INTRODUCTION
The measurement of anterior chamber depth (ACD), white-to-white (WTW) distance, and pupil diameter (PD) is an important step prior to any refractive surgery. In this context, the ACD measurement is useful in determining the appropriate phakic or standard intraocular lens (IOL) power, and in predicting the IOL vault prior to its implantation. Furthermore, the WTW distance is useful in determining the optimum IOL size, and the PD is essential in determining the optical zone where the laser pattern has to be applied. Also, an anterior chamber angle (ACA) evaluation is essential to establish the risk of angle disclosure(1). Recent technological advances have allowed the ACD, WTW, PD, and ACA measurements to be quantified with the following non-invasive techniques: Scheimflug photography (Pentacam-Galilei), scanning slit topography (Orbscan/OrbscanII), and partial (IOLMaster) and low coherence interferometry (Visante-optical coherence interferometry and Lenstar). However, invasive techniques such as A-Scan or ultrasound byomicroscopy, are still being used to measure ACD in some cases.
The Pentacam HR (Oculus, Wetzlar, Germany) and the Galilei G4 (Ziemer, Switzerland) are two clinical tomographers that are both based on Scheimpflug cameras. Beside corneal parameters, these devices also have the ability to measure the ACD, ACA, PD, and ACA, and they are now being routinely used in clinical practice. Because of this, we felt that it was important to study the agreement between the Pentacam HR and the Galilei G4 systems regarding ACD, ACA, PD, and ACA measurements. Table 1 shows all previously reported studies that have assessed either the Pentacam/Pentacam HR or the Galilei systems, focusing on measurements of the ACD(1-19) or WTW distance(20-22). Ho wever, to our knowledge, a side by side comparative study has not previously been reported. Regarding PD and ACA measurements, there have been no studies published using either the Pentacam/ Pentacam HR or Galilei/Galilei G4 systems. Recently, Domínguez-Vicent et al.(22), assessed the agreement between the Galilei G4 and the Orbscan II systems in order to measure the angle kappa.
Table 1 Anterior eye results obtained in published peer-reviewed studies
| Mean ACDa | Mean WTWc | ||
|---|---|---|---|
| Reference (no. of eyes) | Device | ± SDb (mm) | ± SD (mm) |
| Savant et ai.(2), (50) | Pentacam | 3.21 ± 0.03 | - |
| IOLMaster | 3.23 ± 0.03 | - | |
| Nemeth G et al.(3), (42) | A-Scan | 2.89 ± 0.49 | - |
| Pentacam | 2.87 ± 0.40 | - | |
| Doors et al.(4), (66) | Orbscan II | 3.25 ± 0.29 | - |
| Pentacam | 3.34 ± 0.27 | - | |
| Visante OCTe | 3.41 ± 0.25 | - | |
| Woodmass et al.(5), (52) | Pentacam | 3.82 ± 0.41 | - |
| IOLMaster | 3.78 ± 0.42 | - | |
| Reuland et al.(6), (82) | Pentacam | 3.25 ± 0.50 | - |
| IOLMaster | 3.20 ± 0.40 | - | |
| Lackner et al.(7), (60) | Orbscan | 3.23 ± 0.40 | - |
| Pentacam | 3.18 ± 0.38 | - | |
| Utine et al.(8), (42) | Orbscan II | 3.49 ± 0.30 | - |
| Pentacam | 3.54 ± 0.31 | - | |
| IOLMaster | 3.43 ± 0.29 | - | |
| Dinc et al.(9), (80) | Orbscan II | 2.80 ± 0.29 | - |
| Pentacam | 2.93 ± 0.30 | - | |
| Visante OCTe | 2.98 ± 0.29 | - | |
| IOLMaster | 3.33 ± 0.42 | - | |
| Elbaz et al.(10), (22) | A-Scan | 3.00 ± 0.37 | - |
| Pentacam | 3.08 ± 0.38 | - | |
| IOLMaster | 2.99 ± 0.37 | - | |
| Szalai et al.(11), (46) | A-Scan | 3.08 ± 0.43 | - |
| Pentacam HR | 2.89 ± 0.41 | - | |
| Yazici et al.(12), (100) | Orbscan | 2.84 ± 0.33 | - |
| Pentacam | 2.98 ± 0.33 | - | |
| Visante OCTe | 2.94 ± 0.34 | - | |
| Salouti et al.(13), (74) | Orbscan II | 3.54 ± 0.07 | - |
| Pentacam HR | 3.25 ± 0.05 | - | |
| Galilei | 3.22 ± 0.05 | - | |
| Hashemi et al.(14), (46) | Orbscan II | 3.10 ± 0.33 | - |
| Pentacam | 3.26 ± 0.34 | - | |
| Kim et al.(15), (51) | Orbscan II | 3.09 ± 0.28 | - |
| Pentacam | 3.23 ± 0.33 | - | |
| O'Donnell et al.(16), (17) | Pentacam | 2.96 ± 0.32 | - |
| Visante OCT | 3.03 ± 0.29 | - | |
| Lenstar | 2.93 ± 0.30 | - | |
| Huang et al.(17), (108) | Pentacam | 3.78 ± 0.25 | - |
| Lenstar | 3.76 ± 0.24 | - | |
| Németh et al.(18), (83) | Pentacam HR | 3.01 ± 0.34 | - |
| IOLMaster | 2.95 ± 0.32 | - | |
| Aramberri et al.(19), (35) | Pentacam HR | 3.04 ± 0.33 | - |
| Galilei | 3.14 ± 0.32 | - | |
| Salouti et al.(20), (37) | Orbscan II | - | 11.67 ± 0.29 |
| Galilei | - | 12.01 ± 0.61 | |
| EyeSys | - | 12.09 ± 0.87 | |
| Kim et al.(21), (20) | Orbscan II | - | 11.56 ± 0.41 |
| Pentacam | - | 11.86 ± 0.45 | |
| Visante OCT | - | 11.70 ± 0.47 |
a= anterior chamber depth (ACD)
b= standard deviation (SD)
c= white-to-white (WTW) distance
d= pupil diameter (PD)
e= optical coherence tomography (OCT).
Thus, the aim of this study was to compare the ACD, WTW, PD, and ACA measurements obtained using a double-Scheimpflug camera (Galilei G4) and a single-Scheimpflug camera (Pentacam HR) in order to determine whether these devices can be used interchangeably in clinical practice.
METHODS
Subjects
This transversal study comprised 80 right eyes from 80 subjects (39 men and 41 women), whose ages ranged from 20 to 40 years (mean ± standard deviation: 30.36 ± 7.32 years). Their spherical equivalent (SE) ranged from -4.25 to +1.00 diopters (D) (mean: -0.80 ± 2.33 D). Subjects with a best-corrected visual acuity below 20/25, ocular or systemic disease, a history of ocular surgery, intraocular pressure above 21 mmHg, or the presence of retinal or optic disk pathology, were excluded from taking part in the study.
Informed consent was obtained from each participant following a verbal and written explanation of the nature and possible consequences of the study. Moreover, this study followed the tenets of the Declaration of Helsinki.
Devices used
Galilei G4
The Galilei G4 system is a recent version of the Galilei topographer. This non-invasive optical diagnostic device was designed for the assessment of the eye's anterior segment. It is based on a rotating dual-Scheimpflug camera and a Placido topography system. The images recorded by this device include the cornea, iris, pupil, limbus, anterior chamber, and lens. After each standard 3D scan, this device integrates the Placido and Scheimpflug images in order to generate a 3 D model of the anterior segment. Moreover, this device also includes a LED near/far adjustable fixation target which can be moved in steps of 0.25 D from -20 D to +20 D.
The Galilei G4 was used to automatically measure the ACD, WTW distance, mean ACA, and PD for far vision. The central ACD was calculated as the distance between the corneal endothelium and the crystalline lens' anterior surface, with a resolution of 0.01 mm. The limbus was fitted to a best-fit ellipse in the top reference image and the WTW distance was then measured as the maximum length in the horizontal direction of the ellipse, also with a resolution of 0.01 mm. Regarding the ACA measurements, these were done by extrapolating the posterior corneal surface and the smoothed surface of the iris, to the point where both curves intersected. This angle of intersection was taken as the ACA, with a resolution of 0.10 degrees. Finally, the PD was fitted to a best-fit circle in the reference top view image.
Pentacam HR
The Pentacam HR is a non-invasive tomographer that is based on a rotating simple Scheimpflug system. The camera revolves around the optical axes of the eye, to calculate a 3 D model of the anterior segment. The internal software creates a 3 D reconstruction of the anterior segment using the elevation data contained in these images, thus providing information about both the anterior and the posterior surface of the cornea, crystalline lens, and anterior chamber. The device has a red light source that serves as a fixation target, and which can be moved in 0.5 D steps from + 2 D-5 D.
The Pentacam HR was also used to automatically measure the central ACD, WTW distance, ACA, and PD, all for far vision. The central ACD was calculated as the distance between the corneal endothelium and the crystalline lens' anterior surface, with a resolution of 0.01 mm. The WTW distance was calculated automatically from the iris photo, with a resolution of 0.10 mm. The ACA was calculated from the reconstructed anterior segment image, using the angle intersection between the posterior corneal surface and iris, with a resolution of 0.10 degrees. Finally, the PD was calculated as the mean value of the measurement procedure, with a resolution of 0.01 mm.
Experimental procedure
Each eye's ACD, WTW distance, ACA, and PD, were measured three times with each device under far-viewing conditions, and an average value was obtained. The order in which these two devices were used was randomized and for each subject and all measurements were performed within a single session. In order to avoid any possible bias related to differences in luminance conditions, both devices were placed in the same room, which remained in complete darkness during the measurements. Moreover, black fabric was placed over both the instrument and the subject in order to avoid any luminance emanating from the computer or any other source. The same specialist, who had experience operating both devices and who was not aware of the study goals, carried out all the experimental measures.
Statistical analysis
Statistical analysis was performed by means of the SPSS statistical software package SPSS/Pc + 10.1 for Windows (SPSS, Chicago, Illinois, USA). A Student's t-test for unpaired data was used to compare the differences in ACD, WTW, ACA, and PD measurements between the Galilei G4 and the Pentacam HR. Differences were considered to be statistically significant when P<0.05. To assess inter-device agreements and their interchangeability for the measurement of anterior eye distances, the method described by Bland and Altman for repeated measurements was used(23). The 95% limits of agreement were computed as the mean difference of ± 1.96 SD.
RESULTS
Anterior chamber depth
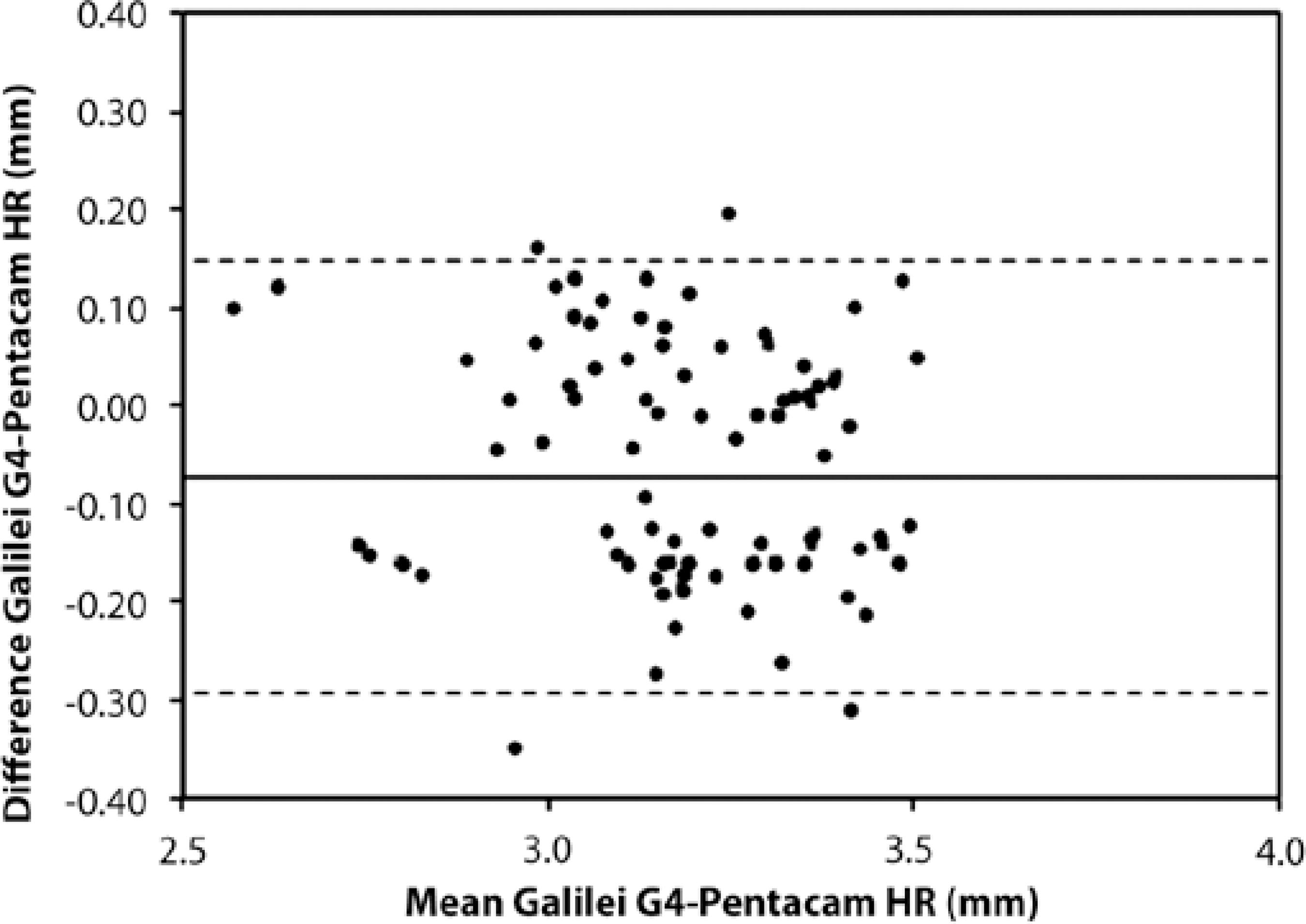
Results revealed that the Pentacam HR yielded significantly larger ACD measurements than the Galilei G4 (P<0.05), with the mean difference being -0.07 ± 0.11 mm (Table 2). Regarding the device agreements, figure 1 shows Bland-Altman plots that represent the difference between both devices against their mean. It can be seen that although the mean ACD difference was close to zero, the spread was highly variable. The 95% limit of agreement was within 0.43 mm.
Table 2 Mean anterior eye distances (expressed mean ± standard deviation (SD), mean differences, SD, and limits of agreement obtained for the Galilei G4 and Pentacam HR systems for all anterior eye distances
| Galilei G4 | Pentacam HR | P | Mean difference ± SD | 95% Limits of agreement | |
|---|---|---|---|---|---|
| Anterior chamber depth (mm) | 3.12 ± 0.23 | 3.19 ± 0.24 | <0.05 | -0.07 ± 0.11 | -0.29 to 0.14 |
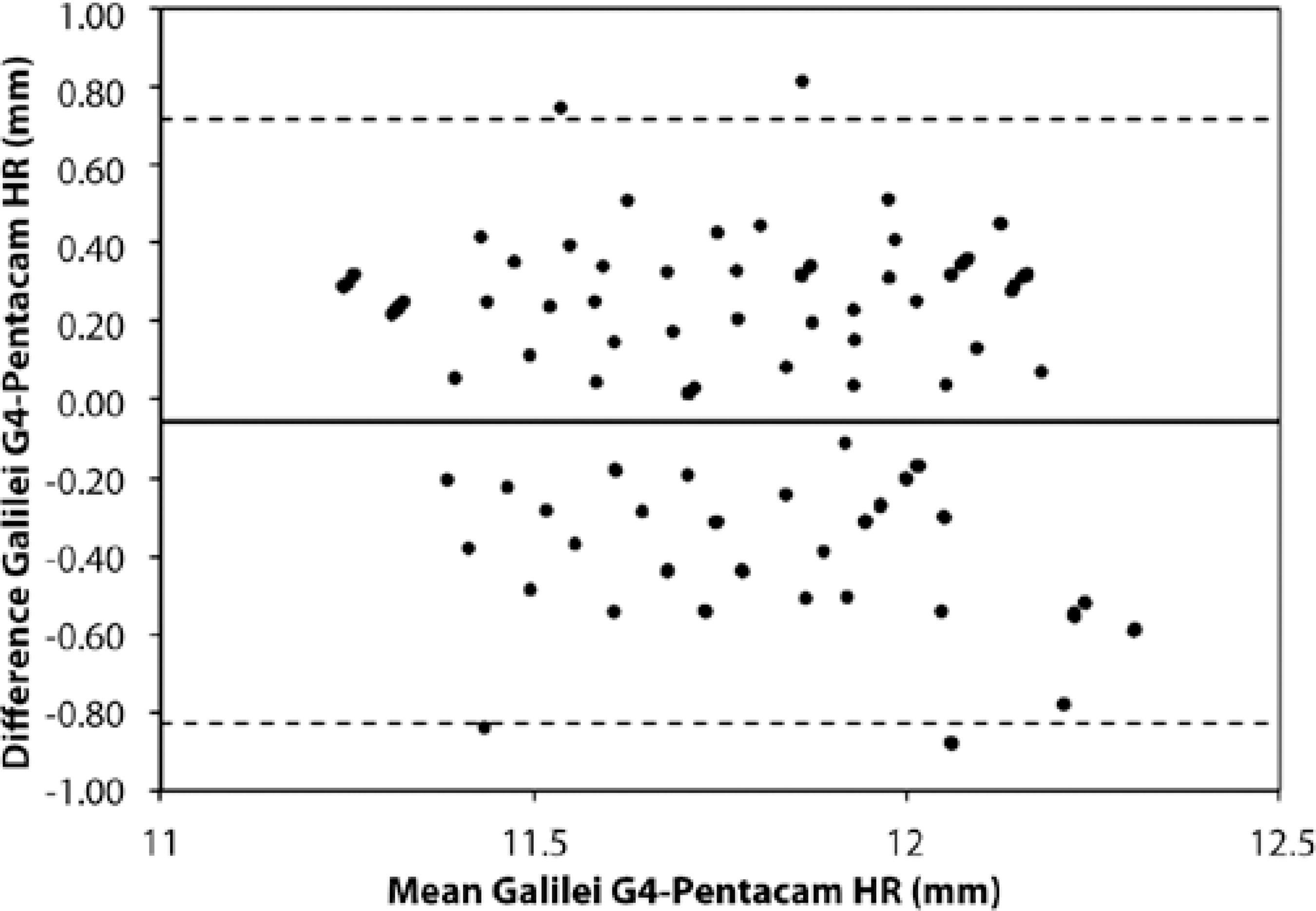
| White-to-white distance (mm) | 11.84 ± 0.31 | 11.90 ± 0.43 | >0.05 | -0.05 ± 0.39 | -0.82 to 0.71 |
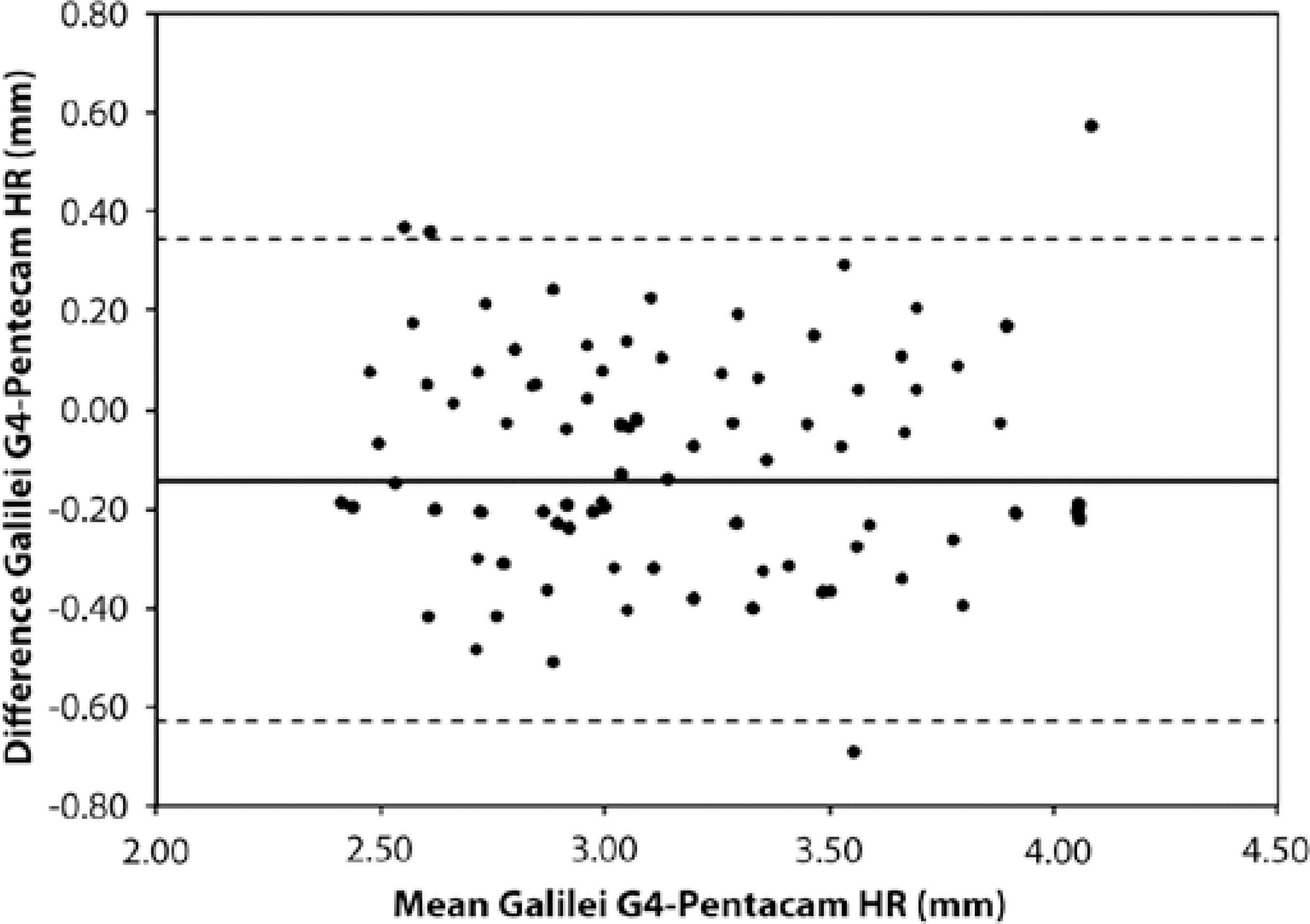
| Pupil diameter (mm) | 3.22 ± 0.58 | 3.22 ± 0.52 | <0.05 | -0.14 ± 0.24 | -0.63 to 0.34 |
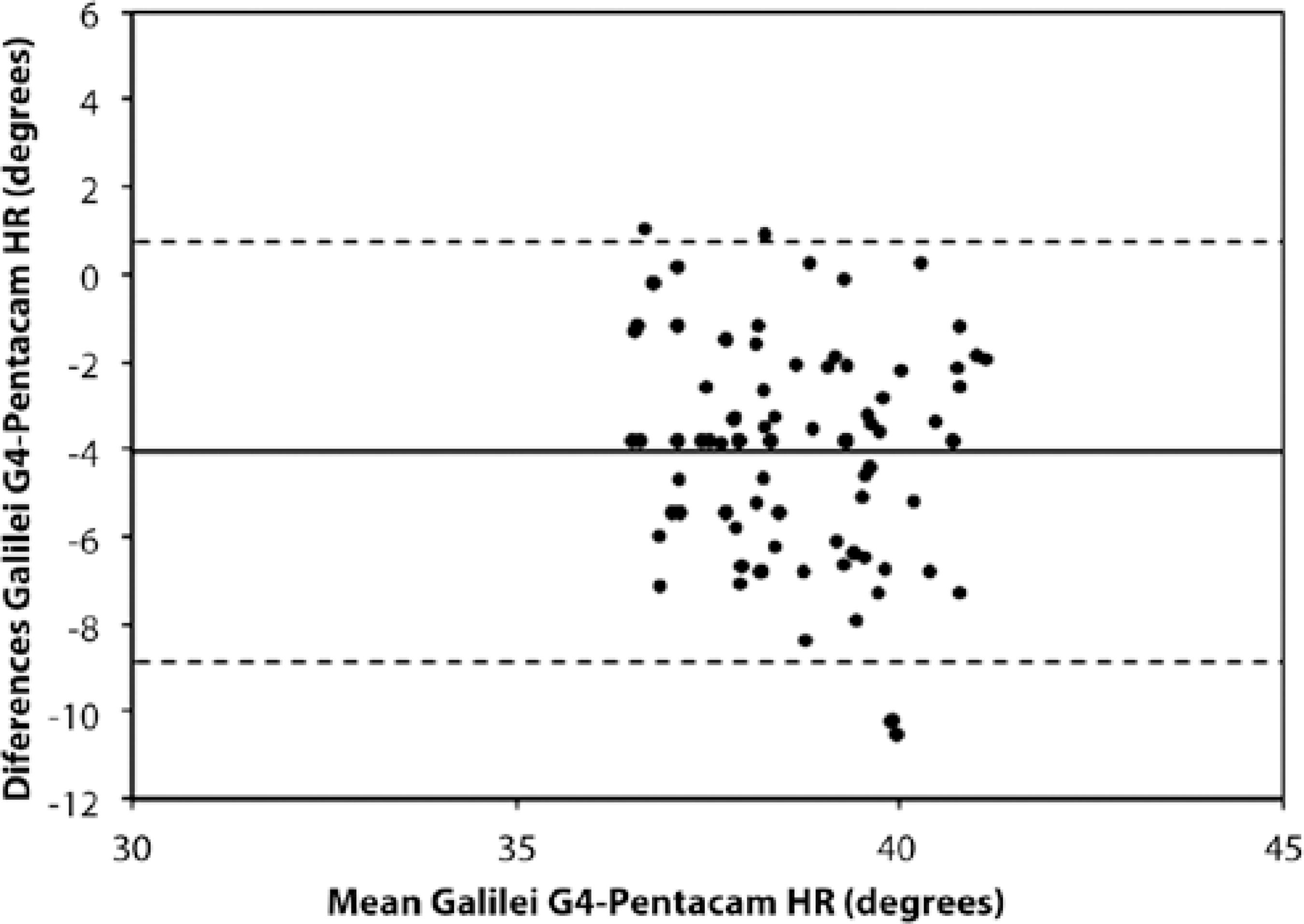
| Anterior chamber angle (degrees) | 34.30 ± 2.86 | 39.26 ± 2.85 | <0.05 | -4.05 ± 2.45 | -8.86 to 0.74 |
White-to-white distance
Results revealed no statistical difference between the two systems regarding WTW distances (P>0.05), with the mean difference being -0.05 ± 0.39 mm (Table 2). However, the wide spread values inferred from figure 2, and the wide 95% limits of agreement, revealed poor agreement between the device measures.
Pupil diameter
Results showed that the Pentacam HR produced significantly higher PD measurements than the Galilei G4, with the mean difference being - 0.14 ± 0.24 mm (Table 2). The inter-device comparison (Figure 3) showed a high variability on the anterior eye measurement (the limit of agreement was within 0.43 mm), despite its mean difference being close to zero.
Anterior chamber angle
Results revealed that the Pentacam HR produced significantly higher ACA values than the Galilei G4 (P<0.05), with the mean difference being 4.05 ± 2.45 degrees (Table 2). A Bland-Altman comparison (Figure 4) revealed a wide limit of agreement (9.60 degrees) and high spread values.
DISCUSSION
The aim of the present work was to compare the ACD, WTW distance, PD, and ACA values obtained by the Galilei G4 and the Pentacam HR systems, so as to elucidate whether or not these devices can be considered to be interchangeable in clinical practice when it comes to measuring these parameters.
Anterior chamber depth
The Galilei G4 produced significantly lower ACD measurements than the Pentacam HR, the mean difference being 0.07 ± 0.11 mm. Based on the limits of agreement analysis, there is a 95% chance that the Pentacam HR will measure the ACD between 0.14 mm shallower and 0.29 mm deeper than the Galilei G4. This range is large enough to create damage(24) related to the IOL vault. However, this range is not clinically relevant to the IOL power calculation (IOL power varies by 0.05 D for each 0.10 mm of ACD(25)). Consequently, it can be concluded that these devices can be used interchangeably to calculate IOL power, but not to predict the IOL vault.
These results agree with previously published studies(14,19). Salouti et al.(13), compared the ACD measurements from volunteers using the Galilei and Pentacam HR systems, concluding that the differences between these devices were within clinically acceptable levels (the highest mean difference and limits of agreement widths being 0.02 ± 0.01 mm and 0.23 mm, respectively). However, Aramberri et al.(19), concluded that single and dual Scheimpflug camera systems produced significantly different ACD measurements, with the mean difference and confidence interval being 0.10 ± 0.05 mm and 0.04 mm, respectively. Thus, further studies are required in order to clarify which Scheimpflug device (Pentacam HR or Galilei G4) measures the ACD at a shallower or deeper level. Despite these differences in results, the differences between the devices were not significant from a clinical point of view regarding IOL power assessment.
White-to-white distance
The mean WTW distances measured in our study with the Galilei G4 and the Pentacam HR were 11.84 ± 0.31 mm and 11.90 ± 0.43 mm, respectively (mean difference: 0.05 ± 0.39 mm). Regarding the device comparison, the Bland-Altman plot revealed that there is a 95% chance that the Pentacam HR will measure the ACD between 0.71 mm shorter and 0.82 mm longer than the Galilei G4. Although comparable results were obtained between these devices, they are significant from a clinical point of view. Thus, it can be concluded that these devices cannot be used interchangeably to measure this distance.
Pupil diameter
To our knowledge, there has only been one previously published study regarding the measurement of the PD with a non-invasive anterior segment device(26). In this case two infrared pupillometers were compared with the OrbscanII and two aberrometers (Table 1 summarizes their results). We found lower PD values than the previously reported study, with a mean difference of approximately 3.00 mm. These differences could be due to the different illumination systems used in the studies: infrared light below 1 lux was used for the pupillometers and visible light was used in our study. However, similar results were obtained regarding pupil diameters measured with the Orbscan II(26) and those obtained in the present study.
Our results showed that the Pentacam HR measured significantly higher PD values than the Galilei G4 (means of 3.13 ± 0.52 mm and 3.22 ± 0.58 mm, respectively). The device comparison revealed that there was a 95% chance that the Pentacam HR would measure the PD between 0.34 mm shorter and 0.63 mm longer than the Galilei G4. These differences are significant from a clinical point of view regarding the IOL's optic zone(24).
Anterior chamber angle
In terms of the ACA, our study revealed a statistically significant difference between the Pentacam HR (mean: 39.26 ± 2.85 degrees) and the GalileiG4 (mean: 34.30 ± 2.86 degrees) measurements, with the mean difference being 4.05 ± 2.45 degrees. These measurements are in close agreement with those obtained by Leung et al.(27), where the trabecular iris angle was measured using slit-lamp OCT (SL-OCT) and the Visante OCT system. In this study the mean ACA measured with the SL-OCT and the Visante OCT was approximately 39.20 and 38.85 degrees, respectively.
Our results revealed that the Pentacam HR produced significantly higher ACA values than the Galilei G4. The Bland-Altman analysis revealed a 95% chance that the Pentacam HR would measure the ACD between 0.74 degrees lower and 8.86 degrees higher than the Galilei G4. These values are significant from a clinical point of view. Thus, it can be concluded that the two devices cannot be used interchangeably to measure the ACA.
We therefore conclude that the Galilei G4 and Pentacam HR systems cannot be used interchangeably in clinical practice when used to measure the ACD (especially when it comes to assessing the IOL vault), WTW distance, PD, and ACA due to their poor measurement agreements. Finally, it is worth mentioning that there were several limiting factors in this study: first, only two anterior segment tomographers (Pentacam HR and Galilei G4) were included; second, the participants' ages ranged between 20 and 40 years; and finally, only normal corneas of healthy subjects were included. Further studies should attempt to include additional anterior chamber measuring devices, an extended age range, and study the agreement between these devices in postoperative corneas, and in those with defined pathologies.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

