Vanessa Gonçalves Crespi-Flores1; Nilza Minguini1; Edméia Rita Temporini1; Keila Monteiro de Carvalho1
DOI: 10.1590/S0004-27492012000300008
ABSTRACT
PURPOSE: To verify Ophthalmology resident's and supervisor's perceptions regarding learning and teaching strabismus surgery. DESIGN: Descriptive Study. METHODS: Subjects: 1st and 2nd year residents. Each resident studied the standard strabismus surgery technique on a CD-ROM, then performed a rabbit rectus muscle recession and a strabismus surgery on a patient. A structured questionnaire was handed to the residents, and the authors made observations including variables referring to the surgical technique applied, self-evaluation of this technique and if appropriate training was given. RESULTS: Thirty-eight questionnaires were analysed. All 1st year residents (R1) had had some difficulty remembering the surgery sequence and 69.6% of 2nd year residents (R2). Concerning the surgical material handling, 93.3% of R1 and 52.2% of R2 had had any difficulty. The residents reported that during the surgery in humans, 50% remembered the experimental stage and that this training completely fulfilled their needs for 47% and partially for other 47%. CONCLUSION: Experimental surgery, more practice opportunities and resident's supervision may improve the teaching of strabismus surgery.
Keywords: Strabismus; Learning; Clinical competence; Internship and residency; Ophthalmology; education; Teaching; methods
RESUMO
OBJETIVO: Verificar percepções do residente de Oftalmologia e do supervisor em relação ao método de ensino e ao aprendizado cirúrgico de estrabismo. DESENHO: Estudo descritivo. MÉTODOS: Participantes: residentes do 1º (R1) e 2º (R2) ano. Cada residente estudou a técnica cirúrgica padrão em CD-ROM, então, realizou um retrocesso de músculo reto de coelho albino, e em sequência, cirurgia de correção de estrabismo em pacientes. Foi aplicado questionário estruturado aos residentes, e registradas observações do aprendizado pelo supervisor, incluindo-se variáveis referentes à aplicação da técnica cirúrgica de estrabismo, autoavaliação do domínio da técnica e do treinamento recebido. RESULTADOS: Foram estudados 38 questionários. Todos R1 relataram ter pouca ou média dificuldade em relação à lembrança da sequência de passos do procedimento e 69,6% dos R2. No manuseio do instrumental 93,3% dos R1 relataram algum grau de dificuldade e 52,2% dos R2. Os residentes relatam que no momento cirúrgico lembram do que foi ensinado na fase experimental (50%), e que este treinamento atende totalmente suas necessidades para 47% dos residentes e em parte para outros 47%. CONCLUSÃO: Cirurgia experimental, mais oportunidades práticas e supervisão dos residentes pode aprimorar o ensinamento cirúrgico de estrabismo.
Descritores: Estrabismo; Aprendizagem; Competência clínica; Internato e residência; Oftalmologia; educação; Ensino; métodos
ORIGINAL ARTICLE ARTIGO ORIGINAL
Strabismus surgery learning for Ophthalmology residents of university service
Aprendizado cirúrgico de estrabismo para residentes de Oftalmologia de serviço universitário
Vanessa Gonçalves Crespi-FloresI; Nilza MinguiniI; Edméia Rita TemporiniII; Keila Monteiro de CarvalhoI
IPhysician, Faculty of Medical Sciences. Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
IIPublic Health Professor, Faculty of Medical Sciences. Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
ABSTRACT
PURPOSE: To verify Ophthalmology resident's and supervisor's perceptions regarding learning and teaching strabismus surgery.
DESIGN: Descriptive Study.
METHODS: Subjects: 1st and 2ndyear residents. Each resident studied the standard strabismus surgery technique on a CD-ROM, then performed a rabbit rectus muscle recession and a strabismus surgery on a patient. A structured questionnaire was handed to the residents, and the authors made observations including variables referring to the surgical technique applied, self-evaluation of this technique and if appropriate training was given.
RESULTS: Thirty-eight questionnaires were analysed. All 1st year residents (R1) had had some difficulty remembering the surgery sequence and 69.6% of 2nd year residents (R2). Concerning the surgical material handling, 93.3% of R1 and 52.2% of R2 had had any difficulty. The residents reported that during the surgery in humans, 50% remembered the experimental stage and that this training completely fulfilled their needs for 47% and partially for other 47%.
CONCLUSION: Experimental surgery, more practice opportunities and resident's supervision may improve the teaching of strabismus surgery.
Keywords: Strabismus/surgery; Learning; Clinical competence; Internship and residency; Ophthalmology/education; Teaching/methods
RESUMO
OBJETIVO: Verificar percepções do residente de Oftalmologia e do supervisor em relação ao método de ensino e ao aprendizado cirúrgico de estrabismo.
DESENHO: Estudo descritivo.
MÉTODOS: Participantes: residentes do 1º (R1) e 2º (R2) ano. Cada residente estudou a técnica cirúrgica padrão em CD-ROM, então, realizou um retrocesso de músculo reto de coelho albino, e em sequência, cirurgia de correção de estrabismo em pacientes. Foi aplicado questionário estruturado aos residentes, e registradas observações do aprendizado pelo supervisor, incluindo-se variáveis referentes à aplicação da técnica cirúrgica de estrabismo, autoavaliação do domínio da técnica e do treinamento recebido.
RESULTADOS: Foram estudados 38 questionários. Todos R1 relataram ter pouca ou média dificuldade em relação à lembrança da sequência de passos do procedimento e 69,6% dos R2. No manuseio do instrumental 93,3% dos R1 relataram algum grau de dificuldade e 52,2% dos R2. Os residentes relatam que no momento cirúrgico lembram do que foi ensinado na fase experimental (50%), e que este treinamento atende totalmente suas necessidades para 47% dos residentes e em parte para outros 47%.
CONCLUSÃO: Cirurgia experimental, mais oportunidades práticas e supervisão dos residentes pode aprimorar o ensinamento cirúrgico de estrabismo.
Descritores: Estrabismo/cirurgia; Aprendizagem; Competência clínica; Internato e residência; Oftalmologia/educação; Ensino/métodos
INTRODUCTION
Strabismus surgery may have complications, like scleral perforation and muscle loss. Scleral perforations' incidence varies between 0.13% and 12%(1-4). This incidence, with the improvement of surgical techniques and the use of modern needles, is much lower(2,5).To better define the perforation incidence, Simon et al. reported 728 cases in 553,565 surgeries, an incidence of 1.32/1000, but perforations were twice as common with residents or fellows operating(2).
The surgical training of a resident in the area of Ophthalmology should have maximal attention on the teaching program because of its complexity due to the difficulty in standardizing a training method. Defining teaching competencies' methods and evaluation tools are necessary(6).The surgical experience must feature a progressive development of surgical practice(7),but the individual learning abilities vary a lot inside a resident group. Surgery residents enter residency programs with varying levels of knowledge and skills(8).
In the United States (US) the residency program, including Ophthalmology, is accredited by an organization called Accreditation Council for Graduate Medical Education (ACGME). Changes in the health care environment have created a demand for a new set of competencies in residency training(9) defined by ACGME.These competencies are: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, systems-based practice(10).The "American Board of Ophthalmology" added another competency: surgery(10).Therefore, significant modifications from its present form to produce competent surgeons for the future are required(11). Lee, Volpe(10) proposed methods and curriculum changes to conform the medical teaching to ACGME requirements, including the laboratorial surgery practice. Surgery conferences and assistant surgeon observation are also fundamental.
Self-evaluation and performance questionnaires have been used to study surgical education. The self-evaluation is an important teaching strategy(12,13) and a tool used and validated by previous studies(14).Some authors have studied and validated a resident's perception questionnaire that works like an educational evaluated tool in surgery environment, detecting areas to be improved(11).
The use of controlled educational settings to help surgery residents acquire basic knowledge and skills regarding adverse events should enhance patient safety and improve outcomes(15).
Our aim was to verify Ophthalmology resident's and supervisor's perceptions about learning and teaching strabismus surgery, acquiring subsidies for strabismus learning improvement.
METHODS
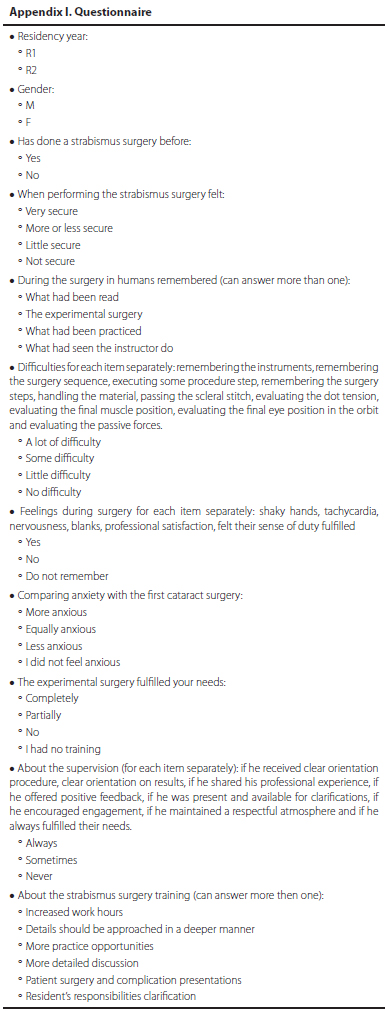
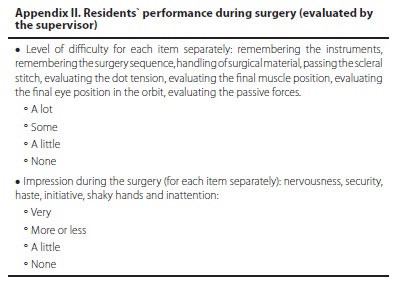
Descriptive study. Subjects: The inclusion criteria were first and second year Ophthalmology residents in 2005 and 2007 of the University Hospital, who signed the informed consent. The exclusion criteria were residents who did not want to participate or did not answer the questionnaire. The study involves animal experimentation (rabbits), according to ethical principles from the Regional Committee and The Association for Research in Vision and Ophthalmology (ARVO/USA). This project was approved by the Ethical Committee from this Institution. Each resident studied the standard horizontal rectus muscle recession surgery technique on CD-ROM, and under supervision, performed a rabbit rectus muscle recession. Then, he or she did a strabismus surgery on a patient at Clinical Hospital. A structured questionnaire was handed to the residents after the procedure, including variables referring to the surgical technique applied, self-evaluation of this technique and if appropriate training was given (Appendix I). The authors evaluated the residents` performance during the surgery regarding the level of difficulty, anxiety, shaky hands and insecurity (Appendix II). The data was entered into the EPI-INFO (Epidemiological Information) program and had its frequency analyzed.
RESULTS
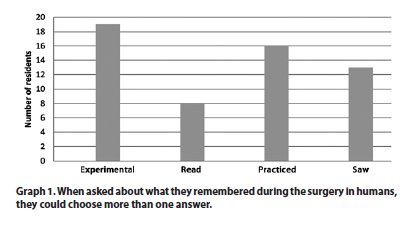
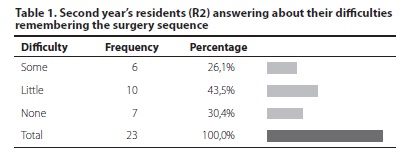
Forty-three residents were evaluated but only 38 questionnaires were analysed (5 were not handed in). Fifteen were R1 (40%) and 23 were R2 (60%). Twenty-four were male (63%) and 14 (37%) were female. Thirty-six per cent had already done a strabismus surgery. None of the first year residents (R1) had ever done a strabismus surgery before and 63% of the second year residents had already done at least one. When asked about what they remembered during the surgery in humans, they could choose more than one answer (Graphic 1). Furthermore, about the recollection during the patient's surgery, 29% had no difficulty remembering the surgical instruments and 18% in remembering the procedure sequence. All of the R1 and 70% of R2 had some difficulty remembering the surgery sequence (Table 1). When asked about their hardships, they could refer to more than one and 92% had some difficulty executing some procedure step, 79% remembering the surgery steps, 68% handling the materials, 82% passing the scleral stitch, 82% evaluating the dot tension, 87% evaluating the final muscle position, 84% evaluating the final eye position in the orbit, 97% evaluating the passive forces. Concerning the handling of the surgical material, 93% of R1 and 52% of R2 related any difficulty.
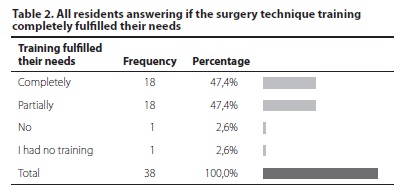
During the patient's surgery, 24% of the residents felt shaky hands, 11% had tachycardia, 34% felt nervous, 10% had blanks, 95% felt professional satisfaction, 95% felt their sense of duty fulfilled, and comparing with the cataract surgery 87% felt less or not anxious at all. The surgical technique training completely fulfilled the needs of 47% (Table 2). All residents said that they had been oriented about the procedure and results.
Evaluating the instructor, 87% of the residents said that he always shared his experience and 92% that he always gave positive feedback and was always present for 95%. He always encouraged engagement for 89%, maintained a respectful atmosphere for 95% and always fulfilled their needs for 95%.
Concerning the strabismus surgery training, the residents suggested changes: 55% in working hours, 37% that the details should be approached in a deeper manner, 50% a more detailed discussion, 84% more practice opportunities, 16% patient surgery and complication presentations, and 16% a resident's responsibilities clarification.
Forty-three supervisor's charts concerning the resident's surgical procedures were analysed. Nineteen were R1 (44%), and 24 were R2 (56%). Seventy-two per cent had some difficulty remembering which materials had been used, 88% remembering the procedure sequence, 70% handling the materials, 88% passing the scleral stitch, 84% evaluating the dot tension, 84% evaluating the final muscle position, 95% evaluating the final eye position in the orbit, and 100% evaluating the passive forces.
Comparing the questions, we observed that the residents who felt secure performing the strabismus surgery also felt that experimental surgery completely or almost completely fulfilled their needs, but of the residents who felt a little insecure (8 residents), 25% (2 residents) acknowledged that it did not.
Twelve residents had already done strabismus' surgery before and only one of those (18%) recalled the experimental practice during the surgery, but considering those who had never done a strabismus' surgery before (21), 66% (14 residents) remembered the experimental training. Considering those who had already done a surgery before, 18% felt nervous, 33% had shaky hands and 25% tachycardia. The residents that had never done a surgery before reported: 43% felt nervous, 19% shaky hands and 5% tachycardia.
Comparing the resident's answers and the supervisor's impressions, despite the latter's observations like anxiety (63%), shaky hands (65%) and some insecurity (98%), 51% of residents did not report any of these feelings.
DISCUSSION
This study describes the resident's perceptions regarding teaching and their own surgery's learning through an anonymous questionnaire. Hence, each resident had freedom to expose his impressions regarding knowledge and difficulty, and also regarding their instructor and supervision.
The number of first year residents with some difficulty remembering the procedure sequence or handling the instruments is higher than the number of the second year residents with these hardships. We may assume that it is because of a bigger practical opportunity that the second year residents had during residency, who also felt more secure about performing surgery. The experimental surgery combined with observation and discussions could decrease anxiety and improve performance.
There is a consensus that the residents entering training programs in surgery must have minimum surgical practice before starting their second residency year. Even studying in books and Atlas and performing as assistant surgeon, the first surgery on patients can cause distress, anxiety or frustration if the resident does not feel prepared. The improvement on technical skills should occur in an initial learning stage and the surgery training focus should be on new teaching methods and knowledge transfer.
Traditionally, technical skills have been learned by the resident as an assistant surgeon in the operating room(6), which may not be the best occasion to learn. The environment can be hostile and stressful, and the teaching cannot be patterned. Training outside the operating room offers solutions to some of these problems and accelerates the learning curve(16).An experimental education module helps relieve some anxiety during the first surgery in humans and the feedback allows the supervisor to encourage the resident to correct his errors. Furthermore, it is an attempt to combine knowledge and technical, interpersonal and professional skills. The experimental surgery on animals is performed in controlled settings, this being important in the learning process which can develop skills, increasing the resident's self-confidence, basic prerequisites to reduce complication rates.
The supervisor's impressions and the resident's answers diverged concerning nervousness, shaky hands and insecurity during the surgery on the patient. Since the answers were evaluated on an anonymous questionnaire, we believe that the resident, despite feeling nervous or insecure, preferred not to make any comment, as self-assurance. The supervisor is also important when he gives positive reinforcement for a first year insecure resident or a second year resident, who is much more confident but nevertheless needs orientation.
The residents recalled during the surgery especially what they had been learning in the experimental stage and what they had previously practiced. Although only 50% pointed out the experimental surgery as important, this was the most efficient way to learn, according to the questionnaires.
According to Lee et al.(17), learning and retention rates after lectures alone are poor, and seminars, web-based or interactive presentations may improve retention rates. Other authors(18)studied the impact of standardized patient (SP) use to improve abilities on clinical exams, showing a significant positive impact on the student group that used this learning method. On surgical practices, the animal surgery can help enhance attention and learning. Scott et al.(19),studying laparoscopic surgery learning, give evidence that bench models with simulations may improve resident's technical skills.
Brewster et al.(15), created an educational model to integrate technical and clinical skills, emphasizing interpersonal and communication abilities, as well as professionalism. They used standardized patients, a bench model simulation, and a five-point scale using global rating forms to study resident's performance during training.
The appropriate surgical training of a resident in the area of Ophthalmology is still considered a complex and challenging subject that should not be overlooked(7).
Regarding resident's perceptions about teaching and learning strabismus surgery with self-evaluation, the residents claimed that during surgery in patients, they recalled what had been taught in the experimental stage (50%) and that this training totally fulfilled their needs for 47%, and partially for other 47%. In order to improve teaching techniques, 84% suggested more practice opportunities and 55% increased work hours.
The supervisor's evaluation of resident's attitude during strabismus surgery describes symptoms like nervousness (63%), shaky hands (65%), and some insecurity (98%), factors that were not reported by some residents, since 51% did not point out any feeling, showing a divergence between self-criticism and the supervisor's evaluation.
This preparation - including experimental surgery, along with more practice opportunities and resident's supervision - may improve strabismus surgery teaching.
CONCLUSION
The experimental surgical practice of strabismus in rabbits may represent an important form of practical learning which should precede surgery in patients, so that the resident can become familiar with instrument manipulation techniques and with ocular tissues.
We suggest new projects in this area like multicenter and controlled studies, to test the surgical resident's improvement and the application of new training methods.
ACKNOWLEDGEMENT
To the Department of Experimental Surgery for its professionalism and dedication.
REFERENCES
1. Monteiro de Carvalho KM. Amblyopia: care and prevalence in pre-school children. In: Campos EC. Strabismus and ocular motility disorders. London: The Macmillam; 1990. p.39-43.
2. Simon JW, Lininger LL, Scheraga JL. Recognized scleral perforation during eye muscle surgery: incidence and sequelae. J Pediatr Ophthalmol Strabismus. 1992;29(5):273-5.
3. Morris RJ, Rosen PH, Fells P. Incident of inadvertent globe perforation during strabismus surgery. Br J Ophthalmol. 1990;74(8):490-3.
4. Noel L, Bloom JN, Clarke WN, Bawazeer A. Retinal perforation in strabismus surgery. J Pediatr Ophthalmol Strabismus. 1997;34(2):115-7.
5. Goldestein JH, Prepas SB, Conrad SD. Effect of needle characteristics in strabismus surgery. Arch Ophthalmol. 1982;100(4):617-8.
6. Silva MR. O ensino da Oftalmologia. Rev Bras Oftalmol. 2009;68(3):127-8.
7. Crouch ER Jr. A comparison of the success rates of resident and attending strabismus surgery: discussion. J Pediatr Ophthalmol Strabismus. 1993;30(3):157-8.
8. Sachdeva AK, Loiacono LA, Amiel GE, Blair PG, Friedman M, Roslyn JJ. Variability in the clinical skills of residents entering training programs in surgery. Surgery. 1995; 118(2):308-9.
9. Lee AG. The new competencies and their impact on resident training in ophthalmology. Surv Ophthalmol. 2003;48(6):651-62.
10. Lee AG, Volpe N. The impact of the new competencies on resident education in ophthalmology. Ophthalmology. 2004;111(7):1269-70.
11. Kanashiro J, McAleer S, Roff S. Assessing the educational environment in the operating room - a measure of resident perception at one Canadian institution. Surgery. 2006;139(2):150-8.
12. Domingues RC, Amaral E, Zeferino AM. Auto-avaliação e avaliação por pares - estratégias para o desenvolvimento profissional do médico. Rev Bras Educ Med. 2007; 31(2):173-5.
13. Zeferino AM, Domingues RC, Amaral E. Feedback como estratégia de aprendizado no ensino medico. Rev Bras Educ Med. 2007;31(2):176-9.
14. Claridge JA, Calland JF, Chandrasekhara V. Young JS, Sanfey H, Schirmer BD. Comparing resident measurements attending surgeon self- perceptions of surgical educators. Am J Surg. 2003;185(4):323-7.
15. Brewster LP, Risucci DA, Joehl RJ, Littooy FN, Temeck BK, Blair PG, et al. Management of adverse surgical events: a structured education module for residents. Am J Surg. 2005;190(5):687-90.
16. Binenbaum G, Volpe NJ. Ophthalmology resident surgical competency: a national survey. Ophthalmology. 2006;113(7):1237-44.Comment in: Ophthalmology. 2007; 114(4):829-30; author reply 830. Opthalmology. 2006;113(12):2380-1.
17. Lee AG, Beaver HA, Greenlee E, Oetting TA, Boldt HC, Olson R, et al. Teaching and assessing systems- based competency in ophthalmology residency programs. Surv Ophthalmol. 2007;52(6):680-9.
18. Sachdeva AK, Wolfson PJ, Blair PG, Gillum DR, Gracely EJ, Fridman M. Impact of a standardized patient intervention to teach breast and abdominal examination skills to third-year medical students at two institutions. Am J Surg. 1997;173(4):320-5.
19. Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, et al. Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg. 2000;191(3):272-83.
 Correspondence address:
Correspondence address:
Vanessa Gonçalves Crespi-Flores.
Av. Jesuíno Marcondes Machado, 585
Campinas - SP - 13092-320 - Brazil
E-mail address: [email protected]
Submitted for publication: February 6, 2012
Accepted for publication: April 5, 2012
Study was carried out at Department of Ophthalmology, Strabismus Division Faculty of Medical Sciences - UNICAMP - Campinas (SP), Brazil.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: V.G.Crespi-Flores, None; N.Minguini, None; E.R. Temporini, None; K.M.de Carvalho, None.
Institutional Review Board FCM/UNICAMP (CEP: 463-2004)