

Dilay Ozek; Ozlem Evren Kemer
DOI: 10.5935/0004-2749.20180100
ABSTRACT
Purpose: This study aimed to compare the effectiveness of eye drops containing a combination of sodium hyaluronate and trehalose and sodium hyaluronate for the treatment of corneal cross-linking and epithelial healing.
Methods: This study included 46 eyes of 23 keratoconus patients who underwent corneal cross-linking on both eyes. Unpreserved trehalose 30 mg/mL and sodium hyaluronate 1.5 mg/mL (Thealoz Duo®; Thea, France) were applied six times a day on one eye of each patient and unpreserved sodium hyaluronate 0.15% (Eye Still®; Teka, Inc., Istanbul) was applied on the other eye. Patients were examined daily until complete re-epithelialization. Postoperative examinations to assess the measured size of epithelial defect were performed using slit-lamp biomicroscopy.
Results: The study included 23 patients (13 females and 10 males) with a mean age of 20.9 ± 10.3 years. Corneal epithelial healing time after cross-linking was 2.3 ± 1.2 days for the trehalose and sodium hyaluronate group and 3.8 ± 2.9 days for the sodium hyaluronate group (p=0.03).
Conclusion: The application of eye drops containing the combination of trehalose and sodium hyaluronate resulted in faster corneal re-epithelialization following corneal cross-linking than that of eye drops containing sodium hyaluronate alone.
Keywords: Keratoconus; Epithelium, corneal; Wound healing; Trehalose; Hyaluronic acid; Ophthalmic solutions; Cross-linking reagents
RESUMO
Objetivo: Este estudo teve como objetivo comparar a eficácia de colírios contendo uma combinação de hialurônico de sódio e hialuronato de sódio e trealose para o tratamento da cicatrização epitelial em pacientes com cross-linking corneano.
Métodos: Este estudo inclui 46 olhos de 23 pacientes com ceratocone, que foram operados com cross-linking corneano em ambos os olhos. Trealose não preservada 30 mg/mL e hialuronato de sódio 1,5 mg/mL (Thealoz Duo®; Thea, França) foram aplicados seis vezes por dia em um olho de cada paciente e hialuronato de sódio não conservado, 0,15% (Eye Still®; Teka, Inc., Istambul) foi aplicada no outro olho. Os pacientes foram examinados diariamente até a completa reepitelização. Exames pós-operatórios para avaliar o tamanho medido do defeito epitelial foram realizados usando biomicroscopia com lâmpada de fenda.
Resultados: O estudo incluiu 23 pacientes (13 mulheres e 10 homens) com idade média de 20,9 ± 10,3. O tempo de cicatrização epitelial da córnea após o cross-linking foi de 2,3 ± 1,2 dias para o grupo trealose e hialuronato de sódio e 3,8 ± 2,9 dias para o grupo hialurônico de sódio (p=0,03).
Conclusão: A aplicação de gotas para os olhos contendo combinação de trealose e hialuronato de sódio resultou em uma re-epitelização da córnea mais rápida após o cross-linking corneano do que a de gotas contendo hialurônico de sódio apenas.
Descritores: Ceratocone; Epitélio anterior; Cicatrização; Trealose; Ácido hialurônico; Soluções oftálmicas; Reagentes para ligações cruzadas
INTRODUCTION
Keratoconus is the most common primary ectasia and is characterized by corneal steepening, visual distortion, apical corneal thinning, and central corneal scarring. Corneal cross-linking (CXL) has become a conventional treatment method for progressive keratoconus over the past decade. CXL is primarily performed to halt the progression of corneal ectasia. Riboflavin combined with ultraviolet A irradiation (UVA) allows for the strengthening of corneal tissue. Riboflavin acts as a photosensitizer in the photopolymerization process, and when combined with UVA irradiation, it increases the formation of intrafibrillar and interfibrillar carbonyl-based collagen covalent bonds via a molecular process that remains unclear(1).
Riboflavin and UVA can be applied after scraping off the corneal epithelium or alternatively, in CXL. Riboflavin cannot permeate the corneal epithelium because of its hydrophilic macromolecule properties, which is why the corneal epithelium is removed. The use of therapeutic contact lenses and artificial tears can speed up the corneal epithelium healing process. A new type of eye drop comprising a combination of trehalose and sodium hyaluronate has been recently introduced. Trehalose has a unique promoting cell survival under desiccation by stabilizing lipids and cell membrane proteins and reducing the number of dead cells on the ocular surface(2).
In our study, patients had CXL in both eyes during two separate sessions and were treated with sodium hyaluronate (SH) alone in 1 eye and with a combination of trehalose and SH (TH-SH) in the other eye and re-epithelialization periods were compared between these groups.
METHODS
This study was approved by the local Ethics Committee of the Ankara Numune Research and Training Hospital and adhered to the principles of the Declaration of Helsinki.
Both eyes of 23 patients underwent epithelium-off (epi-off) CXL in two separate sessions, which had progression of >1 diopter (D), Kmax increase, >2% thinning on the thinnest point of the cornea, and a >0.5 D increase on the manifest refraction spherical value on Scheimpflug camera (Pentacam) evaluation. The first operated eye of each patient was treated with SH alone for epithelial healing, and the second eye was operated an average of 2 weeks after complete re-epithelialization of the first eye was obtained and treated with TH-SH.
Surgical procedure and postoperative treatment
Prior to CXL operation, proparacaine hydrochloride 0.5% (Alcaine; Alcon Laboratories, Puurs, Belgium) was applied. The operation started with central 8.0 mm corneal epithelium debridement using a crescent knife (Beaver-Visitec International Inc., Waltham, MA, USA) with the application of 20% alcohol for 30 s with trephine. Afterward, 5% NaCL solution was used for a thorough cleaning. Riboflavin treatment (0.1% riboflavin-5´-phosphate and 20% dextran T-500) was immediately started after epithelium removal and continued for 30 min at 2-min intervals. In addition, riboflavin was continued to be applied at 2-min intervals during the course of a 10-min exposure to 9 mW/cm2 UVA.
Finally, a therapeutic contact lens (Air Optics; Alcon, Inc.) was fitted. During the treatment period, both eyes underwent standard treatment with diclofenac (Acular LS®) and netilmicin (Netira®), both four times daily. One eye of each patient was treated with sodium hyaluronate (Eye Still®) and the other eye with TH-SH (Thealoz Duo®), both six times daily. Both eyes of the same patient undergoing different treatments were followed up every day until complete re-epithelialization was observed.
Analysis of epithelial defects
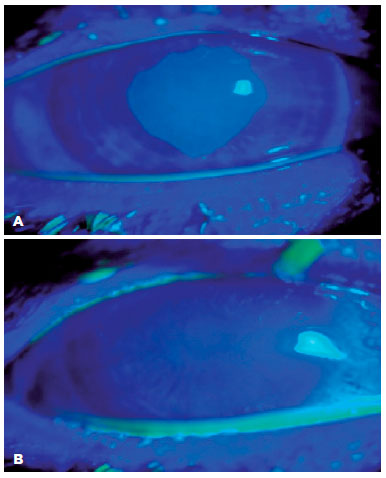
The size of the corneal defect was measured using a cobalt blue filter following the instillation of 2 µL 1% fluorescein solution. Recorded images were analyzed using ImageJ software (NIH, Bethesda, MD, USA) using the binary process. The size of the epithelial defect was calculated and expressed as that relative to the central 8.0 mm cornea. Epithelial status was also examined using slit-lamp biomicroscopy on postoperative days 1, 2, 3, 4, 5, and 7 until total epithelial healing was achieved. The level of re-epithelialization was measured daily by removing the contact lens. If epithelialization was not completed, then the contact lens was reattached and then removed when re-epithelialization was complete.
The present study did not include CXL patients aged <18 years, those with previous eye surgery, or those with potential epithelial healing problems including severe dry eye or diabetes mellitus.
Data were analyzed using IBM SPSS 20.0 Statistics for Macintosh (SPSS, Inc, Chicago, IL, USA). Independent samples t test was performed to compare astigmatism, central corneal thickness, and best-corrected visual acuity, and a paired sample t test was performed to compare total epithelialization time and size. p<0.05 was considered statistically significant.
RESULTS
Overall, 46 eyes of 23 patients (13 females, 10 males) underwent epi-off CXL. Mean age of patients was 25.3 years (19-35). Clinical presentation of the patients is shown in table 1.
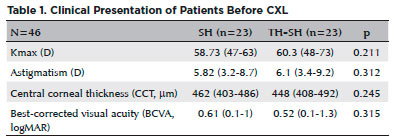
No significant difference was found between the two groups for Kmax, astigmatism, central corneal thickness (CCT), and best-corrected visual acuity (BCVA) prior to Coppock-like cataract operation (p≥0.05).
Corneal epithelial healing after CXL was observed after 2.3 ± 1.2 days (range, 1.0-5.0 days) in the TH-SH and 3.8 ± 2.9 days (range, 1-7 days) in the SH group, and the difference was statistically significant (p=0.03). TH-SH patient’s corneal epithelium defect with fluorescein on the first and (A) second postoperative days (B) are shown in figure 1.
Epithelial defects in the central 8.0 mm debridement area of the corneal epithelium were noted in both eyes of 23 patients in the SH and TH-SH groups, respectively, The TH-SH group had epithelial defects with a mean percentage area relative to the whole debrided area of 26.2% ± 31.1% (range, 16%-92%) on day 1, 16.2% ± 21.1% (range, 10%-40%) on day 3, and 8.3% ± 11.1% (range, 0%-10%) on day 5. The SH group had epithelial defects with a mean percentage area of 32.5% ± 25.7% (range, 0.19%-72%) on day 1, 22.8% ± 13.7% (range, 0.15%-58%) on day 3, and 11.5% ± 13.7% (range, 0%-18%) on day 5 with a statistically significant difference between the two groups on day 1 (p=0.021) and day 3 (p=0.047).
All patients tolerated the use of contact lenses, and no recurrent epithelial problems were noted following contact lens removal. No complications, such as infection, contact lens damage, or corneal infiltration, were noted.
DISCUSSION
CXL is a convenient technique developed on the underlying pathology of the keratoconus. CXL is a relatively new approach where new covalent bands reform with the application of riboflavin and UVA. CXL complication rates ranged from 1% to 10% depending on the stage of keratoconus, with early postoperative complications including transient stromal haze, sterile infiltrates, endothelial decompensation, delayed epithelial healing, and infectious keratitis. Moreover, stromal opacity can be a delayed postoperative event(3).
Diluted ethanol was used to reduce structural and ultrastructural changes due to the toxic effect of alcohol on the corneal epithelial cell. Trehalose showed better morphological and morphometric features of alcohol-treated corneal epithelium and epithelial thickness than the control group in LASEK(4). In the present study, diluted ethanol was used in epi-off CXL. Re-epithelialization of the TH-SH group may have been faster than that of the SH group because trehalose stays on the corneal surface for a prolonged time without preservatives.
Epithelium healing following CXL is a critical step. During this time, fast healing reduces the risks of infection and pain-related discomfort. Confocal microscopy analysis showed that epithelial healing was complete at 1 week after cross-linking. The subepithelial plexus demonstrated nerve plexus loss at 1 month and nerve fiber regeneration, which was started at 3 months and completed at 6 months(5). Total re-epithelialization following CXL was observed 2.7 ± 0.7 days after the epi-on and 2.3 ± 0.4 days after the epi-off procedures(6). In the present study, corneal epithelial healing was observed following epi-off CXL at 2.3 days (range, 1-5 days) for the TH-SH group and at 3.8 days (range, 1-7 days) for the SH group. Using the epi-off technique, our patients showed improved treatment of re-epithelialization for a longer time. This difference may be related to the more objective measurement of re-epithelialization using ImageJ software.
Common treatment methods to shorten the re-epithelialization period include contact lens fitting and the use of artificial tears. A new bioprotectant agent-trehalose-combined with SH may accelerate epithelization. SH is a component of natural tears and a polysaccharide comprising repeating disaccharide. SH protects corneal epithelial cells, stimulates epithelial migration and adhesion, and has a long-term thickening effect on tear film layer. SH has very good biocompatibility and viscoelastic characteristics, remains on the ocular surface for a prolonged time, and increases fluorescein breakup time(7). CD44, the hyaluronate receptor expressed in corneal and conjunctival cells, promotes the interaction of cytoskeletal proteins(8-10). Moreover, hyaluronate binding to CD44 may stimulate cell proliferation via a mechanism involving a kinase cascade(11).Thus, SH exhibits anti-inflammatory activity.
Trehalose is a natural disaccharide that can be synthesized by bacteria, fungi, plants, and invertebrate animals. Trehalose production in the cytoplasm increases during stress and protects the organism with its osmoprotectant and bioprotectant characteristics. Under dry conditions, trehalose stabilizes the cell membrane lipid bilayer by osmoprotection and prevents desiccation-related cell damage. In addition, trehalose plays a role in signal generating or regulating molecules for reducing autophagy, apoptosis, and inflammation-related cell deaths. It hydrates the corneal epithelial cell, prevents desiccation, and improves the epithelial surface by suppressing apoptosis(12). Trehalose not only preserves the cell membrane and membrane proteins from deactivation or denaturation but also has a protective role in reconstructed corneal epithelium(13,14).
Chen et al. have demonstrated that trehalose application restores ocular surface integrity and suppresses inflammatory and proteolytic MMP-9 and Hsp70 expression and keratinization in mice with dry eye damaged by a desiccation model(15).
A study that compared TH-SH with polyethylene glycol/propylene glycol (Systane®) in patients with dry eye observed no significant difference on the ocular surface disease index, ocular staining scores (fluorescein and lissamine green), Schirmer test, and tear breakup time. Patient comfort was significantly better in the TH-SH group according to the visual analog scale(16). Schmidl et al. have indicated that a single application of TH-SH eye drops increases tear film thickness in patients with dry eye disease(17).
SH, with its reported efficacy on symptoms, wound healing properties, anti-inflammatory action, and when combined with the osmoprotectant and bioprotectant activities of trehalose, can be considered more useful for the treatment of epithelial healing following CXL.
Although a new molecule introduced for the treatment of dry eye, trehalose also plays an important role in corneal epithelium healing. Because trehalose is a relatively new agent, we recommend that further studies are warranted for assessing its performance.
REFERENCES
1. Ziaei M, Barsam A, Shamie N, Vroman D, Kim T, Donnenfeld ED, Holland EJ, Kanellopoulos J, Mah FS, Randleman JB, Daya S, Güell J; ASCRS Cornea Clinical Committee. Reshaping procedures for the surgical management of corneal ectasia. J Cataract Refract Surg. 2015;41(4):842-72.
2. Crowe JH, Carpenter JF, Crowe LM. The role of vitrification in anhydrobiosis. Annu Rev Physiol. 1998;60(2):73-103.
3. Seiler TG, Schmidinger G, Fischinger I, Koller T, Seiler T. [Complications of corneal cross-linking]. Ophthalmologe. 2013;110(7): 639-44. German.
4. Aragona P, Colosi P, Rania L, Colosi F, Pisani A, Puzzolo D, et al. Protective effects of trehalose on the corneal epithelial cells. Scientific World Journal. 2014;2014:717835.
5. Sharma N, Suri K, Sehra SV, Titiyal JS, Sinha R, Tandon R, et al. Collagen cross-linking in keratoconus in Asian eyes: visual, refractive and confocal microscopy out comes in a prospective randomized controlled trial. Int Ophthalmol. 2015;35(6):827-32.
6. Yuksel E, Novruzlu S, Ozmen MC, Bilgihan K. A study comparing standard and transepithelial collagen cross-linking riboflavin solutions: epithelial finding and pain scores. J Ocul Pharmacol Ther. 2015;31(5):296-302.
7. Johnson M, Murphy PJ, Boulton M. Effectiveness of sodium hyaluronate eyedrops in the treatment of dry eye. Graefe’s Arch Clin Exp Ophthalmol. 2006;244(3):109-12.
8. Lerner LE, Schawrtz DM, Hwang DG, Howes EL, Stern R. Hyaluronan and CD44 in the human cornea and limbal conjunctiva. Exp Eye Res. 1998;67(3):481-4.
9. Baudouin F, Brignole F, Dupas B. Reduction in keratitis and CD44 expression in dry eye patients treated with a unique 0.18% sodium hyaluronate solution. Invest Ophthalmol Vis Sci. 2001;42(1):32.
10. Entwistle J, Hall CL, Turley EA. HA receptors: signalling to the cytoskeleton. J Cell Biochem 1996;61(1):569-77.
11. Rosales C, O’Brien V, Kornberg L, Juliano R. Signal transduction by cell adhesion receptors Biochem Biophys Acta. 1995;1242(3):77-98.
12. Matsuo T. Trehalose protects corneal epithelial cells from death by drying. Br J Ophthalmol. 2001;85(5):610-2.
13. Elbein AD, Pan YT, Pastuszak I, Carroll D. New insights on trehalose: a multifunctional molecule. Glycobiology. 2003;13(4):17-27.
14. Hill-Bator A, Misiuk-Hojło M, Marycz K, Grzesiak J. Trehalose-based eye drops preserve viability and functionality of cultured human corneal epithelial cells during desiccation. Biomed Res Int. 2014; 2014(3):292139.
15. Chen W, Zhang X, Liu M, Zhang J, Ye Y, Lin Y, et al. Trehalose protects against ocular surface disorders in experimental murine dry eye through suppression of apoptosis. Exp Eye Res. 2009; 89(2):311-8.
16. Pinto-Bonilla JC, Del Olmo-Jimeno A, Llovet-Osuna F, Hernández-Galilea EA randomized crossover study comparing trehalose/hyaluronate eye drops and standard treatment: patient satisfaction in the treatment of dry eye syndrome. Ther Clin Risk Manag. 2015; 13(4):595-603.
17. Schmidl D, Schmetterer L, Witkowska KJ, Unterhuber A, dos Santos VA, Kaya S, et al. Tear film thickness after treatment with artificial tears in patients with moderate dry eye disease. Cornea. 2015; 34(4):421-6.
Submitted for publication:
February 6, 2018.
Accepted for publication:
May 19, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose
Approved by the following research ethics committee: Ankara Numune Education and Research Hospital (#E-17-1177)