INTRODUCTION
Acute anterior uveitis (AAU) is the most common type of intraocular inflammation, with varying incidence reported worldwide(1). Although, in general, it is a smaller threat to vision than posterior uveitis, it is an important cause of blindness and ocular morbidity in Brazil(1,2).
Most often, AAU manifests with varying degrees of pain and ocular hyperemia, visual blurring, and inflammatory cells in the anterior chamber (AC). In severe cases, it can be associated with increased intraocular pressure (IOP)(1). Open-angle or closed-angle glaucoma have been described in 20% uveitis cases(3), and ocular hypertension is considered an important complication of uveitis, particularly when it involves the anterior ocular segment(4).
The corneal involvement during uveitis remains understudied, although the cornea is probably a target of intraocular inflammation(2). Inflammation of the anterior segment causes changes in the endothelium that, if severe, can compromise the integrity of the cornea; these changes have been observed in some studies using specular microscopy(5). Some authors have proposed that corneal thickness is an indicator of endothelial function and suggested that this response can be clinically assessed via central pachymetry measurement(6).
Optical coherence tomography (OCT) is a noninvasive and noncontact method that provides information on corneal disorders that cannot be obtained by biomicroscopic examination(7). In addition, it is a high-resolution imaging method for the determination of the AC angle(8).
Therefore, this study aimed to analyze the corneal thickness and AC angle using Anterior Segment OCT (AS-OCT) in patients with AAU.
METHODS
This prospective study involved 22 patients (24 eyes) with AAU admitted to the emergency service of Fundação Altino Ventura de Recife-Pernambuco (FAV); patients with chronic uveitis, panuveites, intermediate and posterior uveitis, other ocular comorbidities, or previous history of eye surgery were excluded. The criteria defined by the Standardization of Uveitis Nomenclature (SUN) Working Group were used to select patients, and eye samples with scores ranging from +1 to +4 were included(9). The disease was diagnosed on the basis of clinical history and eye examination.
The subjects were invited to undergo the first OCT-SA at the time of the initial emergency visit and to return to the service for the second examination 15 days after treatment initiation. The procedure was performed before dilatation of the pupils in both situations. IOP was measured using Goldmann applanation tonometry on both consultations.
Images of the anterior segment were obtained using the anterior segment module of the RTVue® Fourier-domain system (Optovue, Fremont, California, USA). The central thickness of the cornea and the trabecular temporal angle of AC were measured during the same consultation. During the exam, the central corneal thickness was measured using the pachymetry map obtained with the use of an optional attached lens (CAM-L) (8 × 1024 A-scans). The temporal angle of AC was obtained through the scan of AC angle provided by the same lens CAM-L (1 × 1024 A-scans). The pachymetry map was generated by the system from eight 6-mm-long meridional scans centralized in the pupil. Each 6-mm line consisted of 1.024 axial scans acquired in 0.04 s and the set of eight meridians was obtained in 0.31 s. Five consecutive sets were obtained in 1.55 s and the three most consistent were used to calculate corneal power. Thickness was analyzed in three sectors: central area (2 mm central diameter); pericentral area (ring between 2 and 5 mm), and paracentral area (ring between 5 and 6 mm)(10).
The Schwalbe line (SL), a visible anatomical structure with good image definition in the sections produced by the system, was considered the reference to measure AC angle. The measure of the angle opening from SL is a method of quantifying AC angle opening in RTVue images. Transverse scans (6 × 2 mm) were performed and the temporal portion of AC angle was analyzed(10).
Statistical analysis was performed with the Epi Info (version 7) and the R-cran (version 15) software programs. The results of the quantitative variables were expressed as means ± standard deviation (SD), whereas the qualitative variables were expressed as absolute and relative frequencies. The Wilcoxon test was used to assess the mean difference, and the level of significance was set at 5%.
The study was approved by the Ethics Committee in Human Research (protocol No. 026/2011). All patients signed an informed consent and received ophthalmological follow-up care.
RESULTS
Twenty-two patients (24 eyes) participated in the study, including 15 women (68.2%) and 7 men (31.8%). The age of the participants ranged between 7 and 72 years (mean 42.8 ± 20.3 years). Seventeen patients had the first episode of AAU and 10 patients had recurrent AAU.
The results of the biomicroscopic examination of the anterior segment in the first consultation and 15 days after treatment are shown in Table 1.
Table 1 Results of the anterior segment biomicroscopy of the 24 eyes with acute anterior uveitis subjected to AS-OCT
| Initial visit | 15th day of treatment | |
|---|---|---|
| Results | n (%) | n (%) |
| Keratic precipitates | 6 (25.0) | 1 ( 4.2) |
| Fibrin membrane | 4 (16.7) | 0 ( 0.0) |
| Posterior synechiae | 7 (29.2) | 3 (12.5) |
| Iris pigments in the lens | 5 (20.8) | 4 (16.7) |
| Anterior chamber cell core | n (%) | n (%) |
| +1 | 4 (16.7) | 17 (70.8) |
| +2 | 11 (45.8) | 4 (16.7) |
| +3 | 5 (20.8) | 2 ( 8.3) |
| +4 | 4 (16.7) | 1 ( 4.2) |
Before the initiation of the treatment, the mean central corneal thickness of patients was 564.2 ± 44.2 μm; the thickness of the pericentral and paracentral areas were 580.0 ± 44.3 μm and 580.1 ± 2.9 μm, respectively. Fifteen days after the initiation of treatment, there was a reduction in corneal thickness. The mean value of the patients' central thickness was 529.5 ± 33.1 μm, the pericentral thickness was 542.6 ± 33.6 μm, and the paracentral thickness was 557.8 ± 35.3 μm. The central and pericentral corneal thickness was higher before the initiation of treatment, p = 0.0091 and 0.0068, respectively, whereas the paracentral thickness decreased; however, p was not significant (p=0.1253) (Figure 1).
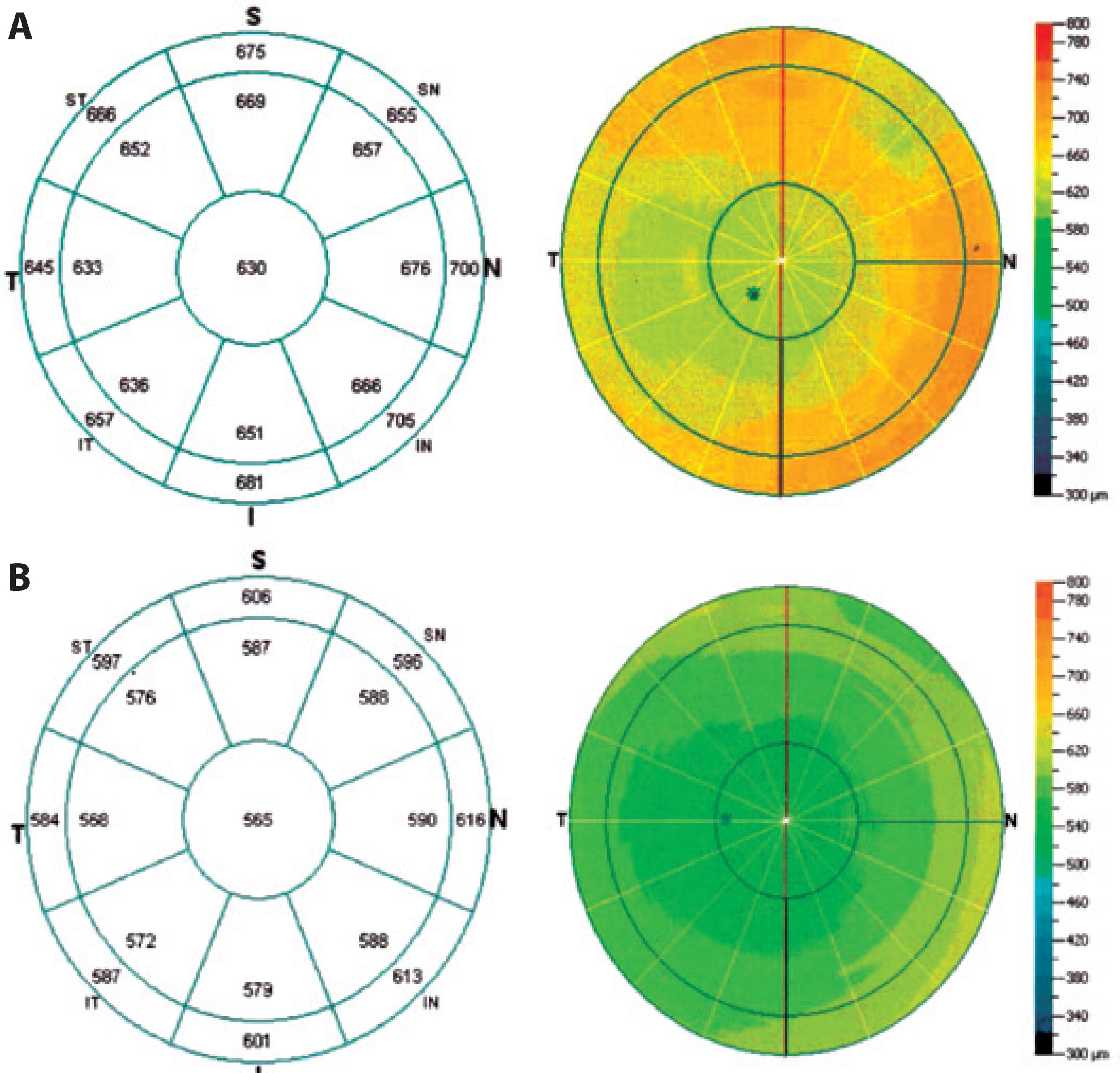
Figure 1 A) Pachymetry map before the start of the treatment. B) Pachymetry map 15 days after the start of the treatment.
The mean AC angles of participants was 44.3° ± 14.4° and the mean intraocular pressure was 10.8 ± 4.5 mmHg before treatment. After treatment, the mean AC angle were 44.7° ± 14.7° and the mean intraocular pressure was 12.3 ± 3.0 mmHg (Figure 2). Tonometry values were not obtained for two patients because of their difficulty in participating in the study. No patient had IOP of >21 mmHg. The values of AC angle and IOP between the assessed periods were not significantly different (p=0.9343 and 0.1874, respectively) (Table 2).
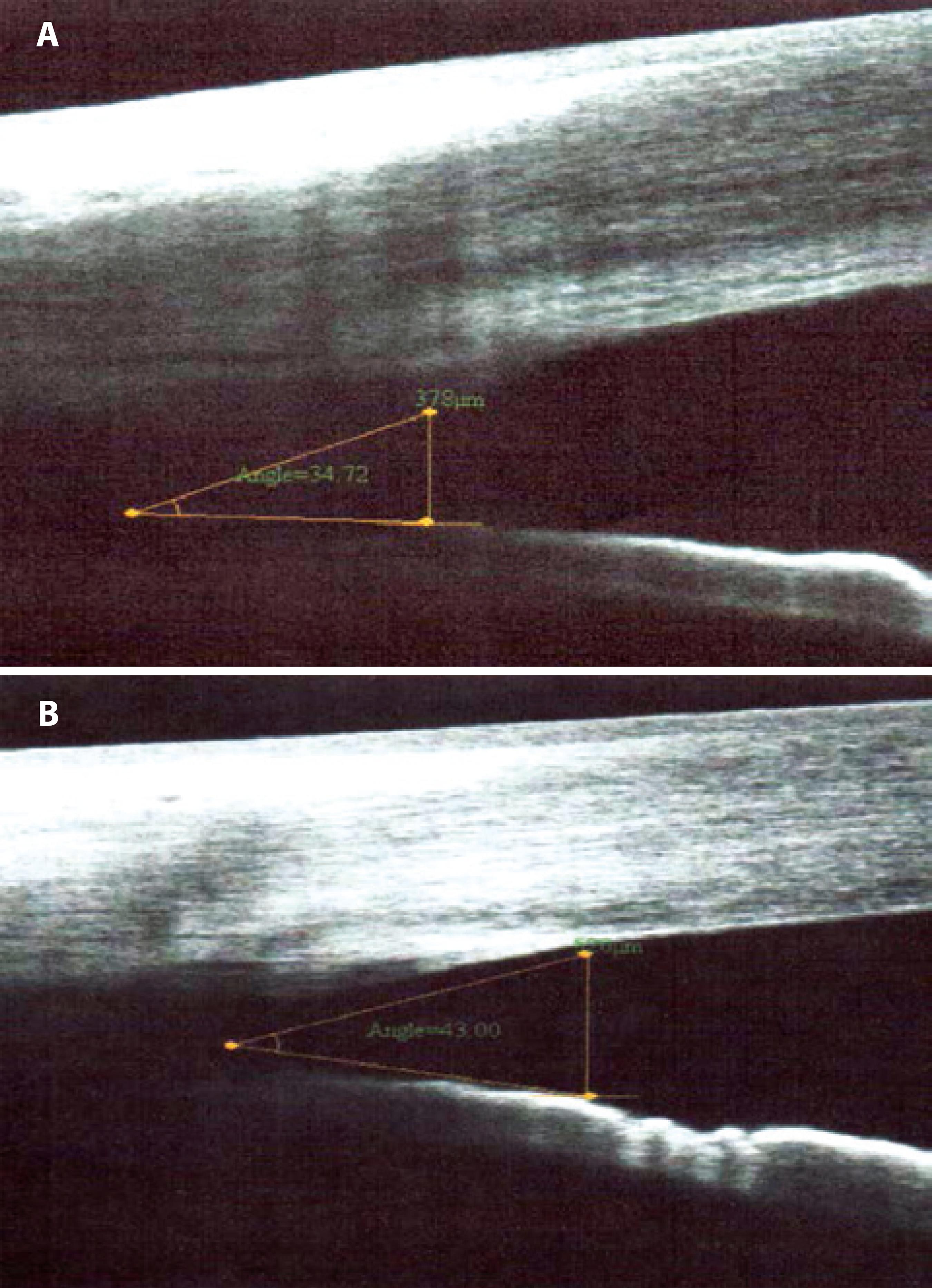
Figure 2 A) Temporal portion of the AC angle viewed on SA-OC before the start of the treatment. B) Temporal portion of AC 15 days after the start of the treatment.
Table 2 Comparison between the variables observed on AS-OCT regarding the assessment period
| Assessment period (Mean ± SD) | |||
|---|---|---|---|
| p | |||
| Variables | Pretreatment | Post-treatment | value |
| Central pachymetry (µm) | 564.2 ± 44.2 | 529.50 ± 33.1 | 0.0091 |
| Pericentral pachymetry (µm) | 580.0 ± 44.3 | 542.59 ± 33.6 | 0.0068 |
| Paracentral pachymetry (µm) | 580.1 ± 2.9 | 557.77 ± 35.3 | 0.1253 |
| Angle of the anterior chamber (º) | 44.3 ± 14.4 | 44.73 ± 14.7 | 0.9343 |
| Intraocular pressure (mmHg) | 10.8 ± 4.5 | 12.27 ± 3.0 | 0.1874 |
DISCUSSION
In general, anterior uveitis (AU) is associated with fewer sequelae than inflammation of the posterior segment, especially if it is treated early. However, its potential for severe ocular consequences is probably underestimated if recurrent or poorly managed(1).
Endothelial anomalies have been observed in cases of AU and posterior uveitis. Some authors have studied these changes in several corneal disorders and uveitis, using specular microscopy(2). It is well known that endothelial anomalies occur in uveitis(5).
Polymorphism and polymegathism of the endothelial cells can occur in AU(5,7). Studies using specular microscopy have demonstrated endothelial changes induced by inflammation, which include defects in the endothelium associated to the deposition of precipitates on the posterior surface of the cornea and other defects similar to guttata and not associated with the precipitates. Moreover, in most patients, these alterations tended to disappear completely, together with other signs of acute inflammation, without changes in cell count, and were significantly correlated with the increase in corneal thickness during the inflammatory period of the disease(11). Despite these anomalies, the majority of cases of uveitis did not progress to permanent corneal decompensation(5,6) and pachymetry values returned to normal by the end of the inflammatory crisis(6).
In a study conducted in patients with Behçet's disease, the mean central pachymetry in patients with active disease was significantly higher than that in patients with inactive disease and in the control group. Some mechanisms have been proposed to explain the negative effect of the inflammatory process on the endothelium. In this sense, several inflammatory mediators and cytokines have been found in the aqueous humor and cornea during inflammation and are probably responsible for cellular damage(6).
The patients in this study exhibited a significant reduction in mean central pachymetry between the initial period of the disease and following the control of ocular inflammation (564.2 ± 44.3 µm to 529.50 ± 33.1 µm, respectively). We would like to point out that no patient had edema of the cornea on clinical examination.
The patients in this study did not exhibit a significant change in IOP during the disease; however, inflammation of the anterior segment, particularly in severe cases, can occur with the increase in IP(1). We observed an increase in pachymetry in the sample during the uveitis crisis. Thickening of the cornea caused by edema can lead to underestimated IOP measurement by Goldmann applanation tonometry(12,13), which may interfere with the established approach.
In this study, the mean temporal AC angle was within normal values and the difference between the pretreatment and post-treatment periods was not statistically significant, probably because most of these patients exhibited mild to moderate ocular inflammation, with low frequency of posterior synechiae. In addition, there were few cases of recurrent uveitis, and without sequelae from previous episodes.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

