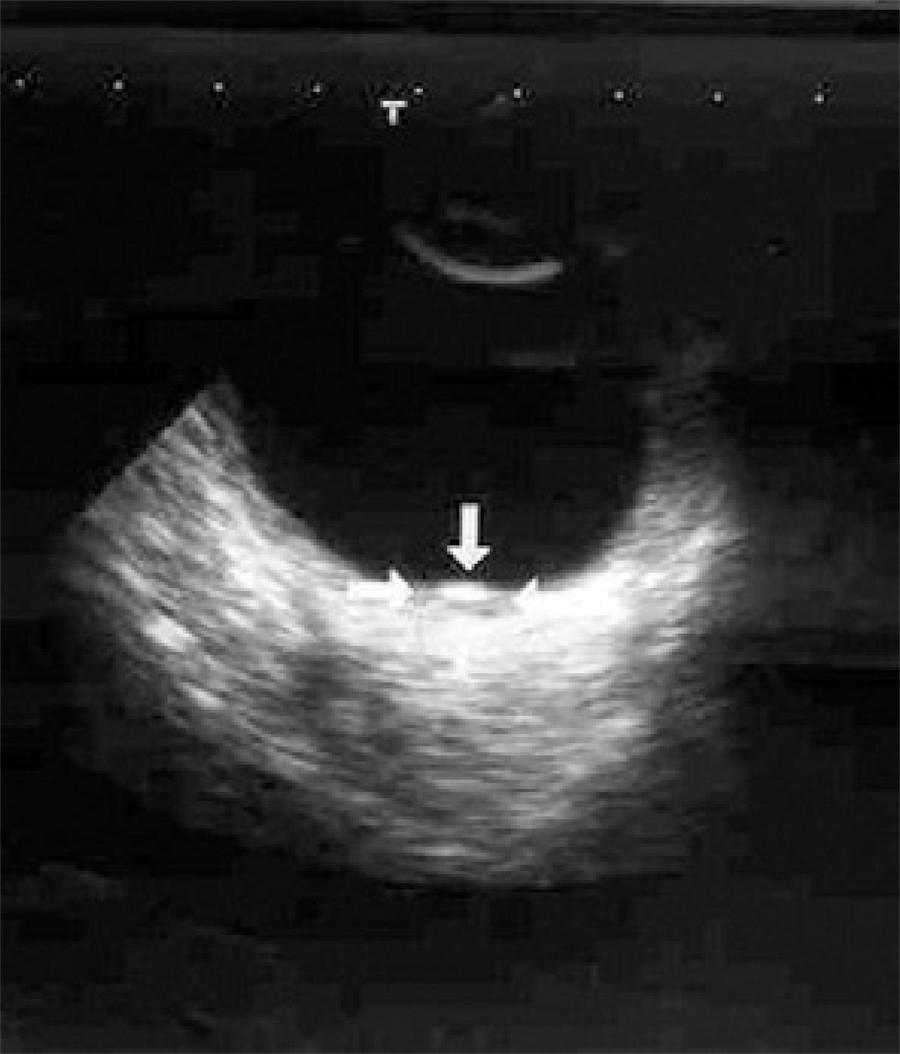
A 49-year-old woman with metastases of pancreatic cancer to liver, spleen, multiple abdominal lymph nodes, and additionally with peritonitis carcinomatosa was presented to the Ophthalmology Department of the Akdeniz University Hospital with a two week history of blurred vision in her left eye two months after the diagnosis. Her best-corrected visual acuities were 20/20 for the right and 20/200 for the left eye. Intraocular pressure and external appearance were normal in both eyes. A slit-lamp examination showed no sign of intraocular inflammation. Fundus examination revealed a white-yellow dome-shaped subretinal mass of 2 optic disc diameters infero-temporal to the macula with minimal subretinal fluid on the right and a white-yellow dome-shaped subretinal mass of approximately 3 optic discs in diameters supero-temporal to the macula with shallow subretinal fluid involving juxtafoveal region (Figure 1). Pigmentary alterations at the border of both lesions were evident. Ocular USG confirmed bilateral choroidal mass, suggestive of metastasis (Figure 2). Although the lesion threatened the vision and demanded radioactive plaque brachytherapy, the medical condition of the patient deteriorated rapidly. Despite further chemotherapy, the patient died six months after the diagnosis of ocular metastasis. During the follow-up bedside exams, a subjective improvement in vision was noted and the left choroidal lesion shrunk to the diameter of one disc with no subretinal fluid. The choroidal dome-shaped mass on the right eye fully regressed and we observed retinal pigmentary changes, two discs in diameter, in place of the original lesion.
DISCUSSION
Here, we report a case of bilateral choroidal metastasis of pancreatic cancer. Pancreatic cancer ranks fourth among the cause of cancer-related deaths in the United States(7). Majority of the patients present a stage IV disease, with metastasis occurring mainly into the liver and peritoneal cavity(5).
Bilateral metastasis of pancreatic cancer into choroid is extremely rare. Shields et al.(8) reported 950 cases of uveal metastases in 520 eyes of 420 consecutive patients, of which only 1 man (<1%) had pancreatic cancer. Shah et al.(6) described a patient with bilateral choroidal metastasis. The only other bilateral case reported was in French literature(4). The present case was only the third with bilateral choroidal metastasis.
Blurred vision is the most commonly presented symptom of uveal metastasis. Other common symptoms include photopsia, scotoma, floaters, metamorphopsia, and ocular pain(2). The symptom of pain is rare in primary uveal malignancies. Typical choroidal metastases show one or more solitary and slightly elevated lesions with depigmentation and hyperpigmentation on the surface. Exudative detachment may or may not be present. It is not possible to know the origin of the lesions from fundus examination alone. Detailed abdominal and thoracal imaging should be performed when rapidly growing choroidal tumors of unknown origin are present(5,8).
The reported cases had systemic metastasis(5). Metastasis to multiple organs was also evident in the present case. Ocular metastasis of malignant tumors is a poor prognostic sign, with a reported life expectancy of 0.2 to 48 months(2,3). Ocular metastasis is treated with chemotherapy combined with brachytherapy to reduce the size of the metastatic lesion, if the lesion causes vision loss(9). Other therapeutic options include external beam radiotherapy, photodynamic therapy, and observation (for detecting intraocular complications)(10,11). Unfortunately, the medical condition of our patient worsened and she could not tolerate radiotherapy for ocular metastasis. We observed that the subjective and objective improvements of the features were a result of the chemotherapy.
Several screening studies have shown that most patients with uveal metastasis are asymptomatic, and when patients become symptomatic, the symptoms generally worsen rapidly. In conclusion, bilateral uveal metastasis can be related to systemic disseminated disease and influence life expentancy. Intraocular metastatic lesions should be treated as a systemic disease.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

