INTRODUCTION
Incontinentia pigmenti (IP), also known as Bloch-Suzlberger syndrome, is a rare familial disorder affecting the ectodermal structures, with various dermatological, dental, ocular, and neurological features. It is inherited as an X-linked dominant condition and is fatal in males(1).
Diagnosis is made on the basis of skin biopsy. According to Carney(2), dental abnormalities occur in 65% patients, neurological abnormalities in 30%, and ocular manifestations in 35%. Retinal lesions such as ischemia and new vessel proliferation are the most characteristic ocular findings(3).
This paper describes the cases of two young girls with incontinentia pigmenti who were histopathologically diagnosed via skin biopsy and were followed-up for 5 years and >20 years, respectively.
CASE REPORTS
Case 1
A 4-year-old female presented with total hyphema in the right eye following unsuccessful cataract surgery in 1990. Ultrasound revealed complete retinal detachment. Pars plana vitrectomy was performed, albeit with little success, and phthisis developed within a few months. Upon examination, her other eye exhibited lens opacity, an attached retina with some pigment clumping, and a small amount of fibrosis over the macula (Figure 1). The best-corrected visual acuity was 20/400. Her past medical history revealed a cutaneous rash during the neonatal period and 3 seizures in the past year. She was also being treated for dental abnormalities. A clinical diagnosis of incontinentia pigmenti was confirmed by skin biopsy. During the follow-up period, myopia increased to -9.00 in the left eye. In 2007, at the age of 21, she developed a cataract and underwent phacoemulsification and IOL implantation. Her best-corrected visual acuity was restored to 20/400 and has been maintained since then.
Case 2
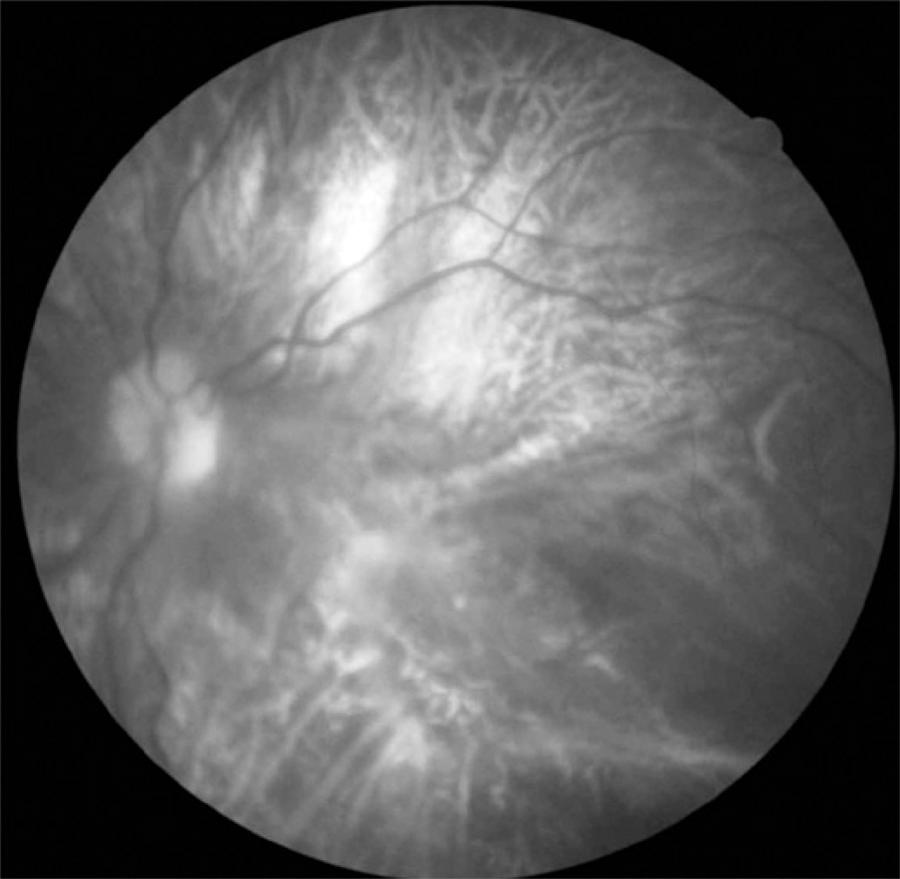
A 5-year-old girl presented with pain, hyperemia, and no light perception in the left eye in 2008. The intraocular pressure (IOP) in the affected eye was 47 mmHg. Ultrasound examination revealed fibrotic tissue extending from the posterior aspect of the lens to the optic nerve. The initial diagnosis was persistent hyperplastic primary vitreous (PHPV), although closed funnel retinal detachment could not be ruled out. The patient received medical treatment for the increased IOP and developed total hyphema 2 months later. The IOP decreased dramatically to 4 mmHg, and the condition of her left eye progressed to phthisis within a month. The best-corrected visual acuity in the fellow eye was 20/25. In 2010, her myopia increased to -4.00, and during retinal examination, an area of nonperfusion with new vessels was observed in the temporal peripheral retina (Figure 2). Her past medical history revealed a cutaneous rash during the neonatal period, which left pigmented lesions on the abdomen. Dental abnormalities were observed, including 12 missing teeth. Skin biopsy revealed an epidermis with hypopigmentation and a decreased melanocyte count, necrotic keratinocytes, and acanthosis. The dermis appeared thickened with a discrete inflammatory infiltrate and melanophages. Focal areas of degeneration of the basal lamina were present.
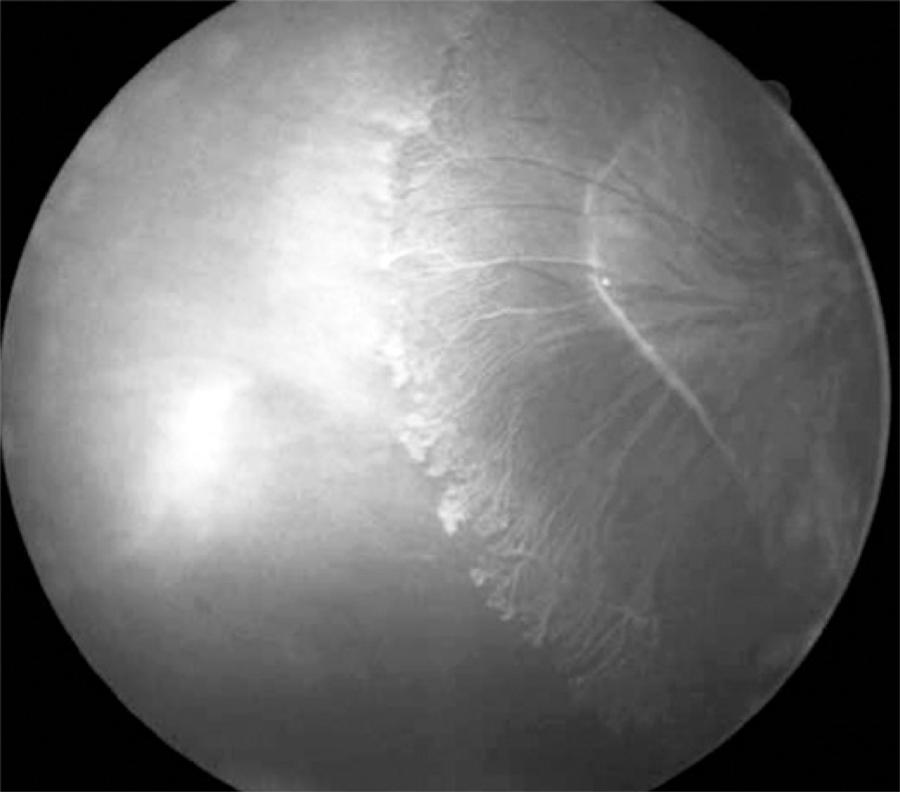
Figure 2 Case 2, right eye, pre-treatment. Fluorescein angiography showing an extensive area of nonperfused retina in the temporal periphery, along with fibrosis and new vessel formation.
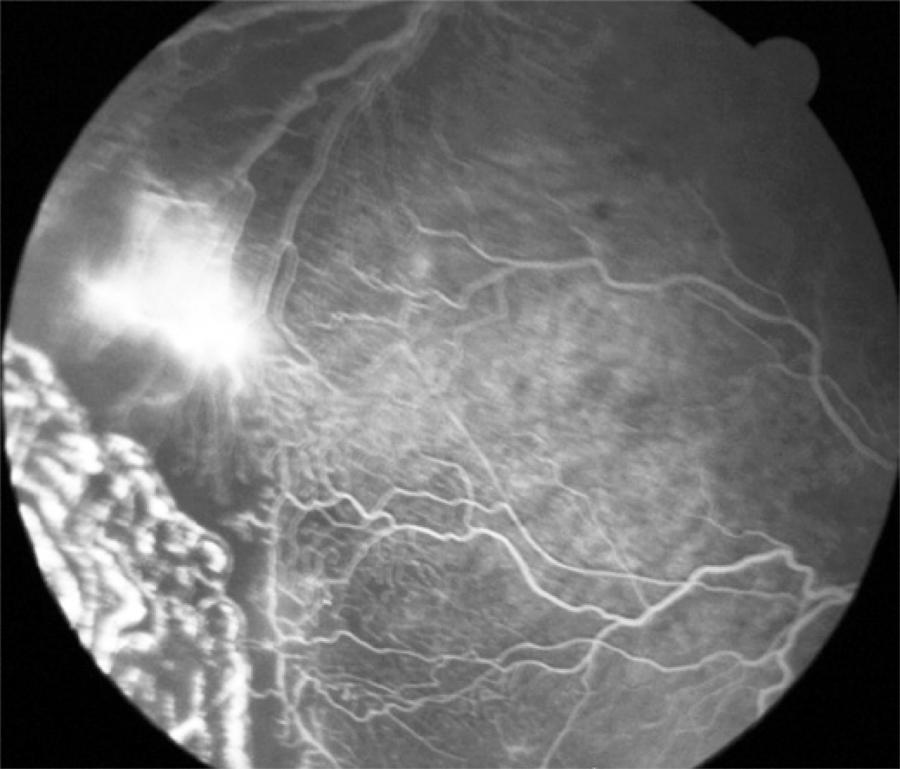
The non-perfused retina of the left eye was subjected to laser therapy. Six months later, fluorescein angiography revealed only a few leaking vessels and a stable retina (Figure 3). Her best-corrected visual acuity at the last follow-up in April 2013 was 20/20 in the left eye.
DISCUSSION
Although ocular manifestations of IP are reported in 35% patients(2), they may be more frequent than previously believed because of undiagnosed ocular changes in many patients. Holmstrom and Thoren(1) reported ocular findings in 77% patients in their series of 30 patients. These authors identified two groups of patients: one with serious manifestations (43% patients) and one with minor ocular changes. The serious ocular findings included retinal detachment, phthisis, retinal ridges with dragged retina, macular fibrosis, cataract, and severe myopia. Asymmetric ocular findings were present in all patients in this group.
Asymmetry was an important feature in both our patients. Both girls had a serious ocular problem in one eye, leading to complete loss of vision and phthisis. It is noteworthy that in both patients, IP was not diagnosed before the ocular problems.
According to a study by O'Doherty et al.(4), who studied 19 patients with IP, the mean age at the first eye examination was 8 years. Our patients were 4 and 5 years old, respectively, at the first ophthalmic evaluation. Such findings may indicate that the diagnosis of IP is overlooked in the neonatal period, that there may be little awareness of this diagnosis, and that the ocular manifestations of IP is given insufficient importance by pediatricians.
Retinal vascular abnormalities involving the periphery as well as the macula appear to account for the primary disease process in the eye(5). The findings in the fellow eyes of both of our patients supported the evidence that postnatal vascular shutdown and macular infarction can occur in IP patients. The ophthalmic and angiographic features of our patients suggest that an ischemic retina with its vasoproliferative sequelae, rather than RPE abnormalities, constitute the primary pathogenesis of eventual retinal detachment in IP patients, as also observed by other researchers(5-7).
Cataracts are also a common feature of the disease and, in many cases, are the ocular symptoms that bring the child to the ophthalmologist. When the cataract is combined with retinal detachment, surgical results can be very poor(8), as observed in Case 1.
Ischemia of the peripheral retina with new vessel proliferation, as observed in Case 2, is one of the most common features of IP and, if not treated, is probably responsible for retinal detachment. In Case 2, laser photocoagulation was used for the ischemic area with very good outcomes, consistent with previous reports(9).
In both patients, stability of vision and ocular changes was achieved after treatment and maintained throughout the follow-up period, which was >20 years in Case 1 and 5 years in Case 2.
Despite the limited number of cases, the encouraging results achieved for the current patients, who had severe ocular manifestations of IP, indicate that it is appropriate to perform a comprehensive eye examination immediately after IP diagnosis. Moreover, patients with neonatal cataract and/or retinal problems should be adequately screened for IP.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

