

Daniel Meira-Freitas1; Michel Eid Farah1; Ana Luisa Höfling-Lima1; Fabio Bom Aggio1
DOI: 10.1590/S0004-27492009000600019
ABSTRACT
The optical coherence tomography (OCT) and indocyanine green angiography (ICGA) findings of a 58-year-old male with acute syphilitic posterior placoid chorioretinitis are reported herein. Best-corrected visual acuity was 20/150 in the right eye (OD) and 20/30 in the left eye (OS) at presentation. On funduscopy, there was a central subretinal placoid yellowish lesion in OD. VDRL and serum FTA-ABS were positive. OCT showed increased reflectance and thickening of the subfoveal RPE-choriocapillaris complex corresponding to the lesion in OD. ICGA revealed a hypofluorescent spot corresponding to the lesion in OD and confluent small dots extending to periphery, without any correspondence in fundus examination. The same dots were also seen in OS, even though no lesions could be observed clinically. Intravenous ceftriaxone 2 g daily was given for 10 days. One month after the first visit, visual acuity improved to 20/30 and marked improvement of the lesion was seen. OCT was normal in both eyes at the final visit.
Keywords: Syphilis; Uveitis; Choroiditis; Tomography; optical coherence; Indocyanine green; Case reports
RESUMO
Relatamos aqui os achados da tomografia de coerência óptica (OCT) e angiografia com indocianina verde (ICGA) de um paciente masculino de 58 anos com a coroidopatia placóide posterior aguda sifilítica. A acuidade visual corrigida na apresentação foi de 20/150 no olho direito (OD) e 20/30 no olho esquerdo (OE). A fundoscopia evidenciou lesão sub-retiniana placóide amarelada central no OD. As sorologias VDRL e FTA-ABS foram positivas. OCT evidenciou aumento de refletividade subfoveal e espessamento do complexo EPR-coriocapilar correspondente à lesão do OD. ICGA revelou hipofluorescência local correspondente à lesão do OD e pequenos pontos confluentes que se estendiam para a periferia, sem qualquer correspondência na fundoscopia. O mesmo também foi visto no OE, embora nenhuma lesão pode ser observada clinicamente. Ceftriaxona 2 g intravenosa diária foi administrada durante 10 dias. Um mês após a primeira visita, a acuidade visual do OD foi 20/30 e melhora acentuada da lesão foi observada. Na última visita, o OCT foi normal em ambos os olhos.
Descritores: Sífilis; Uveíte; Coroidite; Tomografia de coerência óptica; Verde de indocianina; Relatos de casos
RELATOS DE CASOS
Optical coherence tomography and indocyanine green angiography findings in acute syphilitic posterior placoid choroidopathy: case report
Achados da tomografia de coerência óptica e angiografia com indocianina verde na coroidopatia placóide posterior aguda sifilítica: relato de caso
Daniel Meira-FreitasI; Michel Eid FarahII; Ana Luisa Höfling-LimaII; Fabio Bom AggioII
IDepartment of Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brazil
IIDepartment of Ophthalmology, UNIFESP - São Paulo (SP) - Brazil
ABSTRACT
The optical coherence tomography (OCT) and indocyanine green angiography (ICGA) findings of a 58-year-old male with acute syphilitic posterior placoid chorioretinitis are reported herein. Best-corrected visual acuity was 20/150 in the right eye (OD) and 20/30 in the left eye (OS) at presentation. On funduscopy, there was a central subretinal placoid yellowish lesion in OD. VDRL and serum FTA-ABS were positive. OCT showed increased reflectance and thickening of the subfoveal RPE-choriocapillaris complex corresponding to the lesion in OD. ICGA revealed a hypofluorescent spot corresponding to the lesion in OD and confluent small dots extending to periphery, without any correspondence in fundus examination. The same dots were also seen in OS, even though no lesions could be observed clinically. Intravenous ceftriaxone 2 g daily was given for 10 days. One month after the first visit, visual acuity improved to 20/30 and marked improvement of the lesion was seen. OCT was normal in both eyes at the final visit.
Keywords: Syphilis; Uveitis; Choroiditis; Tomography, optical coherence; Indocyanine green; Case reports
RESUMO
Relatamos aqui os achados da tomografia de coerência óptica (OCT) e angiografia com indocianina verde (ICGA) de um paciente masculino de 58 anos com a coroidopatia placóide posterior aguda sifilítica. A acuidade visual corrigida na apresentação foi de 20/150 no olho direito (OD) e 20/30 no olho esquerdo (OE). A fundoscopia evidenciou lesão sub-retiniana placóide amarelada central no OD. As sorologias VDRL e FTA-ABS foram positivas. OCT evidenciou aumento de refletividade subfoveal e espessamento do complexo EPR-coriocapilar correspondente à lesão do OD. ICGA revelou hipofluorescência local correspondente à lesão do OD e pequenos pontos confluentes que se estendiam para a periferia, sem qualquer correspondência na fundoscopia. O mesmo também foi visto no OE, embora nenhuma lesão pode ser observada clinicamente. Ceftriaxona 2 g intravenosa diária foi administrada durante 10 dias. Um mês após a primeira visita, a acuidade visual do OD foi 20/30 e melhora acentuada da lesão foi observada. Na última visita, o OCT foi normal em ambos os olhos.
Descritores: Sífilis; Uveíte; Coroidite; Tomografia de coerência óptica; Verde de indocianina; Relatos de casos
INTRODUCTION
Syphilis is caused by the spirochete Treponema pallidum. It can be transmitted through sexual contact, blood transfusion or via the transplacental route. The skin, heart, eyes, bones and nervous system may be affected.
The most common ocular finding of syphilis is uveitis, occurring in 2.5% to 5% of patients with tertiary syphilis(1). The presenting signs include focal retinitis, papillitis, iritis, keratic precipitates, periphlebitis, vitritis, as well as serous and exudative retinal detachment(2). Gass et al. described acute syphilitic posterior placoid chorioretinitis (ASPPC) in six patients with evidence of secondary syphilis that showed one or more large macular or peripapillary placoid lesions. It was proposed that the angiographic features of this entity were sufficiently conspicuous to suggest the diagnosis of secondary syphilis(3). Herein we report the optical coherence tomography (OCT) and indocyanine green angiography (ICGA) findings in a patient with ASPPC.
CASE REPORT
A 58-year-old heterosexual white male presented with one-week history of sudden painless central decrease of vision in his right eye (OD). Best-corrected visual acuity was 20/150 in OD and 20/30 in the left eye (OS). His pupils were briskly reactive to light, without afferent pupillary defect. Slit-lamp examination was unremarkable with no anterior chamber or vitreous inflammation. On funduscopy, there was a central subretinal placoid yellowish lesion in OD at the level of the retinal pigmented epithelium and a faded foveal reflex (Figure 1A). Funduscopy was normal in OS, except for mild hyperemia of the optic disc.
Humphrey perimetry (24-2 Swedish Interactive Threshold Algorithm Standard) testing revealed a generalized decrease of sensitivity on both eyes associated with extensive relative central scotoma in OD. Intravenous fluorescein angiography showed irregular early hyperfluorescence with temporal and superior areas of hypofluorescence due to blockage and late staining of the placoid lesion in OD (Figure 1B). OCT showed increased reflectance and thickening of the subfoveal RPE-choriocapillaris complex corresponding to the lesion in OD (Figure 1F).
At the third day of follow-up, the patient presented a deterioration of visual acuity in OD to counting fingers and a marked expansion of the lesion size. ICGA revealed a hypofluorescent area corresponding to the lesion in OD (Figure 1D), as well as hypofluorescent confluent small dots extending to the periphery in a radial pattern (Figure 1E), without any correspondence in fundus examination. The same was also seen in OS, even though no lesions could be observed clinically.
Based on the diagnostic hypothesis of acute posterior multifocal placoid pigment epitheliopathy, oral prednisone (40 mg daily) was prescribed. At the 10th day of follow-up, visual acuity improved to 20/80 in OD. Laboratory work-up became available, revealing positive both VDRL (1:128) and serum FTA-ABS. Serology was negative for HIV antibodies. Intravenous ceftriaxone 2 g daily was given for 10 days.
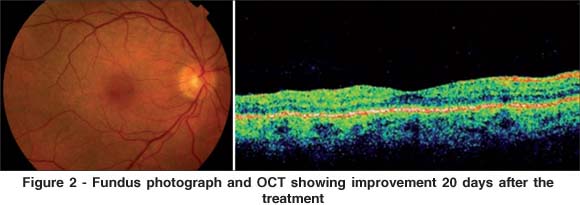
One month after the first visit, visual acuity was further improved to 20/30 and marked improvement of the lesion was seen (Figure 2). OCT was normal in both eyes.
DISCUSSION
Although initially thought to be specific of ocular syphilis in immunocompromised individuals(4-6), ASPPC has been described in HIV negative patients without any evidence of immunocompromise as well(1,7).
In accordance with other studies, fluorescein angiogram showed irregular initial hyperfluorescence with hypofluorescent spots and late staining of the lesion(3,5,7). The lesion was hypofluorescent on ICGA, with the characteristic leopard skin pattern(3) beyond its limits in OD. Interestingly, leopard spots in the peripapillary area and in the posterior pole were also present in OS, without any correspondence in fundus examination. These lesions may represent fibrin and inflammatory exudates at the level of the inner choroid and are consistent with a bilateral inflammatory process similar to that seen in white dot syndrome.
OCT findings revealed thickening of the foveal RPE-choriocapillaris band, suggesting involvement of these tissues as well, probably by means of contiguity. We postulate that transient functional compromise of the outer retina in the foveal area led to the severe reduction in visual acuity. Similar findings were also found in a patient with unilateral acute idiopathic maculopathy(8). On the other hand, Joseph et al. reported increased thickening of the neuroretina and underlying layers in one patient and subretinal fluid at the macula in another patient, with restoration of the normal chorioretinal architecture in both after treatment(9). These different patterns may occur as a result of the varied disease spectrum of syphilis.
Fundus and angiographic changes in ASPPC may mimic other chorioretinal diseases. It is important to distinguish the placoid lesions seen in ASPPC from those of acute posterior multifocal placoid pigment epitheliopathy (APMPPE), serpiginous choroiditis, and viral retinitis(10). Like syphilitic placoid lesions, APMPPE may occur in the posterior pole as a large, solitary and ephemeral lesion. Nevertheless, the syphilitic placoid disease may differ from APMPPE and others through the leopard spots seen on angiographic exams. It is possible that the pattern of inflammation that is supposed to reach the inner choroid via the optic nerve and secondarily affect the RPE and photoreceptors may be common to white dot syndrome and ASPPC.
In conclusion, ASPPC is a variant of ocular syphilis that has many features that share similarities with other idiopathic chorioretinal diseases, mainly white dot syndromes. ICGA showed a bilateral inflammatory process at the level of the inner choroid. OCT disclosed transient RPE-choriocapillaris thickening at the fovea, suggesting secondary involvement by contiguity.
REFERENCES
1. Aldave AJ, King JA, Cunningham ET Jr. Ocular syphilis. Curr Opin Ophthalmol. 2001;12(6):433-41.
2. Kuo IC, Kapusta MA, Rao NA. Vitritis as the primary manifestation of ocular syphilis in patients with HIV infection. Am J Ophthalmol. 1998;125(3):306-11. Comment in: Am J Ophthalmol. 1998;125(3):374-82. Am J Ophthalmol. 1998; 125(3):383-5. Am J Ophthalmol. 1998;125(3):411-5.
3. Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):1288-97.
4. Díaz-Valle D, Allen DP, Sánchez AA, Aguado CB, Benítez Del Castillo JM, Aceñero MJ. Simultaneous bilateral exudative retinal detachment and peripheral necrotizing retinitis as presenting manifestations of concurrent HIV and syphilis infection. Ocul Immunol Inflamm. 2005;13(6):459-62.
5. Ouano DP, Brucker AJ, Saran BR. Macular pseudohypopyon from secondary syphilis. Am L Ophthalmol. 1995;119(3):372-4.
6. Tran TH, Cassoux N, Bodaghi B, Fardeau C, Caumes E, Lehoang P. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005;243(9):863-9.
7. Baglivo E, Kapetanios A, Safran AB. Fluorescein and indocyanine green angiographic features in acute syphilitic macular placoid chorioretinitis. Can J Ophthalmol. 2003;38(5):401-5.
8. Aggio FB, Farah ME, Meirelles RL, de Souza EC. Stratus OCT and multifocal ERG in unilateral acute idiopathic maculopathy. Graefes Arch Clin Exp Ophthalmol. 2006;244(4):510-6.
9. Joseph A, Rogers S, Browning A, Hall N, Barber C, Lotery A, et al. Syphilitic acute posterior placoid chorioretinitis in nonimmuno-compromised patients. Eye. 2007;21(8):1114-9.
10. Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: reemergence of an old adversary. Ophthalmology. 2006;113(11):2074-9.
 Correspondence address:
Correspondence address:
Daniel Meira-Freitas
Rua Botucatu, 820 - São Paulo (SP)
CEP 04023-062
E-mail: [email protected]
Recebido para publicação em 08.05.2009
Última versão recebida em 07.07.2009
Aprovação em 14.07.2009
Trabalho realizado no Departamento de Oftalmologia da Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brazil.