

Regina de Souza Carvalho1; Newton Kara-José2; Newton Kara-Junior3
DOI: 10.1590/S0004-27492010000500007
ABSTRACT
PURPOSE: To check the occurrence of post-visit, the patient's understanding and the assessments of the doctor on duty about the efficacy of the process, at the ophthalmology emergency sector. METHODS: It was conducted a transversal, analytical research among doctors on duty and patients being seen consecutively in the ophthalmology emergency sector of Hospital das Clínicas da Universidade de São Paulo. RESULTS: The sample was made of 28 doctors on duty and 561 patients, 51.3% male and 48.7% female, with a mean age of 39.8 years old. From 34.1% of the patients who were previously seen by other sectors, 8.4% looked for two services and 5.7% three or more services. In the previous visits, 56.9% of the patients mentioned that they did not receive any explanation about their diagnostic. From the patients seen at Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo - FMUSP, 95.1% mentioned that the ophthalmologists explained the diagnostic and from those 84.0% understood what was explained. Among 40.4% of the patients who received medicine prescriptions in the previous services, 85.5% mentioned that they received explanation about its use and 82.9% followed the orientation. At Hospital das Clínicas - FMUSP 95.0% of the patients understood how and why to use the medicine. At the ophthalmologists point of view, more than 90.0% of the patients understood the diagnostic and the prescribed treatment. CONCLUSION: According to this research, for most of the patients, it was provided post-visit orientation and patients' understanding about the disease and the treatments proposed.
Keywords: Emergency Service, Hospital; Eye Diseases; Referral and consultation; Physician-patient relations; Emergency medical services
RESUMO
OBJETIVO: Verificar a ocorrência de pós-consulta, a compreensão pelo paciente e a avaliação do plantonista sobre a eficácia do processo, em pronto-socorro de oftalmologia. MÉTODOS: Foi realizada pesquisa transversal, analítica em plantonistas e pacientes atendidos consecutivamente no pronto-socorro de oftalmologia do Hospital das Clínicas da Universidade de São Paulo. RESULTADOS: A amostra foi composta por 28 plantonistas e 561 pacientes, 51,3% do sexo masculino e 48,7% do sexo feminino, com média de idade de 39,8 anos. Dos 34,1% pacientes que passaram previamente por outros serviços, 8,4% procuraram dois serviços e 5,7% três ou mais serviços. No atendimento dos serviços prévios, 56,9% dos pacientes mencionaram não ter recebido explicação sobre o diagnóstico. Dos pacientes atendidos no Hospital das Clínicas da FMUSP, 95,1% referiram que os oftalmologistas explicaram o diagnóstico e desses 84,0% entenderam o que foi explicado. Dentre os 40,4% pacientes que receberam prescrição de medicação nos serviços prévios, 85,5% mencionaram terem recebido explicação do seu uso e 82,9 % seguiram a orientação. No Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - FMUSP, 95,0% dos pacientes entenderam como e porque usar a medicação. Na percepção dos oftalmologistas, mais de 90,0% dos pacientes entenderam o diagnóstico e o tratamento prescrito. CONCLUSÃO: Nas condições desta pesquisa, para grande maioria dos pacientes, houve o fornecimento de orientação pós-consulta e a compreensão do paciente sobre a doença e tratamento propostos.
Descritores: Serviço Hospitalar de Emergência; Oftalmopatias; Referência e consulta; Relações médico-paciente; Serviços médicos de emergência
ORIGINAL ARTICLES ARTIGOS ORIGINAIS
Post-visit at ophthalmology emergency service: frequency and perception of the doctors on duty and users
Pós-consulta em serviço de emergência oftalmológica: frequência e percepção dos plantonistas e usuários
Regina de Souza CarvalhoI; Newton Kara-JoséII; Newton Kara-JuniorIII
IPedagogue, Faculdade de Medicina da Universidade de São Paulo - USP - São Paulo (SP), Brazil
IIPhysician, Faculdade de Medicina da Universidade de São Paulo e Faculdade de Ciências Médicas da Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
IIIPhysician, Faculdade de Medicina da Universidade de São Paulo - USP - São Paulo (SP), Brazil
ABSTRACT
PURPOSE: To check the occurrence of post-visit, the patient's understanding and the assessments of the doctor on duty about the efficacy of the process, at the ophthalmology emergency sector.
METHODS: It was conducted a transversal, analytical research among doctors on duty and patients being seen consecutively in the ophthalmology emergency sector of Hospital das Clínicas da Universidade de São Paulo.
RESULTS: The sample was made of 28 doctors on duty and 561 patients, 51.3% male and 48.7% female, with a mean age of 39.8 years old. From 34.1% of the patients who were previously seen by other sectors, 8.4% looked for two services and 5.7% three or more services. In the previous visits, 56.9% of the patients mentioned that they did not receive any explanation about their diagnostic. From the patients seen at Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo - FMUSP, 95.1% mentioned that the ophthalmologists explained the diagnostic and from those 84.0% understood what was explained. Among 40.4% of the patients who received medicine prescriptions in the previous services, 85.5% mentioned that they received explanation about its use and 82.9% followed the orientation. At Hospital das Clínicas - FMUSP 95.0% of the patients understood how and why to use the medicine. At the ophthalmologists point of view, more than 90.0% of the patients understood the diagnostic and the prescribed treatment.
CONCLUSION: According to this research, for most of the patients, it was provided post-visit orientation and patients' understanding about the disease and the treatments proposed.
Keywords: Emergency Service, Hospital; Eye Diseases; Referral and consultation; Physician-patient relations; Emergency medical services.
RESUMO
OBJETIVO: Verificar a ocorrência de pós-consulta, a compreensão pelo paciente e a avaliação do plantonista sobre a eficácia do processo, em pronto-socorro de oftalmologia.
MÉTODOS: Foi realizada pesquisa transversal, analítica em plantonistas e pacientes atendidos consecutivamente no pronto-socorro de oftalmologia do Hospital das Clínicas da Universidade de São Paulo.
RESULTADOS: A amostra foi composta por 28 plantonistas e 561 pacientes, 51,3% do sexo masculino e 48,7% do sexo feminino, com média de idade de 39,8 anos. Dos 34,1% pacientes que passaram previamente por outros serviços, 8,4% procuraram dois serviços e 5,7% três ou mais serviços. No atendimento dos serviços prévios, 56,9% dos pacientes mencionaram não ter recebido explicação sobre o diagnóstico. Dos pacientes atendidos no Hospital das Clínicas da FMUSP, 95,1% referiram que os oftalmologistas explicaram o diagnóstico e desses 84,0% entenderam o que foi explicado. Dentre os 40,4% pacientes que receberam prescrição de medicação nos serviços prévios, 85,5% mencionaram terem recebido explicação do seu uso e 82,9 % seguiram a orientação. No Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - FMUSP, 95,0% dos pacientes entenderam como e porque usar a medicação. Na percepção dos oftalmologistas, mais de 90,0% dos pacientes entenderam o diagnóstico e o tratamento prescrito.
CONCLUSÃO: Nas condições desta pesquisa, para grande maioria dos pacientes, houve o fornecimento de orientação pós-consulta e a compreensão do paciente sobre a doença e tratamento propostos.
Descritores: Serviço Hospitalar de Emergência; Oftalmopatias; Referência e consulta; Relações médico-paciente; Serviços médicos de emergência.
INTRODUCTION
The medical visit is a representative moment in the doctor-patient relationship, consisting of history collection of the patient (anamnesis), physical exam, diagnostic impression formulation, prescription and therapeutic explanation to be used(1).
The word visit, with a wide significance, can be perceived as "to have listening for your complaints", to get advice, to meditate. The two first designations mean the relationship of the patient with the professional, integrating an action of externalization-talk about yourself, and other of internalization-listening what the other person is saying(2).
The doctor-patient relationship is considered a key aspect in a medical visit. It has effects not only in the users' satisfaction, but also exerts direct influence over its health state(3).
The interaction between patient and professional will depend on, in one side, factors related to the patient: his/her need, therapeutic in use, his/her expectations, believes, fears and concerns, psychosocial and educational conditions, and his/her previous experiences with other physicians and, on the other side, factors related to the Health professional: the influence of other professionals, his/her personality, his/her psychological factors (stress, anxiety, frustration, communication difficulty), his/her technical training (professional experience and skills) and his/her human side(4).
The efficient interchange of information between the patient and the Health professional is very important to the comprehension, acceptance, adherence to the recommendations and clinical results(5).
The final moment of the visit, when the doctor explains to the patient about the disease and the procedure to be used, requires competence, patience, use of appropriate language and time to listen and answer to the patient about the possible doubts he/she may have.
In a research accomplished in 2001, the author states that it is hard to understand the scarce number of publications, either nationally or internationally, related to the ophthalmologic patients' emotional reactions and the peculiarities of the doctor-patient relationship(6).
This study notices the occurrence of post-visit orientation, the patients' understanding and the assessment of the doctor on duty about the efficacy of the process, at ophthalmology emergency sectors.
METHODS
An analytical transversal research was performed with patients seen at the Ophthalmology Emergency Room (ER) of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - HC-FMUSP, for one week considered as "typical", (01 to 08/04/2006) and doctors on duty(5).
It is considered that the better practical period for data collection of activities production is the "typical week", as it presents a definite and representative time of activities production they want to assess(7). So, it is possible to get data which enable to know the situation and which allow building a baseline for the assessment process.
It was set a non-probabilistic sample, promptly accessible, formed by subjects attended and doctors on duty of the mentioned service.
The research instrument was made of two semi-structured questionnaires. The first one, was applied by interviewers (nurses), previously trained. The second one was directly completed by the ophthalmologist on duty.
The application of the questionnaires was performed within the week from April 1st, 2006 to April 8th, 2006, comprehending 24 hours a day.
The patients were interviewed in two time points: in the first one, within the waiting period previous to the visit and in the second one, out of the visit place, at the hospital exit. The ophthalmologists did not know about the questionnaire applied to the patients.
For the ophthalmologists' answers, the questionnaire was directly completed in the exam room, after the patient's visit, without his/her presence. There were included in the study, all patients sawn within the period and who agreed to participate and all ophthalmologists on duty.
Patients who presented communication problems or were < 14 years old were assisted by the company and/or responsible. Patients who had: lucidity loss; with multiple traumatisms and those who refused to participate were excluded.
The diagnostics were classified and distributed into five categories: trauma, inflammation and/or infection, degenerative diseases, "other ophthalmologic diagnostics"(8) and with no "ocular changes". Return cases were mentioned, but did not enter in the mentioned categories.
People interviewed and the ophthalmologists were asked about the availability and acceptance in participating of the research and informed, in writing, upon an Informed Consent Form, that the participation was voluntary. For the patients it was renewed that the participation would not affect the visit waiting time and that the refusal would not provoke in any damage to the medical visits. The information obtained was typed in a database using the program EpiData (version 9.0). For statistical analysis, it was allowed a significance level of p0.05. The research was approved by the Research Ethics Committee/Investigational Review Board of Hospital das Clínicas da FMUSP nº 530/05.
RESULTS
The sample had 28 doctors on duty (2 doctors on duty for each period of 12 hours) and 561 patients (95.2% from those who were present at the service during the week of research), being 51.3% male and 48.7% female. The age of the patients ranged from 27 days to 91 years old (mean=39.8 years old; standard deviation=20.9 years old). Sixty-three (11.3%) patients did not attend school and 301 (53.9%) concluded the elementary school. Diagnostic of 549 (97.9%) from the 561 cases was obtained. Three hundred and three (55.2%) were in the diagnostic group of inflammation/infection; 19.1% trauma. A group of 3.6% did not present ocular changes and 1.1% of the patients were considered as follow-up visits.
One hundred ninety-one patients referred that they looked for other services before going at the Ophthalmology ER of HC-FMUSP; 85.9% looked for only one service, 8.4% looked for two services, 3.1% looked for three services, and 2.6% looked for four services or more.
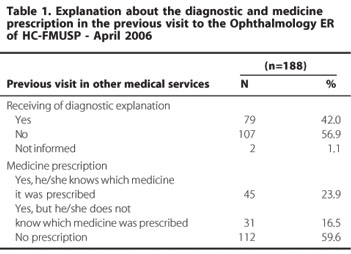
One hundred and eighty-eight (188) patients answered to questions concerned other received treatments (Table 1). From those patients, 79 (41.8%) mentioned that explanation about the diagnostic was given in the only (or last) medical service they looked for. Seventy-six (76) patients (40.4%) referred that some medicine was prescribed in this service (Table 1).
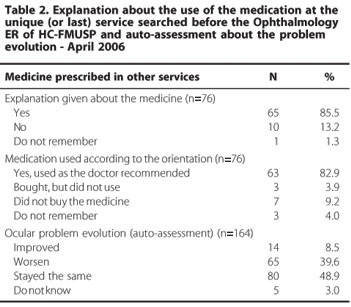
Among the patients who mentioned that received a prescription of some medicine, 65 (85.5%) declared that they received explanations about how to use it and 63 (82.9%) mentioned that they used it as recommended. One hundred and sixty-four patients (87.2%) assessed the problem evolution after they looked for another service. Approximately 50.0% referred worsen of the symptoms or remained the same (Table 2).
Five hundred and nine (90.7%) patients answered the questions that assessed the explanations given by the doctors who examined him/her at the Ophthalmology ER of HC-FMUSP during the typical week. From those, 484 (95.1%) reported that the doctor explained to them what they had in the eyes (Table 3). The explanation was understood by 404 (84.0%) patients who stated that received some explanation.
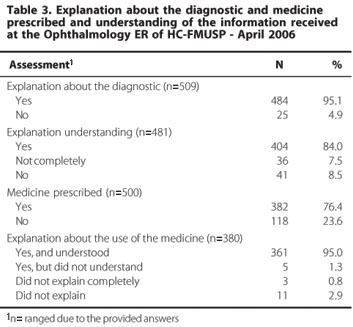
Five hundred (89.1%) patients answered whether they had received or not prescription of some medicine. From these, 382 (76.4%) received prescription of some medicine. Among those who received prescription of some medicine, 361 (95.0%) understood how and why to use it (Table 3).
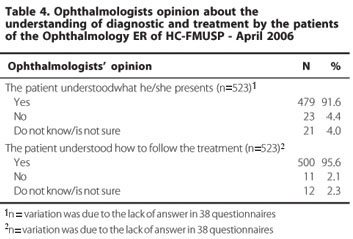
According to the ophthalmologists, more than 90% of the patients understood their diagnostics and how to follow the prescription (Table 4).
DISCUSSION
Medical exam is completed with the post-visit. Both determine the adherence degree and patient satisfaction.
In a research with general practioners, surgeons and patients in the United States of America, the authors referred that the patients give much value to the interest, attention, advices and information given by the doctor during the visit(9).
Doctor-patient relationship is extremely complex as it depends on several variables, such as communication, availability, tolerance, but two factors are crucial: understanding and confidence(10).
In an Emergency Room, the doctor-patient relationship can suffer additional interferences from the great demand, not much time to see the patient, stress related to the emergency process, lack of suitable physical structure for the visit, constant movement and internal organization problems from this type of service.
It is also important to highlight that the available time for the ER visit is not enough for the patient to express his/her doubts and to get answers(11).
The ER of HC-FMUSP received 28.585 patients in the year previous to this research, representing 13.6% of the service of the entire ER HC, counting on with only one ophthalmologist on duty, one resident and one assistant at each shift(12).
Even in this limited setting for a proper doctor-patient relationship, 95.1% of the patients seen at the Ophthalmology ER of HC-FMUSP mentioned that the doctors on duty explained "what had in the visits", and from those 84.0% understood what was explained (Table 3).
From the 34.1% of the patients who visited other services previous to the ER of HC-FMUSP, 56.9% mentioned that they did not received explanations about the diagnostic (Table1).
In a study about the quality of assistance and satisfaction of the patient in a university hospital, it was noticed that 45.3% of the outpatient service stated that they did not received orientation during the post-visit(13).
Japanese researchers in 1999(14) mentioned the lack of orientation in the post-visit; the disability of some doctors in explaining or of some patients in understanding; the uncertainty of the diagnostic and the prescribed treatment, and a certain degree of psychic changes diagnosed, lead the patient to look for a second opinion. They also mentioned that, from the 40.0% of the patients who looked for a second opinion, 21.9% went to more than two places(14).
In this research, from the 34.1% of the patients who visited other services previously to HC, 85.9% looked for one service, 8.4% looked for two services, 3.1% looked for three services, and 2.6% looked for four services or more. Patients who search for opinions in different services are not satisfied with the obtained results and/or need better explanations about the disease and treatment proposed. It is important to notice that, from the patients who searched other services, 48.9% mentioned that "their visits were the same"; 39.6% referred worsening of the status after the treatment and only 8.5% referred improvement (Table 2). The lack of explanation about how to act provokes few or none adherence to the medical prescription, postponing the effective treatment and overloading the reference centers.
A research conducted in the ER of UNICAMP, reported that 87.5% of the patients coming from other services were unnecessarily referred to specialized reference centers and/or came by their own initiative to check the treatment, which shows little confidence in the first service(15).
In Brazil, researchers(16) found that 32.0% of patients in the ophthalmologic sector were searching for a second opinion, being the main reasons of this management: confirmation of the diagnostic (43.0%); lack of confidence in the first doctor (33.0%) and perception of lack of interest from the professionals (24.0%).
Information exchange between professional and patient should be encouraged to make the patients participation in the treatment process effectively collaborative.
A 2000 study noticed the importance of physicians as prescribers, since the prescription is based on the interpretation of what patients inform(17). Patients importance lays on the description of what he/she is feeling and if he/she will adhere the medical indication or not.
The physician should use an appropriate language in order to make the patient understand his/her problem and the proposed treatment, keeping in mind that there is a difference between what the physician explained and what the patient understood. Frequently, patients do not understand what physicians explain, and do not express themselves in a way physicians understand his/her doubts and complaints.
It is noticed in this paper that even with the diagnostic clarification, 4.9% of the patients said that they did not receive any explanation and 16.0% understood a bit or did not understand the provided explanation (Table 3), totalizing 20.9% of patients who need better clarifications. However, in the ophthalmologists' opinion, only 4.4% of the patients did not understand the explanations about the diagnostic and the physicians are not sure about the real understanding of 4.0% of the patients (Table 4).
It is worth to emphasize that 95% of the patients understood how and why to use the prescribed medicine, however, 2.1% did not understand or poorly understood what was prescribed, and 2.9 % mentioned that did not receive explanations about the medicine use (Table 3). Those patients will have a lower adherence to the treatment, consequently, none or low resolution capability; and probably will look for another service.
It is important to evaluate the reason of this lack of communication and to improve supplement in this process. The lack of understanding of the problem and its treatment can postpone its resolution, worsen the disease and lead to the search of other opinion, with damages to the subject's health and higher expenses of the public service. On the other side, the service and the hospital are subjected to lawsuit of the Medical Ethics Code(18-19), which states that the doctor on duty needs to provide necessary information and to obtain the patient and/or his/her family comprehension.
The emergency services can use strategies as provision of written material, assessment of patients' perception; continuous improvement of the doctor on duty who, besides providing a technical-diagnostic support, should increase in value the doctor-patient relationship through communication and pursuance of strategies together with the patient to easy the understanding of the required care to promote adequate ocular health. They can also use nurse assistants, nurses and ophthalmology assistants duly trained and supervised by the doctor on duty to perform the post-visit when the patients flow is exacerbated(20).
A 1991 survey(21) verified that users feel better assisted at hospitals (private, medical insurance or not), followed by public emergency services. The authors registered the importance attributed to the "good relationship between doctor and patient" in the service assessment. The establishment of human relationships with patients contribute to develop the feeling of medical responsibility, as well as to improve the results and the treatment adherence, increasing patients satisfaction degree(22).
In this study, from the patients who received drugs prescription in other services, 85.5% informed that received explanation about how to use the medicine (Table 1 and 2). However, 17.1% of the patients did not adhere the treatment because they did not follow correctly the doctor guidelines; did not buy the medicine or did not remember to use the drug (Table 2).
Probably, some of the 39.6% of the patients who mentioned worsening of the symptoms or that remained unchanged (48.9%) after the previous service visit (Table 2) have not used the medicine as explained.
Patients understanding about ocular disease concepts, their believes and medicine used is deficient as well as in relationship to the ability required to use the medicine and actions to a better disease control, renewing the need of constant educational intervention and well trained professionals for health care(23).
In a study performed at a university hospital emergency(24), it was found that 29.4% of the patients use homemade products as the first management for the treatment of ocular diseases. Information about what people know and do regarding ocular problems is an important data for prevention and educational health programs(25). The post-visit should stimulate the adoptions of correct managements before appeals.
Researchers(4) mentioned that the medical education is mainly guided to aspects related to anatomy, physiology, clinics, and pathology, not considering the history of the diseased and the moral and psychological support. In order to have a better doctor-patient relationship, there is a need to check the physician's attitude, his or her professional background and graduation.
It is important to emphasize the greater responsibility of HC-FMUSP ER as, besides the service rendered to the patients; it is a standard for residents and fellows who will have their future management influenced by the system where they have learned to interact with others.
One of the differences between a college and a university is the greater responsibility the latter has regarding education, service rendering, researches, and communities problems(26). The university should examine the type of health assistance that is being offered to the community on its influence area. Without those data, it is not possible to provide health managers reproducible templates to solve problems. The assessment which can indicate the formation model to be taught to Medicine and post-graduation students can also be impaired.
CONCLUSION
Most of the patients seen at the Emergency Room of Hospital das Clínicas da Universidade de São Paulo considered that they were well guided at the post-visit about the diagnostic and the prescribed treatment. However, 20.9% considered that they were not guided or did not understand what they had in the eyes. According to the ophthalmologists, more than 90% of the patients understood their diagnostics and how to comply with the treatment.
A considerable number of patients came for a second opinion, and most of them mentioned that they did not receive orientation about the disease and its treatment.
Notes: This study, despite the representative number of the assessed cases, collected information from patients who visited the Ophthalmology ER of HC-FMUSP and thus cannot be generalized to all Brazilian Ophthalmology ERs.
The cases of second opinion represent only those unsatisfied and do not present evidenced relationship with the total of patients previously seen at ER-HC FMUSP.
REFERENCES
1. Conselho Regional de Medicina do Estado da Bahia-CREM. Parecer Nº 23/02. Remuneração de revisão de consulta médica. 6 de 6 de 2002. J CREMEB; 23 de fevereiro de 2002. [citado 2009 Set 26]. Disponível em: http://www.portalmedico.org.br/pareceres/crmba/pareceres/2002/23-2002.htm
2. Rezende TB. Idosos e a consulta médica. Um estudo de representações sociais. [tese] Rio de Janeiro: Universidade Federal do Rio de Janeiro; 2003.
3. Caprara A, Rodrigues J. A relação assimétrica médico-paciente: repensando o vínculo terapêutico. Ciênc Saúde Coletiva. 2004;9(1):139-46.
4. Caprara A, Franco LSA. A relação paciente-médico: para uma humanização da prática médica. Cad Saúde Pública. 1999;15(3):647-54.
5. Carvalho RS. Conduta leiga e assistência médica em pacientes do Pronto-Socorro de Oftalmologia do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. [tese] São Paulo: Faculdade de Medicina, Universidade de São Paulo; 2007. http://www.teses.usp.br/teses/disponiveis/5/5149/tde-25032009-145309/
6. Rodrigues CRC. Relação médico-paciente. In: Rodrigues MLV, Dantas AM. Oftalmologia clínica. 2ª ed. Rio de Janeiro: Cultura Médica; 2001. p.1-8.
7. Tanaka OY, Melo CM. Avaliação de programas de saúde do adolescente. Um modo de fazer. São Paulo: EDUSP; 2001. p.10-5.
8. Edwards RS. Ophthalmic emergencies in a district general hospital casualty department. Brit J Ophthalmol. 1987;71(12):938-42.
9. Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553-9. Comment in: JAMA. 1997;277(21): 1682. JAMA. 1997;277(21):1681; author reply 1682.
10. Luz PL. Nem só de ciência se faz a cura. O que os pacientes me ensinaram. São Paulo: Atheneu; 2002. Capitulo 2, As dificuldades do prognóstico; p.23-32.
11. Sutherland LR, Verhoef MJ. Patients who seek a second opinion: are they different from the typical referral? J Clin Gastroenterol. 1989;11(3):308-13.
12. Carvalho RS, José NK. Ophthalmology emergency room at the University of São Paulo General Hospital: a tertiary hospital providing primary and secondary level care. Clinics (São Paulo). 2007;62(3):301-8.
13. Oliveira DF, Arieta CE, Temporini ER, Kara-José N. Quality of health care: patient satisfaction in a university hospital. Arq Bras Oftalmol. 2006;69(5):731-6.
14. Sato T, Takeichi M, Hara T, Koizumi S. Second opinion behavior among Japanese primary care patients. Br J Gen Pract. 1999;49(444):546-50.
15. Kara-Junior N, Zanatto MC, Villaça VT, Nagamati LT, Kara-José N. Aspectos médicos e sociais no atendimento oftalmológico de urgência. Arq Bras Oftalmol. 2001;64(1): 39-43.
16. Obeid WN, Vieira LA, Frangieh AY. Segunda opinião em Oftalmologia. Arq Bras Oftalmol. 2005;68(3):311-6.
17. Pepe VL, Castro CG. A interação entre prescritores, dispensadores e pacientes: informação compartilhada como possível benefício terapêutico. Cad Saúde Pública. 2000;16(3):815-22.
18. Conselho Federal de Medicina. Resolução CFM nº 1.246/88 de 08/01/88. Aprovar o código de ética médica. Diário Oficial da União; 26 de janeiro de 1988, art. 59 e 70. [citado 2009 Set 28]. Disponível em: http://www.portalmedico.org.br/resolucoes/cfm/1988/1246_1988.htm.
19. Conselho Regional de Medicina do Estado de São Paulo. Resolução publicada pelo CFM em 17 de setembro estabelece o novo código de ética Médica. J Cremesp. 2009; 263:9 de set. [citado 2009 Jul 21]. Disponível em: http://www.cremesp.org.br/?siteAcao=Jornal&id=1204
20. Oliveira RC, Kara-José N. Sucesso em Oftalmologia. In: Oliveira RC, Kara-José N. Auxiliar de oftalmologia. São Paulo: Roca; 2000. v.2, p.363-72 (Série Atualidades em Oftalmologia).
21. Cohn A, Nunes E, Jacobi PR, Karsch US. A saúde como direito e serviço. São Paulo: Cortez; 1991. v.7. (Série Pensamento Social e Saúde).
22. Kleinman A. Suffering and its professional transformation: toward an ethnography of interpersonal experience. Cult Med Psychiatry. 1991;15(3):275-301.
23. Rocha JC, Gondim EL, Braga FT, Dantas FJ, Temporini ER, Kara-José N. Ocular health myths among a hospital staff. Ophthalmic Epidemiol. 1997;4(2):107-13.
24. Carvalho RS, Kara-José N, Temporini ER, Kara-Junior N, Noma-Campos R. Self-medication: initial treatments used by patients seen in an ophthalmologic emergency room. Clinics (São Paulo). 2009;64(8):735-41.
25. Oliveira RS, Temporini ER, Kara-José N, Carricondo PC, Kara José A. Perceptions of patients about cataract. Clinics (São Paulo). 2005;60(6):455-60.
26. Kara-José N, Rangel FF, Barbosa NL. Perfurações do globo ocular e ferimentos da face. Necessidade de diagnóstico precoce. Arq Bras Oftalmol. 1982;45(2):66-9.
 Correspondence address:
Correspondence address:
Regina de Souza Carvalho
Rua Barão do Triunfo, 1.220 - Apto. 122
São Paulo SP - CEP 04602-005
E-mail: [email protected]
Recebido para publicação em 21.12.2009
Última versão recebida em 05.09.2010
Aprovação em 12.10.2010
The research was part of the Ph.D. Dissertation in Sciences presented to Faculdade de Medicina da Universidade de São Paulo, 2006; subsidized by Fundação de Amparo à Pesquisa do Estado de São Paulo - FAPESP - nº 55408-8.
Work carried out at the Emergency Sector of Hospital das Clínicas, São Paulo University School of Medicine - USP.
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência do Dr. Joaquim Pereira Paes sobre a divulgação de seu nome como revisor, agradecemos sua participação neste processo.