INTRODUCTION
The changes in anterior chamber depth (ACD), anterior chamber angle (ACA), and pupil diameter (PD) that occur during the eye's accommodation, have been extensively studied. Table 1 is a compilation of the results of all studies that evaluated at least one of these three eye metrics during accommodation. Studies assessing the changes in central ACD(1-28), mean ACA(16), and PD(3,7,26,28,29) during accommodation concluded that these metrics decreased after increasing the stimulus vergence. Figure 1 is a side-by-side comparison of two Scheimpflug images that show central ACD for far vision and for -4 diopters (D) of accommodation.
Table 1 Results of reported studies that assessed the anterior chamber depth (ACD), anterior chamber angle (ACA), and pupil diameter (PD) with accommodation. The negative sign indicates a decrease in the ACD, ACA, or PD
| Reference | Device used | Number of eyes | Mean age ± SD (age range) | Refractive error ± SD (refractive error range) | Mean change in ACD (mm) | ACA value (degrees) | Mean change in PD value (mm) |
|---|---|---|---|---|---|---|---|
| Alderson et al.(1) | Lenstar | 10 | 29 (22-39) | -2.11 ± 2.50 (-6.00 – +0.38) | After -5 D: -0.22 ± 0.06 | - | - |
| Baikoff et al.(2) | OCT | 1 albino eye | 19 | 2 | After -10 D: -0.407 | - | - |
| Baikoff et al.(3) | OCT | 104 | 39 ± 15.20 (7-82) | (-5.00 +5.00) | After mamimum accommodation, with 20 years: -0.30 | - | After -10 D in dim light: -1.5 |
| After maximum accommodation, with 40 years: -0.10 | - | - | |||||
| After mamimum accommodation, with 65 years: 0.00 | - | - | |||||
| Bolz et al.(4) | PCI | 10 emmetropic | 23.00 ± 2.40 (19-31) | -0.03 ± 0.08 | After -1 D: -0.01 | - | - |
| (-0.25 – 0) | After -2 D:-0.05 | ||||||
| After -3 D: -0.12 | |||||||
| After -4 D: -0.19 | |||||||
| After -5 D: -0.27 | |||||||
| 10 myopic | 24.70 ± 3.90 (19-31) | -4.70 ± 1.50 | After -1 D: -0.33 | - | - | ||
| (-7.25 – -2.75) | After -2 D:-0.55 | ||||||
| After -3 D: -0.14 | |||||||
| After -4 D: -0.22 | |||||||
| After -5 D: -0.25 | |||||||
| Drexler et al.(5) | PCI | 10 eyes | 30 (25-39) | (-5.25 – -0.25) | At near point:-0.186 ± 0.09 | - | - |
| Du et al.(6) | UBM | 37 | 28.8 ± 6.9 (20-40) | -16.71 ± 4.64 (-23.86 – -8.63) | After pharmacological accommodaion: vertical: -0.18 ± 0.16 horizontal: -0.15 ± 0.09 | - | - |
| Du et al.(7) | UL-OCT | 41 | 33.5 ± 6.9 (21-41) | -2.50 ± 2.60 | After -5 D: -1.43 | - | After -5 D: -1.117 |
| Dubbelman et al.(8) | Scheimpflug camera (Nidek Eas-1000) | 65 | 32 ± 9 (16-51) | -1.4 | Change per diopter: -0.048+0.0004* age | - | - |
| Garner et al.(9) | A-Scan | 11 | 21.2 (18-28) | -1.88 ± 1.64 | After -1.50 D: -0.02 | - | - |
| (-4.25 – +0.50) | After -3.50 D: -0.09 | ||||||
| After -5.50 D: -0.20 | |||||||
| After -8.00 D: -0.24 | |||||||
| Kaluzny et al.(10) | Ultrasound biometry | 372 | 11.30 ± 4.43 (4-9) | (-9.00 – +9.00) | After maximal accommodative effort in: emmetropic group: -0.14 ± 0.14 myopic group: -0.07 ± 0.13 hyperopic group: -0.24 ± 0.16 | - | - |
| Kasthurirangan et al.(11) | MRI | 15 | 22.8 ± 3.1 (19-29) | ± 0.75 D sphere less than 0.50 D cylinder | At near viewing: -0.31 ± 0.30 mean diopters near viewing: [6.9 to 4.8] | - | - |
| Kirschkamp et al.(12) | A-Scan | 9 | (20-38) | - | After -4 D: -0.2 | - | - |
| Koivula et al.(13) | OCT | 41 myopic | 24-49 | -6.30 (-14.50 – -3.50) | After -4.50 D: -0.32 | - | - |
| 11 hyperopic | 2.60 (1.10-3.80) | After -4.50 D: -0.28 | - | - | |||
| Koretz et al.(14) | Scheimpflug Slit lamp | 41 | (18-40) | (-2 – +2) | After -1 D: -0.037 ± 0.026 | - | - |
| Mallen et al.(15) | IOLMaster | 30 emmetropic | 21.40 ± 2.00 | -0.07 ± 0.23 | After -6.00 D: -0.19 ± 0.05 | - | - |
| 30 myopic | 21.5 ± 2.10 | -3.59 ± 0.75 | After -6.00 D: -0.18 ± 0.03 | ||||
| Marchini et al.(16) | UBM | 26 eyes with monofocal IOL implantation | 76 ± 6 (66-87) | - | After -3 D: -0.03 ± 0.30 | After -3 D horizontal: -1.22 ± 5.81 vertical: -0.75 ± 4.87 | - |
| UBM Hi-Scan | After -3 D: -0.04 ± 0.09 | After -3 D horizontal: -1.08 ± 3.53 vertical: -4.15 ± 2.98 | - | ||||
| Malyugin et al.(17) | OCT | 31 emmetropic | 25.9 ± 2.3 (20-33) | -0.39 ± 0.33 (-1.00-0.13) | After -1 D: -0.03 ± 0.03 | - | - |
| After -3 D: -0.12 ± 0.06 | |||||||
| After -6 D: -0.19 ± 0.08 | |||||||
| After -10 D: -0.21 ± 0.08 | |||||||
| 36 myopic | 26.6 ± 4.5 (19-35) | 12.52 ± 4.07 (-20.00 – -6.25) | After -1 D: -0.05 ± 0.03 | - | - | ||
| After -3 D: -0.09 ± 0.05 | |||||||
| After -6 D: -0.12 ± 0.07 | |||||||
| After -10 D: -0.13 ± 0.06 | |||||||
| Ni et al.(18) | Pentacam HR | 23 | 24.40 ± 2.60 (18-29) | 0.00 | After -5 D: -0.11 | - | - |
| 15 | 55.70 ± 5.10 (43-58) | 0.00 | After -1 D: -0.01 | - | |||
| Ostrin et al.(19) | A-Scan | 22 | 25.80 ± 2.30 (21-30) | Right eye -2.53 ± 1.98 (-6.00 – +0.75) | After -1 D: -0.051 ± 0.01 | - | - |
| Left eye: -2.52 ± 2.19 (-5.75 – +2.75) | |||||||
| Petternel et al.(20) | PCI | 11 myopic | 38.00 ± 9.00 (19-53) | -16.10 ± 2.60 (-23.30 – -9.40) | After -3 D: -0.04 ± 0.07 | - | - |
| 2 hyperopic | +6.60 ± 1.10 (+5.50 – +7.80) | - | |||||
| Poinoosawmy et al.(21) | Haag-Streit | 125 | (35-70) | (-1.75 – -0.25) | Pharmacological accommodation: | - | - |
| Pachometer Slit-image photography | After 15 minutes: -0.44 | ||||||
| After 30 minutes: -0.55 | |||||||
| After 60 minutes: -0.57 | |||||||
| Read et al.(22) | Pentacam HR | 11 | 24 (20-30) | Sphere: (0.25 – +0.50) | After -5 D: -0.14 ± 0.05 | - | - |
| Cylinder: (-0.25 – 0.00) | |||||||
| Read et al.(23) | Lenstar | 19 emmetropic | 25 ± 4 (18-33) | -0.05 ± 0.27 | After -3 D: -0.10 ± 0.09 | - | - |
| After -6 D: -0.30 ± 0.14 | |||||||
| 21 myopic | -1.82 ± 0.84 | After -3 D: -0.14 ± 0.11 | - | - | |||
| After -6 D: -0.29 ± 0.14 | |||||||
| Ruggeri et al.(24) | OCT | 2 | 35 | After -4 D: -0.07 | - | - | |
| Tsorbatzoglou et al.(25) | PCI | 32 | (16-30) | -0.05 ± 0.13 | After -4.50 D: -0.08 ± 0.06 | - | - |
| 37 | (31-44) | -0.03 ± 0.32 | After -3.00 D: -0.06 ± 0.09 | - | |||
| 32 | (45-71) | +0.21 ± 0.19 | After -0.50 D: -0.03 ± 0.06 | - | |||
| Yan et al.(26) | OCT | 42 emmetropic | (6-20) | 0 | After maximum amplitude of accommodation: -0.25 ± 0.09 | - | After maximum amplitude of accommodation: -0.95 ± 0.53 |
| 42 myopic | (21-40) | -4.75 - -0.25 | After maximum amplitude of accommodation: -0.15 ± 0.07 | - | After maximum amplitude of accommodation: -0.52 ± 0.37 | ||
| 42 hyperopic | (41-60) | +0.25 - +1.75 | After maximum amplitude of accommodation: -0.06 ± 0.04 | - | After maximum amplitude of accommodation: -0.26 ± 0.25 | ||
| Yuan et al.(27) | OCT | 20 | 33.1 ± 5.8 | -2.76 ± 2.61 (-6.88-0.00) | After maximal accommodation ~ -0.05 | - | After maximal accommodation ~ 0.65 |
| Zhou et al.(28) | OCT | 1 | 37 | -3.5 | After -2 D: -0.02 | - | - |
| After -5.50 D: -0.13 | |||||||
| Charman et al.(29) | Hartmann-Shack | 20 emmetropic | 25.30 ± 5.70 | -0.07 ± 0.26 (-0.50 – +0-50) | - | - | After -1 D: -0.21 ± 0.15 |
| 20 myopic | 23.10 ± 4.50 | -3.06 ± 2.35 (-8.45 – -0.60) | - | - | After -1 D: -0.31 ± 0.29 |
SD= standard deviation; AC-OCT= anterior chamber optical coherence tomography; AC= anterior chamber; UBM= ultrasound biomicroscopy; UL-OCT= ultralong scan depth optical coherence tomography; MRI= magnetic resonance imaging; HR-OCT= high-resolution optical coherence tomography; AS-OCT= anterior segment optical coherence tomography; SD-OCT= Spectral domain optical coherence tomography; SL-OCT= Slit lamp optical coherence tomography; PCI= Partial coherence interferometry.
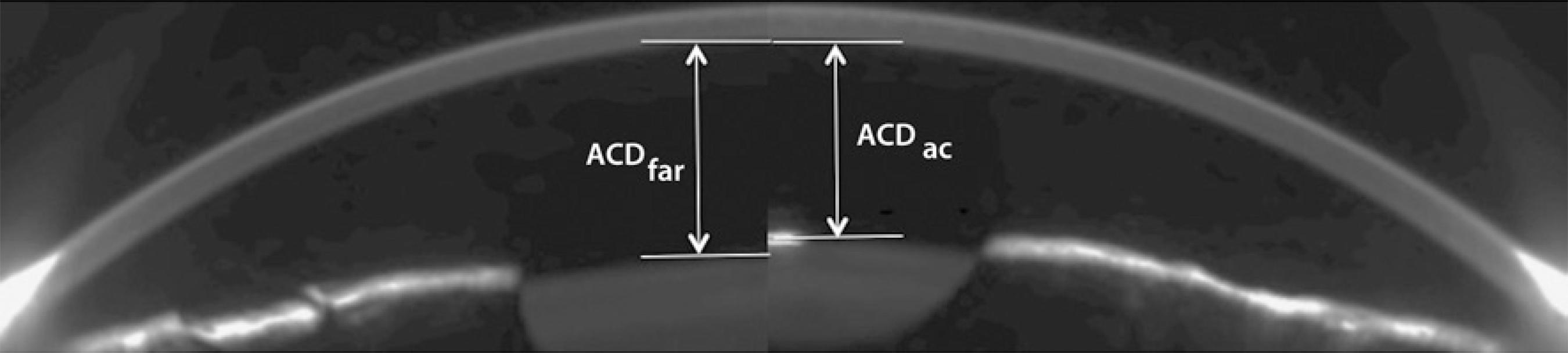
Figure 1 Scheimpflug images obtained with the measuring device, which combines a rotating Dual Scheimpflug and a Placido disc system (Galilei G4, Ziemer Ophthalmic Systems AG, Switzerland). The images represent changes in the anterior chamber depth (ACD) for far vision and after -4 Diopters of accommodation in the same subject. ACDac represents the central ACD during accommodation. ACDfar represents the central ACD for far vision.
The changes in the peripheral ACD and ACA at different meridians during accommodation have not been studied. Quantifying the possible position-related changes in ACD could enable the development of new intraocular lenses (IOL) that preserve the anatomical structures (corneal endothelium, iris, or crystalline lens). Reports of studies assessing the changes in ACA along the horizontal and vertical meridians during accommodation are limited(16). Further, no previous studies assessed the possible changes in ACA during accommodation in young population. Such studies will enable the development of new anterior chamber IOLs that better fits the anterior chamber eye. Several studies have evaluated the changes in pupil diameter during accommodation(3,7,26,28,29). However, four of these studies(3,7,26,28) included myopic or hyperopic subjects and measured the changes in pupil diameter with stimuli vergences beyond 5 D. Further, a Scheimpflug system has not been used to study the changes in pupil that occur during accommodation.
The aim of the present study was to evaluate the changes in ACD, ACA, and PD during accommodation. For this purpose the rotating Dual Scheimpflug and a Placido disc system (Galilei G4, Ziemer Ophthalmic Systems AG, Switzerland) was chosen as a measuring devices. To our knowledge, this is the first comprehensive study that evaluated all of these ocular metrics during accommodation.
METHODS
Study cohort
Eighty right eyes from eighty subjects (39 men and 41 women), whose ages ranged from 20 to 40 years (mean ± standard deviation = 30.36 ± 7.32 years), with a mean spherical equivalent of 0.80 ± 0.73 diopters (D) were included in the study. All patients were informed of the details of this study and a written informed consent was obtained in accordance with the Helsinki Declaration. An Institutional Review Board approval was not required for this study. Subjects with best-corrected visual acuity below than 20/40, ocular or systemic disease, history of ocular surgery, intraocular pressure above 21 mmHg, or retinal or optic disk pathology were excluded from the study.
Measuring device and study Metrics
Measuring device
The rotating Dual Scheimpflug and a Placido disc system (Galilei G4, Ziemer Ophthalmic Systems AG, Switzerland) (Figure 2) is one of the latest versions of the Galilei topographer. This device integrated both the Placido and rotated Dual Scheimpflug images to generate a three-dimensional model of the anterior eye segment. This device also recorded images of the cornea, iris, pupil, limbus, anterior chamber, and the lens. Additionally, the Galilei G4 has a red-LED near/far adjustable fixation target, which can be moved in 0.25-D steps from -20 D to +20 D.
Eye metrics
The Galilei G4 was used to record the central and peripheral ACD, mean ACA of the whole eye, local ACA, and the PD. These eye metrics were measured for far, intermediate, and near vision. The central ACD was measured automatically as the distance between the corneal endothelium and the anterior surface of the crystalline lens. The peripheral ACD was measured 4 mm away from the corneal centre, and was defined as the distance between the corneal endothelium and the iris. This eye metric, which had a resolution of 0.01 mm, was measured manually from the Scheimpflug images at 0 degrees (to measure nasal and temporal ACD) and at 90 degrees (to measure superior and inferior ACD). The ACA was measured automatically as the intersection between the posterior corneal surface and the iris, with a resolution of 0.1 degrees. The ACA of the whole eye was calculated as the average value generated from the 3-D model. This eye metric was also measured individually at the nasal, temporal, superior, and inferior positions. Finally, the PD was computed as the diameter of the best-fit circle for the central image, with a resolution of 0.01 mm.
Experimental procedure
Before each measurement, the central Placido rings were focused and the instrument was aligned. Following this, a volunteer was requested to blink and look at the fixation target for 2 seconds to get an appropriate accommodation response(30). Then, to avoid distortion, the subject was requested to not to blink during the measurement. To ensure that all measurements were made under the same lighting conditions, the experiments were performed in dark.
The ACD, ACA, and PD were measured for a viewing distance that ranged from +1 D to -4 D, in 1-D steps. Far, intermediate, and near vision ranged from +1 D to 0 D, -1 D to -2 D, and -3 D to -4 D, respectively. These parameters were used so as to study the changes in the anterior eye segment during the most common accommodative effort. Three measurements were made for each accommodation stimuli and the average value was retained. A single specialist, who had prior experience operating this device and who also was not aware of the study's goal, carried out all experiments. For each subject, all measurements were made within a single session.
Statistical analysis
SigmaPlot for Windows version 11 (Systat Software, Inc.) was used for the statistical analysis of the data. Since the main goal was to compare the values obtained under different conditions such as accommodative stimulus and anatomical location, the study had a factorial design. Therefore, once the normality assumption was confirmed using the Shapiro-Wilk test, the repeated-Measures ANOVA was chosen as the most suitable test. The Post-Hoc multiple-comparison test by means of the Holm Sidak method was then performed in those cases where the ANOVA revealed differences. The threshold of statistical significance was set at P=0.05.
For ACD, a Two-Way Analysis of Variance was performed, whose two factors were "accommodative stimulus" and "location". For the analysis of the pupil size and mean ACA, the One-Way Analysis of Variance was chosen, with "accommodative stimulus" as its main factor. Finally, for location-dependent ACA, the Two-Way Analysis of Variance was used, with "location" and "accommodative stimulus" as the two factors.
RESULTS
Anterior chamber depth
Table 2 summarizes the ACD values for each accommodation stimuli and position. The percentage of relative change between far and near vision was -4.11%, 7.57%, -2.11%, 7.56%, and -0.51% for central, superior, inferior, nasal, and temporal ACD, respectively, where the negative values indicate a decrease in the ACD and the positive values suggest an increase in ACD. No statistical significant differences were observed in this eye metric among far vision and each accommodation stimuli.
Table 2 Mean anterior chamber depth (ACD), anterior chamber angle (ACA), and pupil diameter (PD) for far (0 D) and near vision (-4 D) ACD and pupil diameter are expressed in mm and ACA in degrees
| Anterior chamber depth | Anterior chamber angle | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Central | Superior | Inferior | Nasal | Temporal | Mean | Superior | Inferior | Nasal | Temporal | Mean | ||
| 0 D | 3.07 ± 0.08 | 1.58 ± 0.11 | 1.79 ± 0.12 | 1.43 ± 0.09 | 1.97 ± 0.09 | 34.72 ± 2.48 | 33.47 ± 0.95 | 36.18 ± 0.84 | 34.32 ± 0.96 | 36.49 ± 0.82 | 3.08 ± 0.16 | |
| -1 D | 3.05 ± 0.08 | 1.64 ± 0.11 | 1.76 ± 0.11 | 1.49 ± 0.11 | 2.08 ± 0.10 | 34.73 ± 1.77 | 33.92 ± 0.67 | 36.75 ± 1.04 | 33.94 ± 0.75 | 36.60 ± 0.68 | 2.91 ± 0.15 | |
| -2 D | 3.02 ± 0.08 | 1.57 ± 0.09 | 1.82 ± 0.13 | 1.53 ± 0.11 | 2.06 ± 0.11 | 34.46 ± 1.91 | 33.79 ± 0.64 | 36.52 ± 0.79 | 33.62 ± 0.68 | 35.82 ± 0.59 | 2.90 ± 0.11 | |
| -3 D | 2.94 ± 0.07 | 1.57 ± 0.10 | 1.84 ± 0.12 | 1.52 ± 0.09 | 2.06 ± 0.11 | 33.77 ± 1.98 | 33.00 ± 0.83 | 34.72 ± 0.66 | 33.86 ± 0.53 | 34.29 ± 1.24 | 2.84 ± 0.11 | |
| -4 D | 2.95 ± 0.07 | 1.68 ± 0.11 | 1.73 ± 0.11 | 1.53 ± 0.11 | 1.96 ± 0.11 | 33.36 ± 1.58 | 31.72 ± 0.56 | 34.24 ± 0.36 | 32.57 ± 1.10 | 35.00 ± 0.49 | 2.75 ± 0.11 | |
The highest ACD was obtained at the central position. The quadrant nasal-superior was significantly shallower than the temporal-inferior quadrant. Further, comparable values were obtained between each pair (nasal-superior, and temporal-inferior). This behaviour was also observed at far and near vision.
Anterior chamber angle
Table 2 summarizes the ACA values for each accommodation-stimuli and position. The percentage of relative change in ACA between far and near visions was -4.55%, -3.72%, -4.71%, -5.07% and -3.73% for nasal, temporal, superior, inferior, and mean ACA, respectively. Whereas the mean ACA at the nasal position and of the whole eye did not vary significantly with accommodation, significant variation was observed in other positions. A significant reduction in ACA at temporal position was obtained among -3.00 D and -1.00 D and 0 D; among -4.00 D and -1.00 D and -2.00 D at superior position, and among -4.00 D and 0.00 D, -1.00 D and -2.00 D at the inferior position.
The nasal-superior quadrant had significantly lower ACA than the temporal-inferior quadrant. Further, comparable ACA was obtained between each pair (nasal-superior and temporal-Inferior).
Pupil Diameter
Table 2 also highlights the absolute PD with accommodation. The PD was reduced -8.31% between far and near visions, and the difference became significant between -4.00 D and -3.00 D and between -1.00 D and -4.00 D.
DISCUSSION
The objective of the present study was to assess the changes in ACD, ACA and, PD during accommodation.
Anterior chamber depth
The central ACD did not change significantly (P>0.05) with accommodation, the mean change between far and near vision being 0.13 ± 0.13 mm. A number of studies (Table 1) have assessed the changes in central ACD during accommodation. Our results are in agreement with those found previously in emmetropic volunteers(4,15,17,18,22,23,25,26). Bolz et al.(4), who used partial coherence interferometry, found a relative ACD decrease of 4.92% after -4.00 D of vergence. Mallen et al.(15) studied the changes in ACD during accommodation using the IOLMaster. The ACD obtained after -6 D accommodation was 5% shallower than that measured for far vision. Malyugin et al.(17), Read et al.(23), and Tsorbatzoglou et al.(25) studied changes in ACD after -3.00 D of accommodation and found that the relative changes were 3.80%, 3.20% and 2.23%, respectively. Finally, Ni et al(18) and Read et al(22) also studied the changes in ACD with accommodation in young eyes with the help of Pentacam HR. After -5 D accommodation, the mean ACD decreased approximately by 0.11 mm and 0.14 mm, respectively.
However, Yan et al.(26) found greater changes than that observed in previous studies. The central ACD decreased by 0.25 ± 0.09 mm. This magnitude of change is approximately 0.12 mm greater than that found in our study. The difference between our results and that of Yan et al.(26) could be due to the stimulus vergence range under analysis. Whereas the highest vergence in our study was -4 D, a vergence was not reported by Yan et al. since these authors used the subject's maximum amplitude of accommodation.
Our results also showed that the ACD is asymmetrical along the eye (Table 2), where the quadrant superior-nasal was significantly shallower than the quadrant inferior-temporal. These results are in agreement with those reported by Koç et al.(27), who studied the anterior chamber width with the help of a Scheimpflug camera. These authors found that the superior-nasal quadrant was significantly narrower than the inferior-temporal quadrant. However, our results contradict the results of Marigo et al.(31), who used ultrasound biomicroscopy (UBM) for their studies. These authors found that the angle opening distance at 250 and 500 μm from the scleral spur was shallower at the horizontal direction than that in the vertical direction. These differences could be related to the different methodologies used in the studies. It can be concluded that ACD is asymmetrical along the anterior chamber eye. Further studies are needed to clarify these contradictions and to propose safer IOL designs, where thickness should be asymmetrical in order to avoid possible damage in the corneal endothelium.
Anterior chamber angle
The ACA of the whole eye changed during accommodation. The relative decrease in ACA was 3.73%. However, the local ACA varied significantly with accommodation. The highest and lowest relative decreases in the ACA after -4 D of accommodation was 5.07% (at inferior position) and 3.72% (at temporal position), respectively. The superior-nasal ACA was significantly narrower than the temporal-inferior ACA. Therefore, it can be concluded that ACA varies in an asymmetrical manner along the anterior chamber eye. These results are in agreement with those of Koç et al.(27), who studied the ACA width at different quadrants. These authors found that the superior-nasal quadrant was significantly narrower than the temporal-inferior quadrant. Further, these results are in agreement with ACD ones because the nasal-superior ACD was significantly shallower than the temporal-inferior ACD. However, our results contradict those reported by Marigo et al.(31), who found shallower angle opening distance at the horizontal direction than in the vertical direction. As discussed earlier, these discrepancies might be related to the different devices used in these studies. To propose a suitable method for placing an angular support IOL, future studies should clarify the ACA symmetry.
To the best of our knowledge, this is the first report that describes the changes in ACA during accommodation(16) in subjects who underwent IOL implantation and whose mean age was 76 ± 6 years. After 3 D of accommodation, the ACA decreased by approximately 1.22 degrees at the horizontal meridian and by 0.75 degrees in the vertical direction. Considering the mean changes in ACA along the horizontal and vertical directions, the mean ACA were approximately 1.35 and 0.95 degrees, respectively. These values are higher than that reported by Marchini et al. These disagreements could be related to the differences in sample population. We included phakic eyes, whereas Marchini et al. used aphakic eyes with an implanted IOL. Additionally, the mean age of our sample population was 25.30 ± 2.98 years, whereas the mean age of subjects in the study reported by Marchini et al. was 76.60 ± 6.0 years.
Pupil diameter
The mean relative change in PD between far and near vision was 8.31%. Yan et al.(26) measured PD up to the maximum amplitude of accommodation in emmetropic subjects using an SL-OCT system and found that the relative decrease in PD was 20.83%. Yuan et al.(28), who measured the changes in PD during accommodation using a spectral-domain OCT system in myopic subjects, found a relative decrease of 15.80%. The differences between the results of earlier studies and that of the present study are likely due to the different methods of measurements adopted. The earlier studies used the full accommodation interval without specifying the maximum vergence value. Another possible reason for the discrepancies may be the differences in the luminance conditions used in each device.
Using ultralong scan depth optical coherence tomography, Du et al.(7) measured dimensional changes in the anterior segment of human eyes during accommodation. The relative change in the pupil diameter with a maximum accommodation effort of -5 D was 21.74%. The differences between the PD values obtained in the present study and that of Du et al. likely occurred due to the different samples studied. Whereas Du et al. included myopic subjects, the subjects in our study were emmetropic.
Baikoff et al.(4) used anterior-chamber OCT (AC-OCT) to measure variations in PD at -10 D of accommodation in dim light. These authors reported a mean change in PD of 1.5 mm. The differences between our results and those of Baikoff et al. could be related to the different experimental conditions used. Baikoff et al. used -10 D as the maximum accommodation, whereas the maximum accommodation stimulus in our study was -4 D. Chartman et al.(29) studied changes in pupil size during accommodation using a Hartman-Shack wavefront sensor. The mean rate of change in PD during accommodation was -0.21 ± 0.15 mm·D-1. Our results are in agreement with those reported by Chartman et al., as the mean change in PD after -1 D accommodation in our study was 0.16 ± 0.31 mm.
One limitation of our study is that only emmetropic subjects were considered. A second limitation is that all measurements were performed with only one device. Future efforts should focus on studying the changes in the anterior segment during accommodation in myopic and hyperopic subjects using other devices.
In summary, the ACA and PD varied significantly with accommodation, whereas variations in ACD were not observed. The anterior chamber eye was found to be asymmetrical, with the nasal-superior area being significantly shallower than the temporal-inferior area.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

