

Rosana Zacarias Hannouche1; Marcos Pereira de Ávila2
DOI: 10.1590/S0004-27492009000400002
ABSTRACT
PURPOSE: 1) Diagnose, through optical coherence tomography (OCT) exam, the occurrence of diabetic macular edema in patients with diabetic retinopathy and visual acuity of 20/40 or better, by measuring the foveal center point thickness, during one year. 2) Evaluate the edema natural history, during this period, associating the center point thickness with hemoglobin A1c and changes in visual acuity. 3) Correlate the obtained results with the control group. METHODS: A prospective study was done, of a sample of 30 patients with diabetic macular edema and visual acuity of 20/40 or better. Measurements of the best corrected visual acuity, hemoglobin A1c level, biomicroscopy with 78-diopter lens, fluorescein angiogram and optical coherence tomography were made. The retinal thickness was selected as the main variable. Besides descriptive statistics, additional tests were applied to analyze the results and determine the correlation between these variables, such as t-Student, Chi-Square, Tukey and ANOVA. The relation of optical coherence tomography with visual acuity and hemoglobin A1c was studied through linear regression. RESULTS: It was found that there is no significant difference between patients and normal individuals, for the variables age and gender. The values of center point thickness found for men were greater than those for women, showing the influence of gender on that thickness. As many as 83.33% of the diabetic patients with clinically significant macular edema presented moderate non-proliferative diabetic retinopathy (NPDR), 10% presented mild NPDR and 6.66% severe non-proliferative diabetic retinopathy. Patients under combined treatment of insulin and oral hypoglycemiant presented influence on the results of center point thickness (through OCT) and visual acuity. The mean duration of diabetes was 9.63 years. Values of center point thickness were always found greater for patients than those for normal eyes. Levels of hemoglobin A1c did not have influence on the center point thickness data, whereas values of visual acuity were significantly correlated with it. CONCLUSION: This study presents the optical coherence tomography applicability in the detection and semiologic evaluation of diabetic macular edema in patients with visual acuity 20/40 or greater, during one year, showing the retinal thickening in the early stages of diabetic retinopathy. Further, it evidenciated the correlation between the increase in foveal thickness and the reduction in visual acuity. Levels of hemoglobin A1c did not influence the center point thickness data. An early detection of clinically significant macular edema leads us to a redefinition of the real meaning of incipient retinopathy and can prevent further significant reduction of vision.
Keywords: Diabetic retinopathy; Macular edema; Tomography, optical coherence; Light coagulation; Fovea centralis; Visual acuity
RESUMO
OBJETIVOS: 1) Diagnosticar a presença de edema macular diabético em pacientes com retinopatia diabética e acuidade visual igual ou melhor que 20/40, pela realização do exame de tomografia de coerência óptica, medindo a espessura foveal central, ao longo de um ano. 2) Avaliar a história natural do edema, ao longo de um ano, associando a espessura foveal central com a hemoglobina glicosilada (HbA1c) e alterações na acuidade visual. 3) Correlacionar os resultados obtidos com o grupo controle. MÉTODOS: Estudo prospectivo de uma amostra de 30 pacientes, com edema macular diabético e acuidade visual melhor ou igual a 20/40. O estudo contou com 30 olhos como grupo controle. Foram feitas medidas da melhor acuidade visual corrigida, dosagem de hemoglobina glicosilada, biomicroscopia com lente de 78 dioptrias, angiofluoresceinografia e tomografia de coerência óptica. Determinou-se, pelo propósito do estudo, a espessura foveal central como principal variável. Além da estatística descritiva, utilizaram-se testes para análise dos resultados: foi testada a homogeneidade de cada variável pelos testes t-Student, Qui-Quadrado e teste de Tukey; para correlacionar variáveis utilizou-se a análise de variância (ANOVA). A relação entre a espessura foveal central no tomografia de coerência óptica com a acuidade visual e a hemoglobina glicosilada foi estudada através de regressão linear. RESULTADOS: Registrou-se não haver diferença significativa entre casos e controles nas variáveis idade (p=0,343) e sexo (p=0,793). Os valores da espessura foveal central para o sexo masculino foram maiores que no sexo feminino (p<0,05) mostrando que a variável sexo interfere nos valores da espessura foveal central. Dos pacientes diabéticos com edema macular clinicamente significativo, 83,33% apresentavam retinopatia diabética não-proliferativa moderada, 10% retinopatia diabética não-proliferativa leve e 6,66% retinopatia diabética não-proliferativa grave. Os pacientes em tratamento combinado de insulina com hipoglicemiante oral apresentaram influência nos resultados da espessura foveal central pela tomografia de coerência óptica e na acuidade visual. A duração média do diabetes foi de 9,63 anos. Registraram-se valores da espessura foveal central pela tomografia de coerência óptica sempre maiores nos pacientes que no grupo controle (p<0,001). As medidas da HbA1c não influenciaram os valores da espessura foveal central (p=0,130) e as medidas da acuidade visual se correlacionaram significativamente com espessura foveal central (p=0,02). CONCLUSÃO: Os resultados deste estudo mostraram a aplicabilidade da tomografia de coerência óptica na detecção do edema macular diabético em pacientes com acuidade visual melhor ou igual a 20/40, ao longo de um ano, mostrando o espessamento retiniano nos estágios iniciais de retinopatia diabética. Evidenciou-se a correlação entre o aumento da espessura foveal central e a piora da acuidade visual. As medidas da HbA1c não influenciaram nas medidas da espessura foveal central. A detecção precoce do edema macular clinicamente significativo leva-nos a redimensionar o real significado da retinopatia incipiente, podendo prevenir perdas acentuadas da visão.
Descritores: Retinopatia diabética; Edema macular; Tomografia de coerência óptica; Fotocoagulação; Fóvea central; Acuidade visual
ORIGINAL ARTICLE
Retinal thickness measurement and evaluation of natural history of the diabetic macular edema through optical coherence tomography
Medida da espessura retiniana e avaliação da história natural do edema macular diabético pela tomografia de coerência óptica
Rosana Zacarias HannoucheI; Marcos Pereira de ÁvilaII
IPós-graduanda da Universidade Federal de Goiás (UFG) - Goiânia (GO) - Brasil
IIProfessor Doutor e Chefe do Centro de Referência em Oftalmologia (CEROF) da UFG - Goiânia (GO) - Brasil
ABSTRACT
PURPOSE: 1) Diagnose, through optical coherence tomography (OCT) exam, the occurrence of diabetic macular edema in patients with diabetic retinopathy and visual acuity of 20/40 or better, by measuring the foveal center point thickness, during one year. 2) Evaluate the edema natural history, during this period, associating the center point thickness with hemoglobin A1c and changes in visual acuity. 3) Correlate the obtained results with the control group.
METHODS: A prospective study was done, of a sample of 30 patients with diabetic macular edema and visual acuity of 20/40 or better. Measurements of the best corrected visual acuity, hemoglobin A1c level, biomicroscopy with 78-diopter lens, fluorescein angiogram and optical coherence tomography were made. The retinal thickness was selected as the main variable. Besides descriptive statistics, additional tests were applied to analyze the results and determine the correlation between these variables, such as t-Student, Chi-Square, Tukey and ANOVA. The relation of optical coherence tomography with visual acuity and hemoglobin A1c was studied through linear regression.
RESULTS: It was found that there is no significant difference between patients and normal individuals, for the variables age and gender. The values of center point thickness found for men were greater than those for women, showing the influence of gender on that thickness. As many as 83.33% of the diabetic patients with clinically significant macular edema presented moderate non-proliferative diabetic retinopathy (NPDR), 10% presented mild NPDR and 6.66% severe non-proliferative diabetic retinopathy. Patients under combined treatment of insulin and oral hypoglycemiant presented influence on the results of center point thickness (through OCT) and visual acuity. The mean duration of diabetes was 9.63 years. Values of center point thickness were always found greater for patients than those for normal eyes. Levels of hemoglobin A1c did not have influence on the center point thickness data, whereas values of visual acuity were significantly correlated with it.
CONCLUSION: This study presents the optical coherence tomography applicability in the detection and semiologic evaluation of diabetic macular edema in patients with visual acuity 20/40 or greater, during one year, showing the retinal thickening in the early stages of diabetic retinopathy. Further, it evidenciated the correlation between the increase in foveal thickness and the reduction in visual acuity. Levels of hemoglobin A1c did not influence the center point thickness data. An early detection of clinically significant macular edema leads us to a redefinition of the real meaning of incipient retinopathy and can prevent further significant reduction of vision.
Keywords: Diabetic retinopathy; Macular edema; Tomography, optical coherence; Light coagulation/methods; Fovea centralis; Visual acuity
RESUMO
OBJETIVOS: 1) Diagnosticar a presença de edema macular diabético em pacientes com retinopatia diabética e acuidade visual igual ou melhor que 20/40, pela realização do exame de tomografia de coerência óptica, medindo a espessura foveal central, ao longo de um ano. 2) Avaliar a história natural do edema, ao longo de um ano, associando a espessura foveal central com a hemoglobina glicosilada (HbA1c) e alterações na acuidade visual. 3) Correlacionar os resultados obtidos com o grupo controle.
MÉTODOS: Estudo prospectivo de uma amostra de 30 pacientes, com edema macular diabético e acuidade visual melhor ou igual a 20/40. O estudo contou com 30 olhos como grupo controle. Foram feitas medidas da melhor acuidade visual corrigida, dosagem de hemoglobina glicosilada, biomicroscopia com lente de 78 dioptrias, angiofluoresceinografia e tomografia de coerência óptica. Determinou-se, pelo propósito do estudo, a espessura foveal central como principal variável. Além da estatística descritiva, utilizaram-se testes para análise dos resultados: foi testada a homogeneidade de cada variável pelos testes t-Student, Qui-Quadrado e teste de Tukey; para correlacionar variáveis utilizou-se a análise de variância (ANOVA). A relação entre a espessura foveal central no tomografia de coerência óptica com a acuidade visual e a hemoglobina glicosilada foi estudada através de regressão linear.
RESULTADOS: Registrou-se não haver diferença significativa entre casos e controles nas variáveis idade (p=0,343) e sexo (p=0,793). Os valores da espessura foveal central para o sexo masculino foram maiores que no sexo feminino (p<0,05) mostrando que a variável sexo interfere nos valores da espessura foveal central. Dos pacientes diabéticos com edema macular clinicamente significativo, 83,33% apresentavam retinopatia diabética não-proliferativa moderada, 10% retinopatia diabética não-proliferativa leve e 6,66% retinopatia diabética não-proliferativa grave. Os pacientes em tratamento combinado de insulina com hipoglicemiante oral apresentaram influência nos resultados da espessura foveal central pela tomografia de coerência óptica e na acuidade visual. A duração média do diabetes foi de 9,63 anos. Registraram-se valores da espessura foveal central pela tomografia de coerência óptica sempre maiores nos pacientes que no grupo controle (p<0,001). As medidas da HbA1c não influenciaram os valores da espessura foveal central (p=0,130) e as medidas da acuidade visual se correlacionaram significativamente com espessura foveal central (p=0,02).
CONCLUSÃO: Os resultados deste estudo mostraram a aplicabilidade da tomografia de coerência óptica na detecção do edema macular diabético em pacientes com acuidade visual melhor ou igual a 20/40, ao longo de um ano, mostrando o espessamento retiniano nos estágios iniciais de retinopatia diabética. Evidenciou-se a correlação entre o aumento da espessura foveal central e a piora da acuidade visual. As medidas da HbA1c não influenciaram nas medidas da espessura foveal central. A detecção precoce do edema macular clinicamente significativo leva-nos a redimensionar o real significado da retinopatia incipiente, podendo prevenir perdas acentuadas da visão.
Descritores: Retinopatia diabética; Edema macular; Tomografia de coerência óptica; Fotocoagulação/métodos; Fóvea central; Acuidade visual
INTRODUCTION
The diabetes has been an important aspect of visual limitation and blindness worldwide, and the diabetic macular edema stands out as one of the main causes of visual impairment and low vision(1). Its observation and importance have always been related to metabolic descompensation of diabetes mellitus. It is known that hyperglicemy is a major agent of all microvascular complications of diabetes. The various clinical methods used to evaluate macular thickening, such as slit-lamp biomicroscopy and stereoscopic photography, are relatively insensitive to small changes in retinal thickness and are not enough to evaluate structural abnormalties in the retina.
The development of digital image analysis, with laser scan of high resolution, culminated with a better image quality and disclosure of optical coherence tomography (OCT) as a diagnosis technique, capable of generate bidimentional images with high level of reproducibility and resolution, through cross-sectional imaging of the retina. The OCT is currently used to confirm diagnostic hypothesis, monitor qualitatively and quantitatively the pharmacologic treatment of diabetic macular edema and, therefore, follow the progression of the disease in a more criterial way.
This study used OCT to verify the presence of macular thickening in diabetic patients who presented visual acuity 20/40 or greater, and evaluated the course of the natural history of these patients during one year, comparing the findings of central foveal thickness (CFT) with visual acuity and hemoglobin A1c.
METHODS
This study was approved by the Research Ethic Committee (Investigational Review Board) of the Clinical Hospital of the Medicine School-Federal University of Goiás. The sample was established with individuals who voluntarily agreed to participate in this study, signing a written informed consent document before procedures were carried out, according to the Health National Council. A prospective study was done, of a sample of patients who looked for the Ophthalmology service at the eye care center CEROF-UFG, from June 2007 to July 2008, after semiologic evaluation.
All patients were examined by the same researcher and filled a form, informing age, gender, history of the current disease, use of insulin and/or oral hypoglycemiant, and levels of hemoglobin A1c.
The exam was divided in three phases: during the baseline as the first phase, a complete ophthalmologic exam was done, as well as the measurement of best corrected visual acuity and detection of clinically significant macular edema (CSME) through biomicroscopy with a 78-diopter lens. Fluorescein angiogram and OCT corresponded, respectively, to second and third phases.
The sample had 30 patients with type 2 diabetes for more than 5 years, diabetic retinopathy with or without clinical control, age from 30 to 65 years, visual acuity of 20/40 or greater, refractometry between -3.00 and +3.00 dioptries, with diabetic macular edema. If the patients, in any exam, presented signs of clinical worsening with impairment in visual acuity (worse than 20/100), and/or macular thickening greater than 350 µm in either eye, and/or fluorescein angiogram with significant leakage increase in relation to previous exam, they were guided to treatment.
After gathering the OCT data, CFT results of only one eye per patient were used in the analysis of the results.
During this study, systemic arterial hypertension was monitored, and iatrogeny was analyzed.
Exclusion criteria included: macular diseases other than the diabetic maculopathy; patients previously submitted to macular photocoagulation or ocular surgery, including cataract extraction, trabeculectomy and vitrectomy; aphakia or pseudophakia patients; other retinal vasculopathies; media opacity, such as corneal opacities, vitreous hemorrhage and cataract; age related macular degeneration (AMD); low vision; patients with proliferative diabetic retinopathy at any stage; and improper fixation.
The collected data were organized according to: gender, age, visual acuity, duration of diabetes, use of insulin, other hypoglycemiant medication and level of hemoglobin A1c.
According to the criteria from Early Treatment Diabetic Retinopathy Study, non-proliferative diabetic retinopathy was classified in mild, moderate and severe(2).
The control group was formed with 30 individuals, without diabetes mellitus, from 30 to 65 years of age, best-corrected visual acuity 20/40 or better, and refractometry between -3.00 and +3.00 dioptries.
The results obtained from normal individuals were used to correlate data of patients with diabetic retinopathy, in order to evaluate the exam reproducibility.
A CFT of 200 µm was considered as normal, as in most referenced studies(2-3).
All variables in this study presented statistic normal distribution, from Kolmogorov-Smirnov test (Table 1). Additional tests were applied to analyze the results, such as t-Student, Chi-Square and Tukey. A variance analysis was used with ANOVA test, to determine the correlation between these variables.
RESULTS
Four hundred patients had both eyes examined. Among those patients, 80 presented CSME and 50 patients were excluded from this study.
The macular thickness found in diabetic patients was always greater than that for the control group. The OCT showed the existence of a correlation between macular thickness and retinopathy level (Figure 1).
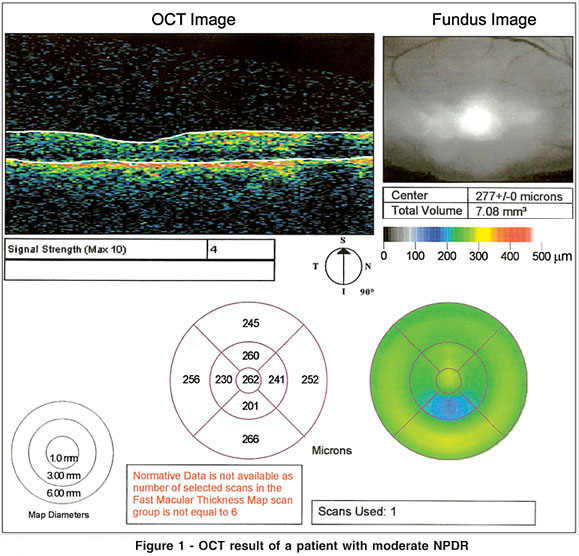
The patients with diabetic retinopathy and retinal thickening presented different degrees of edema, and, as a result, variations of retinal thickness. Ten percent of the cases were mild NPDR, 83.33% were moderate, and 6.66% were severe.
The mean age of diabetic patients was 52 years, and 49.8 years for the normal individuals. From t-Student test, it was shown that there was no significant difference between patients and the control group (p=0.343) for the age variable.
The mean duration of diabetes was 9.63 years, with standard deviation of 3.51.
The statistic analysis of data showed, according to gender, a significant result in the values of central foveal thickness measured by OCT. These values were greater for men than for women. Therefore, gender was a variable that changed OCT values in this research (t-Student: p<0.05). There was no significant difference between the patients and normal individuals, for this variable, according to Chi-Square test (p=793).
A linear regression analysis did not show any significant influence of CFT measured by OCT and hemoglobin A1c over each other (p=0.130), as illustrated in figure 2.
In contrast, a good inverse proportionality (p=0.020) was noted between visual acuity and retinal thickness, as shown in figure 3. Therefore, OCT values had influence, at the follow-up time, on the visual acuity of patients.
In the presence of macular thickening, the risk of progression of the edema during one year was, in this study, equal to 46.6%.
Forty percent of the patients had the diabetic retinopathy worsened, demonstrated through OCT. The profile of these patients was men, users of insulin or combined treatment of insulin and oral hypoglycemiant. A total of 46.66% of the patients had their visual acuity worsened.
DISCUSSION
The hemoglobin A1c is a type of hemoglobin present naturally in blood cells, useful in the determination of high levels of glycemia during long periods. This type of hemoglobin is formed from non-enzymatic reactions between hemoglobin and glucose, through an irreversible connection, to form a stable complex of glycosylated hemoglobin.
Among the ocular complications caused by diabetes, the retinopathy is responsible for the existence of 1.78 million of blind individuals in the world(4).
The metabolic control of this disease is an important factor of beginning, progression and severity of diabetic retinopathy. Patients treated intensively present less risk of microvascular complications, maintaining glycemia and glycosylated hemoglobin levels as close as possible to normality. It can be affirmed that there is a relation between an improper metabolic control and the development of retinopathy, which potentially reduces the vision(5).
Diabetic macular edema is a condition characterized by anatomic thickening of the retina, due to the presence of abnormal fluid accumulation within the retina. It is a result of blood-retinal barrier breakdown.
The OCT measures the retinal thickness by considering the distance between the anterior surface of the retinal pigmented epithelium RPE-choriocappillaris region and the vitreoretinal interface.
Even with new measurement techniques, there is diversity in OCT values cited in literature(3-6), which may be explained by the intervention of ametropy, gender and age.
In some research works, the mean retinal thickness does not vary significantly, if related to age. However, there is a variation of 0.30 µm per decade of life(7), which may be attributed to senile photoreceptor loss, with modification of ganglion cells in the parafoveal region and in the fiber layer near the optic disc, replaced by fibroglial elements.
More recent studies suggested that, in order to compare retinal thickness, it is necessary to consider gender, since their results showed thickness values significantly greater in men(8-9). Kelty (2008) suggested thinner retinas in older patients, women, African-Americans and individuals with myopia of -5.00 dioptries or more.
Despite the fact that visual acuity works as a modest indicator of retinal thickness, it does not surrogate quantitative values, given that other variables, such as age, time of retinal ischemy, leakage presented in the angiogram and glycosylated hemoglobin, also interfere in the visual acuity(2-10). Hence, visual acuity can be taken into account as an important variable in the mild and moderate stages of non proliferative diabetic retinopathy (NPDR), but may be considered as a poor indicator in advanced stages of diabetic maculopathy.
The evaluation of macular thickening by OCT is certainly useful in practical clinic, but the retinal thickness is just one of the variables affecting visual acuity, in a complex of causes, still, not completely known(10).
The OCT is a diagnostic technique that provides cross-sectional imaging of retinal structure and of other ocular tissues, with high accuracy and resolution. Thus, its capacity to reproduce details (10 µm) gets close to the optical microscopy, being compared to a biopsy in vivo. The OCT increases the ability of clinical diagnosis and imaging techniques in ancillary exams, for giving precise and reproducible results that corroborate diagnostic impressions and allow monitoring the progression of diseases, as well as the evolution of retinal responses in therapeutic interventions.
Several research works have showed that OCT is more sensible to detect macular edema than biomicroscopy with 78-diopter lens, which evaluation is subjective(11-12). OCT demonstrates that the macular edema is a complex clinical entity with various morphologies, and goes beyond the limitations of a simple clinical definition. In the early stages of edema, OCT is of main importance, because structural changes in the retina are still not evident with biomicroscopy or fluorescein angiogram(13-14). In the presence of CSME, there is a significant agreement between patterns of fluorescein angiogram and OCT(15).
From a clinical perspective, it can be said that diagnosing macular edema clinically, when it does not appear in OCT, probably would lead to an unnecessary intervention with focal photocoagulation, which leads to paracentral scotomas. OCT can reduce the risk of scotomas induced by laser, in eyes to which clinical suspicion of edema exists, but objective verification does not(11-14). Therefore, the reduction of macular edema can be documented objectively, which makes the OCT, as said in various studies, the right technique to be chosen to follow macular edema.
OCT presents limitations when considering its applicability. Opacities, such as corneal edemas and opacities, cataract with significant opacity, vitreous hemorrhage, among other changes of dioptric media, attenuate the incidence and reflection of light required to final imaging(12).
Another limitation is related to the patient who is not capable of fixing, either because he is not very collaborative, or because of central vision impairment, producing, in these cases, results below the expected. However, the protocol presents the algorithm of alignment, which reduces the inaccuracy caused by the eye movements.
Some retinal diseases, that cause expressive impairment in central visual acuity and lead to an eccentric fixation, can impair the positioning of the scan and data analysis(16). Acquiring images in eyes with justafoveal lesion demands special care, because macular atrophies modify the central retinal anatomy and make it difficult to position the scan at the region to be analyzed.
When pupillary dilation is poor, the exam can still be done. The optical alignment becomes more sensible, due to pupil reduction, and the vision field of the examiner is reduced.
The current treatment of diabetic retinopathy has the objective of preventing, or delaying, the retinopathy appearance, progression, and the impairment of vision(17). The classic treatment is photocoagulation, and the early diagnosis is associated with a better therapeutic response, to prevent expressive vision impairment(18). This emphasizes the requirement of diagnosis when good vision is still present(13-17).
CONCLUSION
This study highlighted the advantages of the use of OCT in the detection of clinically significant macular edema.
It was found, in the literature, support for the association of macular edema with retinal thickening and visual acuity. A standardized comparison between data from patients and normal individuals avoided distortions that could have had influence on the final results.
This study demonstrated the use of OCT in the measurement of retinal thickness and its potential as an indicator in the early diagnosis of diabetic retinopathy, offering new perspectives for the follow-up and treatment of diabetic macular edema.
REFERENCES
1. Olk J, Carol M, Lee JB. Diabetic retinopathy: practical management. Philadelphia: Lippincott; 1993.
2. Browning DJ, Fraser CM, Clark S. The relationship of macular thickness to clinically graded diabetic retinopathy severity in eyes without clinically detected diabetic macular edema. Ophthalmology. 2008;115(3):533-39,e2.
3. Chan A, Duker JS, Ko TH, Fujimoto JG, Schuman JS. Normal macular thickness measurements in healthy eyes using Stratus optical coherence tomography. Arch Ophthalmol. 2006;124(2):193-8.
4. World Health Organization. Prevention of blindness from diabetes mellitus [Internet]. Genebra: WHO; 2005. [cited 2009 Jan 4]. Available from: http://www.who.int/blindness/Prevention%20of%20Blindness%20from%20 Diabetes%20Mellitus-with-cover-small.pdf
5. Klein R, Klein BE, Moss SE, Cruickshanks KJ. The Wisconsin Epidemiologic Study of diabetic retinopathy. XIV. Ten year incidence and progression of diabetic retinopathy. Arch Ophthalmol. 1994;112(9):1217-28. Comment in: Arch Ophthalmol. 1995;113(6):702-3.
6. Estevão ML, Rosen RB, Gentile RC, Muldoon TO. Variables associated with retinal thickness. Invest Ophthalmol Vis Sci. 1999;40(4):S125-6.
7. Baquero Aranda IM, Morillo Sánchez MJ, Garcia Campos JM. [Use of optical coherence tomography to study variations of normal parameters with age]. Arch Soc Esp Oftalmol. 2005;80(4):225-31. Spanish.
8. Bressler NM, Edwards AR, Antoszyk AN, Beck RW, Browning DJ, Ciardella AP, Danis RP, Elman MJ, Friedman SM, Glassman AR, Gross JG, Li HK, Murtha TJ, Stone TW, Sun JK; Diabetic Retinopathy Clinical Research Network. Retinal thickness on Stratus optical coherence tomography in people with diabetes and minimal or no diabetic retinopathy. Am J Ophthalmol. 2008; 145(5):894-901.
9. Kelty PJ, Payne JF, Trivedi RH, Kelty J, Bowie EM, Burger BM. Macular thickness assessment in healthy eyes based on ethnicity using Stratus OCT optical coherence tomography. Invest Ophthalmol Vis Sci. 2008;49(6):2668-72.
10. Diabetic Retinopathy Clinical Research Network, Browning DJ, Glassman AR, Aiello LP, Beck RW, Brown DM, Fong DS, Bressler NM, Danis RP, Kinyoun JL, Nguyen QD, Bhavsar AR, Gottlieb J, Pieramici DJ, Rauser ME, Apte RS, Lim JI, Miskala PH. Relationship between optical coherence tomograghy- measured central retinal thickeness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114(3):525-36. Comment in: Curr Diab Rep. 2008; 8(4):255-6; Ophthalmology. 2008;115(2):416-7; author reply 417.
11. Browning DJ, McOwen MD, Bowen RM Jr, O'Marah TL. Comparison of the clinical diagnosis of diabetic macular edema with diagnosis by optical coherence tomography. Ophthalmology. 2004;111(4):712-5. Comment in: Ophthalmology. 2005;112(4):734-5; author reply 735.
12. Massin P, Erginay A, Haouchine B, Mehidi AB, Paques M, Gaudric A. Retinal thickness in healthy and diabetic subjects measured using optical coherence tomography mapping software. Eur J Ophthalmol. 2002;12(2):102-8.
13. Ozdek SC, Erdinc MA, Gurelik G, Aydin B, Bahceci U, Hasanreisoglu B. Optical coherence tomography assessment of diabetic macular edema: comparison with fluorescein angiographic and clinical findings. Ophthalmologica. 2005; 219(2):86-92.
14. Sugimoto M, Sasoh M, Ido M, Wakitani Y, Takahashi C, Uji Y. Detection of early diabetic change with optical coherence tomography in type 2 diabetes mellitus patients with without retinopathy. Ophthalmologica. 2005;219(6):379-85.
15. Kang SW, Park CY, Ham DI. The correlation between fluorescein angiographic and optical coherence tomographic features in clinically significant diabetic macular edema. Am J Ophthalmol. 2004;137(2):313-22.
16. Sadda SR, Wu Z, Walsh AC, Richine L, Dougall J, Cortez R, et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology. 2006;113(2):285-93.
17. Farah ME. Tomografia de coerência óptica: OCT. Rio de Janeiro: Cultura Médica; 2006.
18. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report nº 4. The Early Treatment Diabetic Retinopathy Study Research Group. Int Ophthalmol Clin. 1987;27(4):265-72.
 Endereço para correspondência:
Endereço para correspondência:
Rosana Hannouche
Av. T-8, 171 - Setor Marista
Goiânia (GO) CEP 74210-270
E-mail: [email protected]
Recebido para publicação em 18.01.2009
Última versão recebida em 09.05.2009
Aprovação em 25.05.2009
Trabalho realizado no Departamento de Oftalmologia da Universidade Federal de Goiás (UFG) - Goiânia (GO) - Brasil.
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência dos Drs. João Borges Fortes Filho e Pedro Carricondo sobre a divulgação de seus nomes como revisores, agradecemos suas participações neste processo.