

João Borges Fortes Filho1; Gabriela Unchalo Eckert2; Marcia Beatriz Tartarella2; Renato Soibelmann Procianoy2
DOI: 10.1590/S0004-27492011000300016
ABSTRACT
Retinopathy of prematurity (ROP) is related to oxygen-regulated vascular endothelial growth factor and to insulin-like growth factor-I. After premature birth, supplemental oxygen induces a retinal hyperoxic condition with vasoconstriction and to a definitive interruption of retinal vasculogenesis. Peripheral ischemia may stimulate retinal neovascularization and the onset of additional ROP-related complications. The natural course of the disease may result in irreversible blindness if not promptly diagnosed and attended. Recently, a significant increase in the prevalence of ROP has been observed in survival rates of preterm infants, especially in emerging-economy countries in Latin America, Asia, and Eastern Europe. This article addresses the main preventive measures in ROP.
Keywords: Retinopathy of prematurity; Blindness; Risk factors
RESUMO
A retinopatia da prematuridade (ROP) está relacionada com o fator de crescimento do endotélio vascular e com o fator de crescimento insulínico-I. Após o nascimento prematuro, o oxigênio suplementar provoca hiperóxia retiniana com vasoconstrição e interrupção definitiva na vasculogênese retiniana. A isquemia retiniana periférica estimula a neovascularização e o surgimento das demais complicações da ROP. A doença, em sua evolução natural, poderá levar à cegueira irreversível, se não for diagnosticada e tratada oportunamente. Recentemente, houve um aumento na prevalência da ROP pela maior sobrevivência de nascidos prematuros especialmente nos países de economia em desenvolvimento na America Latina, Ásia e no Leste Europeu. Nesse artigo vamos abordar as principais medidas preventivas em ROP.
Descritores: Retinopatia da prematuridade; Cegueira; Fatores de risco
REVIEW ARTICLE ARTIGO DE REVISÃO
Prevention of retinopathy of prematurity
Prevenção da retinopatia da prematuridade
João Borges Fortes FilhoI; Gabriela Unchalo EckertII; Marcia Beatriz TartarellaIII; Renato Soibelmann ProcianoyIV
IPhysician, Department of Ophthalmology, Faculdade de Medicina, Universidade Federal do Rio Grande do Sul - UFRGS - Porto Alegre (RS) Brazil; Program for the Prevention of Blindness due to Retinopathy of Prematurity - PROROP - of Hospital de Clínicas de Porto Alegre, Porto Alegre (RS), Brazil
IIPhysician, Department of Ophthalmology, Hospital das Clínicas de Porto Alegre - Porto Alegre (RS), Brazil; Program for the Prevention of Blindness due to Retinopathy of Prematurity - PROROP - of Hospital de Clínicas de Porto Alegre, Porto Alegre (RS), Brazil
IIIPhysician, Department of Ophthalmology, Congenital Cataract Section, Escola Paulista de Medicina, São Paulo Federal University - UNIFESP, São Paulo (SP), Brazil; Program for the Prevention of Blindness due to Retinopathy of Prematurity - PROROP - of Hospital de Clínicas de Porto Alegre, Porto Alegre (RS), Brazil
IVPhysician, Department of Pediatrics and Neonatology, Faculdade de Medicina, Universidade Federal do Rio Grande do Sul - UFRGS - Porto Alegre (RS), Brazil; Program for the Prevention of Blindness due to Retinopathy of Prematurity - PROROP - of Hospital de Clínicas de Porto Alegre, Porto Alegre (RS), Brazil
ABSTRACT
Retinopathy of prematurity (ROP) is related to oxygen-regulated vascular endothelial growth factor and to insulin-like growth factor-I. After premature birth, supplemental oxygen induces a retinal hyperoxic condition with vasoconstriction and to a definitive interruption of retinal vasculogenesis. Peripheral ischemia may stimulate retinal neovascularization and the onset of additional ROP-related complications. The natural course of the disease may result in irreversible blindness if not promptly diagnosed and attended. Recently, a significant increase in the prevalence of ROP has been observed in survival rates of preterm infants, especially in emerging-economy countries in Latin America, Asia, and Eastern Europe. This article addresses the main preventive measures in ROP.
Keywords: Retinopathy of prematurity; Blindness/prevention & control; Risk factors
RESUMO
A retinopatia da prematuridade (ROP) está relacionada com o fator de crescimento do endotélio vascular e com o fator de crescimento insulínico-I. Após o nascimento prematuro, o oxigênio suplementar provoca hiperóxia retiniana com vasoconstrição e interrupção definitiva na vasculogênese retiniana. A isquemia retiniana periférica estimula a neovascularização e o surgimento das demais complicações da ROP. A doença, em sua evolução natural, poderá levar à cegueira irreversível, se não for diagnosticada e tratada oportunamente. Recentemente, houve um aumento na prevalência da ROP pela maior sobrevivência de nascidos prematuros especialmente nos países de economia em desenvolvimento na America Latina, Ásia e no Leste Europeu. Nesse artigo vamos abordar as principais medidas preventivas em ROP.
Descritores: Retinopatia da prematuridade; Cegueira/prevenção & controle; Fatores de risco
INTRODUCTION
Retinopathy of prematurity (ROP), a disease known for over 50 years in countries with low perinatal mortality rates, has been characterized in recent years by an epidemic pattern in several emerging-economy countries with good human development(1). This fact is directly related to the improvement in prenatal and perinatal care, which has allowed increased survival among very low birth weight (VLBW: birth weight (BW) <1,500 grams) or among extremely low birth weight (ELBW: BW <1,000 grams) preterm infants.
The natural course of ROP leads to blindness, causing a social and financial burden on the community. Irreversibly impaired vision may also hinder cognitive and psychomotor development of the affected children(2).
ROP may be prevented by providing health care for the infant during their stay in the Neonatal Intensive Care Unit (NICU). This instructional article analyzes the main measures required for a proper diagnosis in patients at risk of developing ROP and also addresses preventive measures that may be taken to reduce the occurrence of ROP.
THE OXYGEN-THERAPY AND OCCURRENCE OF ROP
The disease correlation with the oxygen-therapy was demonstrated by Campbell, in Australia, in 1951(3), and by Crosse and Evans, in England, in 1952(4). Those studies, suggesting that the indiscriminate use of oxygen soon after birth was related to onset of ROP, produced immediate effects worldwide and, between 1951 and 1960, restrictions on the postnatal use of oxygen created the misimpression that ROP was under control. That period, in which an actual reduction in ROP-related blindness was observed, also corresponded to higher mortality and increased comorbidity among surviving preterm infants. Between 1960 and 1970, oxygen administration was better accepted in NICU, with a significant increase in survival of preterm babies, and, again, several cases of the disease arose.
Oxygen-therapy may be potentially toxic to several organs and tissues, including the still immature retina. Patz et al., in controlled clinical trials since 1952, observed a higher incidence of ROP in patients receiving high oxygen concentrations(5). In the 1960s, it became possible to analyze arterial blood gases, but the limits of arterial oxygen pressure (PaO2) to effectively prevent onset of ROP had yet to be established. The development of pulse oximeters, a device that monitors the oxygen concentration in the skin, revealed wide fluctuations in oxygen levels delivered to preterm and also demonstrated that continuous monitoring of PaO2 may contribute to significantly reduce the incidence of ROP(6). The guidelines issued by the American Academy of Pediatrics currently recommend maintaining PaO2 at 45-80 mmHg with oxygen saturation limits of 85-95% for preterm infants with GA >32 weeks and 85-93% for newborn infants with GA <32 weeks(7).
Preterm infants are more prone to the effects of oxygen toxicity, since they were used to low oxygen tensions during intrauterine life (approximately 22 to 24 mmHg). After premature birth, there is a dramatic increase in oxygen concentration, which may lead to sustained hyperoxia that may overproduce vascular endothelial growth factor (VEGF). High levels of VEGF stimulate neovascularization of the retina, which in severe cases may result in retinal fibrosis and retinal detachment. Repeated episodes of hypoxia-hyperoxia favor the progression of ROP. Restricted use of oxygen can reduce the relative risk for occurrence of ROP(8).
A cohort study, conducted in England between 1990 and 1994, showed that survival of preterm infants nursed in enough oxygen to maintain a saturation of 80-90% was similar to that in the group with oxygen saturation of 88-98%. However, the incidence of ROP (threshold disease) was 6% in the group with restricted oxygen saturation and 28% in the group with saturation of 88-98%(9).
York et al., between 1993 and 1995, analyzed blood gases of 231 newborn infants with BW <1,500 grams. They concluded that variations in oxygen concentrations were directly associated with a higher incidence of ROP onset(10).
Chow et al.(11) reported the results of an educational program for oxygen delivery and monitoring in VLBW infants implemented in 1998. Oxygen saturation was maintained at 85-95% for infants >32 weeks' gestation and at 85-93% for infants <32 weeks' gestation. Alarm limits at 83-93% were used to monitor oxygen saturation. After strict monitoring of respiratory gases, the incidence of ROP 3 to 4 decreased from 12.5% in 1997 to 2.5% in 2001. The need for ROP laser treatment in the whole sample decreased from 4.4% in 1997 to 0% at the end of 1998.
In the NICU of Hospital de Clínicas de Porto Alegre (HCPA), southern Brazil, careful management of oxygen delivery and duration, based not only on clinical criteria, such as cyanosis and cardiorespiratory changes, but also on pulse oximetry maintaining oxygen saturation at the recommended range of 88-94%, also allowed a significant reduction in the occurrence of ROP severe enough to require treatment: from 6.2% in 2005 and 6.7% in 2006 to 4.2% in 2007 and 0% in 2008, 2009, and 2010. The strict management of oxygen delivery to VLBW preterm infants as soon after birth using blender oxygen monitors and pulse oximetry during all the oxygen-therapy period significantly reduced the need for laser treatment (Forte Filho JB et al. Personal communication).
PATHOGENESIS OF ROP AND THE RELATIONSHIP WITH VEGF AND IGF-I
The occurrence of ROP is related to VEGF, an oxygen-regulated factor, and to other non-oxygen-regulated factors, including insulin-like growth factor-I (IGF-I). IGF-I plays an important role in the normal development of retinal vascularization. This factor, at low serum levels, inhibits the natural course of retinal vascularization and, when in excess, stimulates neovascularization. Low serum IGF-I levels, in the first weeks following premature birth, have been associated with a greater likelihood of developing later ROP as well as it is related to disease severity(12).
After premature birth, supplemental oxygen induces a hyperoxic condition that leads to vasoconstriction, vascular obliteration, peripheral ischemia, and definitive interruption of retinal vascular development. Hyperoxia, if maintained for a longer period of time, causes VEGF overproduction, which stimulates undesired retinal neovascularization and the onset of additional ROP-related complications. Supplemental oxygen exposes the retina to PaO2 ranging from 60 to 100 mmHg, which is much higher than the intrauterine tension of 22 to 24 mmHg(12).
In infants who are likely to develop ROP, peripheral retinal vessel growth becomes sluggish or is totally interrupted resulting in an avascular and hypoxic peripheral retina (Phase 1 of ROP). The proliferative phase of disease (Phase 2 of ROP) occurs due to this ischemia. Total extent of lack of retinal perfusion in the early phase of ROP seems to determine the subsequent severity of disease that may lead to retinal detachment and irreversible blindness(12,13).
VEGF is a potent angiogenic factor necessary for normal growth of blood vessels, but, at the same time, it is associated with undesired neovascularization both in the retina and the iris. When a premature birth occurs, there is a reduction in VEGF expression. It is suggested that this phenomenon results from the hyperoxia experienced by the premature infants, since hypoxia induces a vaso-obliteration state due to endothelial cell apoptosis. As the retina gets mature and hypoxic, due to vascular growth interruption, VEGF levels increase progressively until undesired retinal neovascularization starts (Phase 2 of ROP). VEGF inhibition, at this phase, however, cannot prevent retinal neovascularization of ROP, proving that this is indeed a multifactorial disease(12,13).
MAIN RISK FACTORS FOR ROP
Several risk factors (RF) for ROP have been studied over the past 50 years. Among them, general immaturity and debility of the infant's physical health status, low BW, and prolonged oxygen-therapy have been consistently related to disease onset. Maternal use of antenatal steroids and beta-blockers, exposure to bright light in the hospital nursery, use of corticosteroids, indomethacin, surfactant, and erythropoietin, the twin situation, need for arterial duct treatment, presence of intracranial hemorrhage, uncontrolled oxygen therapy, recurrent apneas, blood transfusions, immunosuppression, concomitant presence of infections, and antibiotic use have also been related to onset of ROP, although in a less consistent manner. Blood transfusions in premature infants produce hemodynamic changes due to the reduced blood volume of these patients. Upon receiving adult erythrocytes premature babies may be affected by tissue toxicity due to increased oxygen supply to the retina(14).
Poor postnatal weight gain (WG) in the first weeks of life following premature birth is currently considered an important and consistent RF for onset of ROP, as reported in several studies. Wallace et al.(15), in 2000, suggested that WG less than 50% of BW in the first six weeks of life could indicate an important risk for the development of severe ROP (stages 3, 4 or 5) and concluded that there was a significant difference in WG in children who developed ROP (stage 3 or greater) when compared with children without ROP or with mild ROP (stages 1 or 2). Löfqvist et al.(16) proposed, in 2006, the use of postnatal WG variation together with serum IGF-I levels as definitive and early markers of the risk of a preterm infants developing ROP. This would allow identifying, in a timely manner, babies at risk of developing severe ROP. Fortes Filho et al.(17), in 2009, demonstrated in a prospective study the practical importance of assessing and monitoring WG in the first 6 weeks of life as a predictive factor for later onset of ROP. In that study, it was reported that the occurrence of WG less than 51.2% of BW in the first 6 weeks of life was indicative for the development of severe ROP. Since assessing and monitoring WG can be easily performed during screening programs for detection of ROP, and especially because it does not add costs to the public health system of developing countries, this procedure would be of paramount importance as a practical clinical tool for ophthalmologists carrying out screening sessions for detection of ROP(17,18).
It is important to understand that risk factors for the development of severe ROP show a dynamic behavior in relation to GA, that is, patients with lower GA develop ROP because of their prematurity at birth, whereas patients with higher GA develop ROP as a result of several diseases or comorbidities associated with prematurity, including sepsis and hyaline membrane disease(19).
DIAGNOSIS OF ROP ON SCREENING EXAMINATIONS IN NICU
Screening programs to detect ROP, including systematic fundus examinations at NICU in infants at risk for ROP, provide the best possibility of diagnosing the disease in order to establish an appropriate treatment prior to progression to more advanced stages and blindness.
Inclusion criteria of patients in screening programs vary greatly among countries, or even across regions within a country, and are often based on BW and GA.
In Brazil, in 2002, it was established that screening for early detection of ROP should be performed in all preterm infants with BW <1,500 grams and/or GA <32 weeks. Initial ophthalmological examination should be performed between the 4th and 6th week after birth, through binocular indirect ophthalmoscopy and after pupil´s dilation and repeated according to the findings from baseline examination. Screening may also include infants with larger BW or greater GA who are at risk of developing ROP due to clinical conditions, as determined by the neonatologist in charge(20).
The efficiency of an screening program for detection and early treatment of ROP in preterm babies requires the introduction of a routine protocol in NICU and a collaborative effort involving ophthalmologists, neonatologists, and the nursing staff(21).
On the examination day, the professionals in the NICU should be able to indicate to the ophthalmologist which patients to be examined, their current and previous clinical history, their maternal antecedents, and their currently known RF for ROP, as follows: presence of bronchopulmonary dysplasia, need for oxygen-therapy, presence of sepsis, need for blood transfusions, and use of surfactant, indomethacin, or erythropoietin. Proper identification of known RF for ROP may contribute to a better management of the condition together with the team of neonatologists involved in the prevention of ROP(21).
Fundus examination in VLBW preterm infants is technically difficult to perform, requiring previous training and experience and adequate support from the nursing staff due to the poor health status of the preterm infants. In several occasions, examinations involve patients on ventilatory support with unstable vital signs, who are more prone to side effects of mydriatic eyedrops and to eye manipulations by the ophthalmologist. Therefore, the presence of the nursing staff throughout the procedure is extremely important in order to control and maintain an open airway, to monitor the infant's vital signs and behavior, and to avoid life-threatening conditions(21).
Mydriatic eyedrops routinely used in examinations are not free from side effects and may lead to cardiorespiratory complications, especially in weaker patients. A study conducted in 1996 by Laws showed a mean increase of 6 mmHg in diastolic pressure following topical mydriatics. During fundus examination, there was a further increase in both diastolic and systolic pressure of about 4 mmHg, and the latter was likely to be a response to the stress of the procedure(22). The involvement of the nursing staff is therefore of paramount importance during administration of eyedrops and throughout the ophthalmological examination, requiring previous training of the whole team to achieve adequate dilation of the pupils with minimal side effects to the preterm. The combination of 0.5% tropicamide and 2.5% phenylephrine eyedrops, administered 3 times at 5-minute intervals before examination, has shown to produce fewer side effects and an optimal mydriasis.
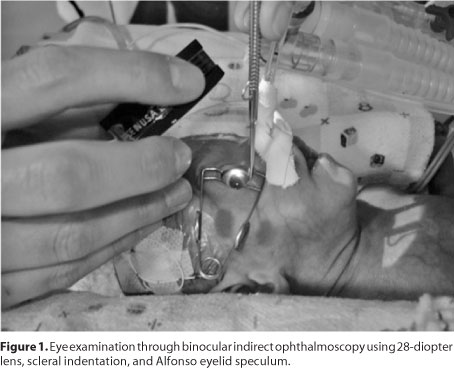
Binocular indirect ophthalmoscopy may be performed using 20-, 28-, or 30-diopter lenses. A newborn infant eyelid speculum, particularly the Alfonso Eye Speculum (Storz®, USA), (Figure 1), after topical ocular anesthesia with one drop of 0.5% proxy-metacaine chloride in each eye, and scleral indentation may be used to facilitate observation of abnormalities in zone III.
TREATMENT OF ROP
Peripheral avascular retinal cryotherapy was the treatment of choice for threshold ROP after 1988, due to the results from the Multicenter Trial of Cryotherapy for Retinopathy of Prematurity (CRYO-ROP), which confirmed that this treatment prevented ROP progression in a significant number of patients(23). Although cryotherapy is still largely used, transpupillary laser has become the method of choice in the treatment of ROP(24). The results of treatment with photocoagulation, using argon or diode laser, are encouraging and can halt disease progression in most patients.
Transpupillary laser treatment should be introduced at diagnosis of type 1 prethreshold ROP or, at worst, at threshold ROP. Type 1 prethreshold ROP usually occurs around the 36th postconceptional week, whereas threshold ROP usually develops between the 37th and 38th postconceptional week.
Current drug arsenal against ROP includes intravitreal anti-VEGF drugs. The drugs most commonly used in ophthalmology are bevacizumab (Avastin®), ranibizumab (Lucentis®), and pegaptanib (Ma-cugen®). Bevacizumab is the most widely used drug for the treatment of difficult cases of ROP. Since this drug is characterized by a larger molecule with shorter half-life within the eye, it is believed to pose less risk of iatrogenic injury to the preterm infants; however, there is plenty of room for further research on this subject. The administration of bevacizumab is best indicated in patients who develop ROP in zone I or in more posterior zone II. In these extremely severe cases, the current approach consists in performing anti-VEGF treatment prior to laser treatment, since photocoagulation leads to the breakdown of the blood-retinal barrier, causing the drug to be eliminated from the vitreous in a shorter time (lower therapeutic effect and poorer results) and also allowing further systemic spread of the drug with potential side effects that are still poorly known(25-27). The recent published results of the BEAT-ROP cooperative study regarding the efficacy of intravitreal bevacizumab for acute stage 3 plus ROP as monotherapy in patients with zone I disease (when compared with conventional laser therapy) showed significant reduction in the recurrence rate of the retinal neovascularization from 42% to 6%. Thus, this controlled study showed superior efficacy of intravitreal bevacizumab over laser therapy as measured by means of disease recurrence and abnormal retinal structural outcomes in patients with ROP in zone I. This represents a true breakthrough in the disease management(28).
PROGNOSIS OF ROP
ROP usually regresses in most stage 1 and 2 patients, since peripheral retina can get fully vascularized within the weeks following premature birth, leaving few residual anatomical and functional changes. Approximately 90% of patients at these stages show spontaneous disease involution and do not require specific treatment. These patients only need progressive follow-up during the first years of life to prevent amblyopia and strabismus and to correct ametropias, whose incidence appears to be greater in preterm babies when compared with nonpremature infants(29).
When ROP reaches stage 3 threshold disease or type 1 prethreshold disease, the patients require treatment, since 50% of patients at threshold disease and more than 15% of patients at type 1 prethreshold disease will have unfavorable anatomical and functional outcomes without appropriate treatment(30).
Prognosis of treatment with cryotherapy or diode laser photocoagulation in threshold disease patients is good and can prevent visual loss in about 70 to 80% of patients, presently(31). However, many children who undergo treatment show subsequent unsatisfactory visual acuity due to residual anatomical changes likely to affect macular region or due to strabismus, amblyopia, or high ametropia(31).
INCIDENCE AND PREVALENCE OF ROP IN BRAZIL
In Brazil, Graziano et al.(32), in 1997, prospectively analyzed data from 102 patients with BW <1,500 grams. The authors detected the occurrence of 29.9% of ROP, including all stages and drew attention to the high prevalence of ROP (78.5%) among patients with BW <1,000 grams and to the 72.7% of ROP in babies <30 weeks' GA. The study concluded that children with BW <1,000 grams and GA <28 weeks were at greater risk of developing stage 3 ROP or even a more advanced stage of disease.
The prevalence of ROP found in prospective studies carried out at HCPA after 2002 also demonstrated high prevalence of ROP (45.6%) in infants with BW <1,000 grams or GA <30 weeks (40.3%)(33,34).
Studies using data from other regions of Brazil have also shown similar results(35-38).
PREVENTION TO REDUCE ROP-INDUCED BLINDNESS
The prevention of ROP comprises a set of measures centered in neonatal screening for timely detection and treatment of the disease, when necessary. According to Quinn(39), the questions that need to be raised and addressed are:
1) HOW DO YOU IDENTIFY THE POPULATION AT RISK FOR ROP?
It should be performed through the implementation of a screening program for the detection of ROP, with weekly ophthalmological assessments in the NICU including all infants at risk for ROP. Brazilian guidelines include patients with BW <1,500 grams and/or GA <32 weeks for southern and southeastern Brazil. In northern and northeastern Brazil, patients with larger BW and greater GA may be examined at the physician's discretion due to reports of ROP severe enough to require treatment in older babies in these regions. These criteria are not static and they should be tailored to each population group and need to be regularly reviewed(40).
2) HOW DO YOU IDENTIFY ROP THAT NEEDS TREATMENT?
Patients who develop type 1 prethreshold ROP or, at worst, threshold ROP, need to be treated promptly and before 37 weeks of postconceptional age.
3) WHAT IS THE IDEAL TREATMENT FOR ROP?
Diode laser transpupillary photocoagulation of the peripheral avascular retina is currently the gold standard for treatment of ROP in more anterior zone II or in zone III. Treatment should be performed between the 37th and 38th postconceptional week. Intravitreal antiangiogenic drugs should be introduced as adjuvant therapy after laser treatment in cases of progressive ROP or even prior to laser treatment in more severe cases of ROP in zone I or posterior zone II. AntiVEGF therapy should be initiated before 36 weeks of postconceptional age.
4) WHAT DO YOU DO WHEN TREATMENT FAILS?
Patients undergoing laser treatment should be followed weekly for monitoring of disease progression as long as there is evidence of plus disease. Regression of plus disease is usually observed within 2 weeks from treatment. If the disease persists 3 weeks after treatment, a second course of laser therapy should be considered by the ophthalmologist. Such situation has been reported to occur in 15 to 20% of treated cases. Confluent treatment is the goal of the second course of laser therapy in order to cover areas left untreated in the first session.
5) HOW DO YOU PREVENT SEVERE ROP BY BETTER CONTROLLING RISK FACTORS IN PRETERM INFANTS?
Phase 1 ROP may be inhibited by an effective monitoring of oxygen-therapy as soon after birth and specific control of RF that each potential ROP patient might show during their NICU stay.
CONCLUSIONS
Neonatal screening examination for detection of ROP, when performed between the 4th and 6th week after birth in VLBW and ELBW preterm infants, provides the best possibility of controlling the disease in those patients who are likely to develop irreversible ROP-related complications.
A collaborative effort involving neonatologists, ophthalmologists, and the nursing staff has contributed greatly to reduce the incidence of ROP in nearly all countries with high quality perinatal care.
Neonatologists play a crucial role in this setting by ensuring that each affected patient receives the best treatment available, according to the set of RF that they present individually, and also by ensuring that standards for oxygen supply and monitoring are followed in the NICU.
The role of the nursing staff is critical to a successful prevention of ROP-induced blindness, since these professionals, in addition to scheduling patients at birth, are present throughout the examination process and also participate actively in the recommendations to the patient's family about the importance of the follow-up examinations after discharge.
Adequate management of maternal risk factors to reduce the possibility of premature labor and a strict management of oxygen delivery since birth, in addition to neonatal screening programs have contributed greatly to reduce ROP-related childhood blindness worldwide, as well as in Brazil.
REFERENCES
1. Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, Zin A; International NO-ROP Group. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115(5): e518-25.
2. Wheatley CM, Dickinson JL, Mackey DA, Craig JE, Sale MM. Retinopathy of prematurity: recent advances in our understanding. Br J Ophthalmol. 2002;86(6):696-700.
3. Campbell K. Intensive oxygen therapy as a possible cause of retrolental fibroplasia; a clinical approach. Med J Aust. 1951;2(2):48-50.
4. Crosse VM. Retrolental fibroplasia. Ulster Med J. 1952;21(1):32-5.
5. Patz A. The role of oxygen in retrolental fibroplasia. Trans Am Ophthalmol Soc. 1968;66: 940-85.
6. Sola A, Chow L, Rogido M. [Retinopathy of prematurity and oxygen therapy: a changing relationship]. An Pediatr (Barc). 2005;62(1):48-63. Review. Spanish.
7. McGregor ML, Bremer DL, Cole C, McClead RE, Phelps DL, Fellows RR, Oden N; HOPE-ROP Multicenter Group. High Oxygen Percentage in Retinopathy of Prematurity study. Retinopathy of prematurity outcome in infants with prethreshold retinopathy of prematurity and oxygen saturation >94% in room air: the high oxygen percentage in retinopathy of prematurity study. Pediatrics. 2002;110(3):540-4.
8. Pierce EA, Foley ED, Smith LE. Regulation of vascular endothelial growth factor by oxygen in a model of retinopathy of prematurity. Arch Ophthalmol. 1996;114(10):1219-28. Erratum in Arch Ophthalmol. 1997;115(3):427.
9. Tin W, Milligan DW, Pennefather P, Hey E. Pulse oximetry, severe retinopathy, and outcome at one year in babies of less than 28 weeks gestation. Arch Dis Child Fetal Neonatal Ed. 2001;84(2): F106-10. Comment in Arch Dis Child Fetal Neonatal Ed. 2001; 84(3):F149. Arch Dis Child Fetal Neonatal Ed. 2001;85(1): F75. Arch Dis Child Fetal Neonatal Ed. 2001;84(3): F149-50. Arch Dis Child Fetal Neonatal Ed. 2001;85(1): F75-6.
10. York JR, Landers S, Kirby RS, Arbogast PG, Penn JS. Arterial oxygen fluctuation and retinopathy of prematurity in very-low-birth-weight infants. J Perinatol. 2004;24(2):82-7.
11. Chow LC, Wright KW, Sola A; CSMC Oxygen Administration Study Group. Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants? Pediatrics. 2003;111(2):339-45.
12. Hellström A, Carlsson B, Niklasson A, Segnestam K, Boguszewski M, de Lacerda L, et al. IGF-I is critical for normal vascularization of the human retina. J Clin Endocrinol Metab. 2002; 87(7):3413-6.
13. Hellström A, Engström E, Hard AL, Bertsson-Wikland K, Carlsson B, Niklasson A, et al. Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth. Pediatrics. 2003;112(5):1016-20.
14. Lermann VL, Fortes Filho JB, Procianoy RS. The prevalence of retinopathy of prematurity in very low birth weight newborn infants. J Pediatr (Rio J). 2006;82(1):27-32.
15. Wallace DK, Kylstra JA, Phillips SJ, Hall JG. Poor postnatal weight gain: a risk factor for severe retinopathy of prematurity. J AAPOS. 2000;4(6):343-7.
16. Löfqvist C, Andersson E, Sigurdsson J, Engström E, Hard AL, Niklasson A, et al. Longitudinal postnatal weight and insulin-like growth factor I measurements in the prediction of retinopathy of prematurity. Arch Ophthalmol. 2006;124(12):1711-8.Erratum in: Arch Ophthalmol. 2007;125(3):426.
17. Fortes Filho JB, Bonomo PP, Maia M, Procianoy RS. Weight gain measured at 6 weeks after birth as a predictor for severe retinopathy of prematurity: study with 317 very low birth weight preterm babies. Graefes Arch Clin Exp Ophthalmol. 2009;247(6):831-6.
18. Härd AL, Löfqvist C, Fortes Filho JB, Procianoy RS, Smith L, Hellström A. Predicting proliferative retinopathy in a Brazilian population of preterm infants with the screening algorithm WINROP. Arch Ophthalmol. 2010;128(11):1432-6.
19. Fortes Filho JB, Eckert GU, Valiatti FB, Dos Santos PG, da Costa MC, Procianoy RS. The influence of gestational age on the dynamic behavior of other risk factors associated with retinopathy of prematurity (ROP). Graefes Arch Clin Exp Ophthalmol. 2010;248(6): 893-900.
20. Zin A, Florêncio T, Fortes Filho JB, Nakanami CR, Gianini N, Graziano RM, Moraes N. Proposta de diretrizes brasileiras do exame e tratamento de retinopatia da prematuridade (ROP). Arq Bras Oftalmol. 2007;70(5):875-83.
21. Costa MC, Eckert GU, Valiatti FB, Bonomo PP, Fortes Filho JB. Incidência da retinopatia e a participação da enfermagem na prevenção da cegueira pela retinopatia da prematuridade no Hospital de Clínicas de Porto Alegre: estudo prospectivo observacional descritivo. Online Braz J Nurs (Online). 2007;6(3).
22. Laws DE, Morton C, Weindling M, Clark D. Systemic effects of screening for retinopathy of prematurity. Br J Ophthalmol. 1996;80(5):425-8.
23. Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1988;106(4):471-9.
24. Pearce IA, Pennie FC, Gannon LM, Weindling AM, Clark DI. Three year visual outcome for treated stage 3 retinopathy of prematurity: cryotherapy versus laser. Br J Ophthalmol. 1998;82(11):1254-9.
25. Mintz-Hittner HA. Avastin as monotherapy for retinopathy of prematurity. J AAPOS. 2010;14(1):2-3. Comment on J AAPOS. 2010;14(1):6-10.
26. Mintz-Hittner HA, Kuffel RR Jr. Intravitreal injection of bevacizumab (avastin) for treatment of stage 3 retinopathy of prematurity in zone I or posterior zone II. Retina. 2008; 28(6):831-8. Erratum in Retina. 2008;28(9):1374.
27. Travassos A, Teixeira S, Ferreira P, Regadas I, Travassos AS, Esperancinha FE, et al. Intravitreal bevacizumab in aggressive posterior retinopathy of prematurity. Ophthalmic Surg Lasers Imaging. 2007;38(3):233-7.
28. Reynolds JD. Bevacizumab for retinopathy of prematurity. N Engl J Med. 2011;364(7):677-8. Comment in N Engl J Med. 2011;364(24):2360-1; author reply 2362. N Engl J Med. 2011;364(24):2359; author reply 2361-2. N Engl J Med. 2011;364(7):603-15.
29. Robinson R, O'Keefe M. Follow-up study on premature infants with and without retinopathy of prematurity. Br J Ophthalmol. 1993;77(2):91-4.
30. Good WV, Hardy RJ. The multicenter study of Early Treatment for Retinopathy of Prematurity (ETROP). Ophthalmology. 2001;108(6):1013-4.
31. Holmström G, Larsson E. Long-term follow-up of visual functions in prematurely born children-a prospective population-based study up to 10 years of age. J AAPOS. 2008;12(2):157-62.
32. Graziano RM, Leone CR, Cunha SL, Pinheiro AC. Prevalência da retinopatia da prematuridade em recém-nascidos de muito baixo peso. J Pediatr (Rio J). 1997;73(6): 377-82.
33. Fortes Filho JB, Eckert GU, Valiatti FB, da Costa MC, Bonomo PP, Procianoy RS. Prevalence of retinopathy of prematurity: an institutional cross-sectional study of preterm infants in Brazil. Rev Panam Salud Publica. 2009;26(3):216-20.
34. Fortes Filho JB, Eckert GU, Procianoy L, Barros CK, Procianoy RS. Incidence and risk factors for retinopathy of prematurity in very low and in extremely low birth weight infants in a unit-based approach in southern Brazil. Eye (Lond). 2009;23(1):25-30.
35. Bonotto LB, Moreira ATR, Carvalho DS. Prevalência de retinopatia da prematuridade em prematuros atendidos no período de 1992-1999 em Joinville (SC): avaliação de riscos associados - "screening". Arq Bras Oftalmol. 2007;70(1):55-61.
36. Pinheiro AM, Silva WA, Bessa CGF, Cunha HM, Ferreira MAF, Gomes AHB. Incidência e fatores de risco da retinopatia da prematuridade no Hospital Universitário Onofre Lopes, Natal (RN) - Brasil. Arq Bras Oftalmol. 2009;72(4):451-6.
37. Schumann RF, Barbosa ADM, Valete CO. Incidência e gravidade da retinopatia da prematuridade e sua associação com morbidade e tratamentos instituídos no Hospital Universitário Antonio Pedro, entre 2003 a 2005. Arq Bras Oftalmol. 2010;73(1):47-51.
38. Shinsato RN, Paccola L, Goncalves WA, Barbosa JC, Martinez FE, Rodrigues MLV, Jorge R. Frequência de retinopatia da prematuridade em recém-nascidos no Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo. Arq Bras Oftalmol. 2010;73(1):60-5.
39. Quinn GE. The 'ideal' management of retinopathy of prematurity. Eye (Lond). 2005;19(10): 1044-9.
40. Zin AA, Moreira ME, Bunce C, Darlow BA, Gilbert CE. Retinopathy of prematurity in 7 neonatal units in Rio de Janeiro: screening criteria and workload implications. Pediatrics. 2010;126(2): e410-7.
 Correspondence address:
Correspondence address:
João Borges Fortes Filho
Department of Ophthalmology. Medical School, Federal University of Rio Grande do Sul and Hospital de Clínicas de Porto Alegre
Rua Ramiro Barcelos, 2350
Porto Alegre - RS
90035-903 - Brazil
E-mail: [email protected]
Submitted for publication: March 3, 2011
Accepted for publication: April 10, 2011
Study carried out at the Department of Ophthalmology of Hospital de Clínicas de Porto Alegre. Brazil.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: J.B.Fortes Filho, None; G.U.Eckert, None; M.B.Taratarella, None; R.S.Procianoy, None.