INTRODUCTION
Persistent fetal vasculature (PFV) is a congenital anomaly of the eye caused by failure of regression of the primary vitreous during the embryonic period. This rare spectrum of disease, also referred to as persistent hyperplastic primary vitreous, has a wide clinical spectrum, including elongated ciliary processes, shallow anterior chamber, retrolental fibrovascular membrane, cataract, vitreous membrane or stalk originating from the optic nerve, retinal fold, traction or de tachment, and vitreous hemorrhage. The mechanism of angle closure in PFV is not completely known, but includes an enlarged cataractous lens and contraction of the retrolental fibrovascular membrane with secondary anterior lens-iris diaphragm displacement1.
CASE REPORT
A 5-year-old girl was referred with pain and hyperemia in the right eye for 2 days. She had undergone pupil dilation with topical cyclopentolate 1% for a routine eye exam 2 days earlier at another facility, and presented with pain and hyperemia in the right eye, nausea, and vomiting several hours later. Timolol maleate 0.5% and brimonidine tartrate 0.1% ophthalmic solutions had been prescribed b.i.d. for the right eye, with persistence of the symptoms.
Her history included full-term birth at 37 weeks and a neonatal body weight of 2,630 g. At the first visit to our institution, she presented high myopia (OD:-7.00 Sph; OS:-7.50 Sph;-2.00 Cyl @ 90º) and a best-corrected visual acuity of hand motion in OD and 20/50 in OS. Ophthalmic exam showed: corneal edema, a shallow anterior chamber, Van Herick Grade 0, fixed mydriasis, and clear lens in OD (Figure 1), and unremarkable findings in OS. The intraocular pressure (IOP) was 34 mmHg and 14 mmHg in OD and OS, respectively (Goldmann applanation tonometry). Gonioscopy (Zeiss four-mirror lens) was impossible in OD because the patient was in pain and could not cooperate with the exam, but open angle was found in OS.
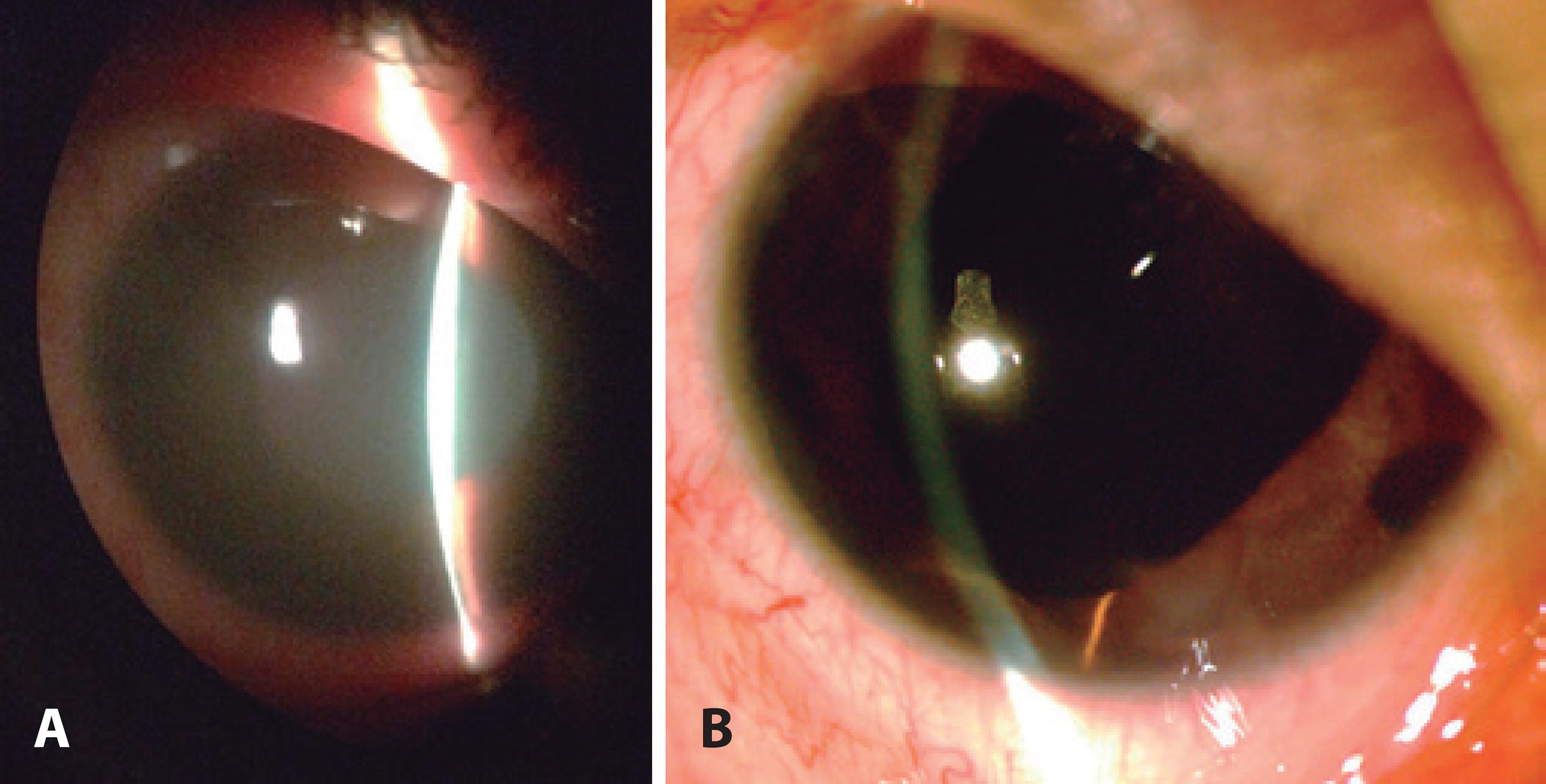
Figure 1 Biomicroscopy of the right eye of a 5-year-old girl with persistent fetal vasculature. A) Before treatment: shallow anterior chamber, corneal edema, fixed mydriasis, and phakia. B) After surgical treatment: wide anterior chamber, iridectomy, and aphakia.
Fundoscopy and wide-field retinography showed a dragged optic disc with the retrolental fibrovascular membrane extending with a narrow base from the optic nerve to the ora serrata in both eyes (Figure 2), which is characteristic of type II or "Y-shape" PFV2.
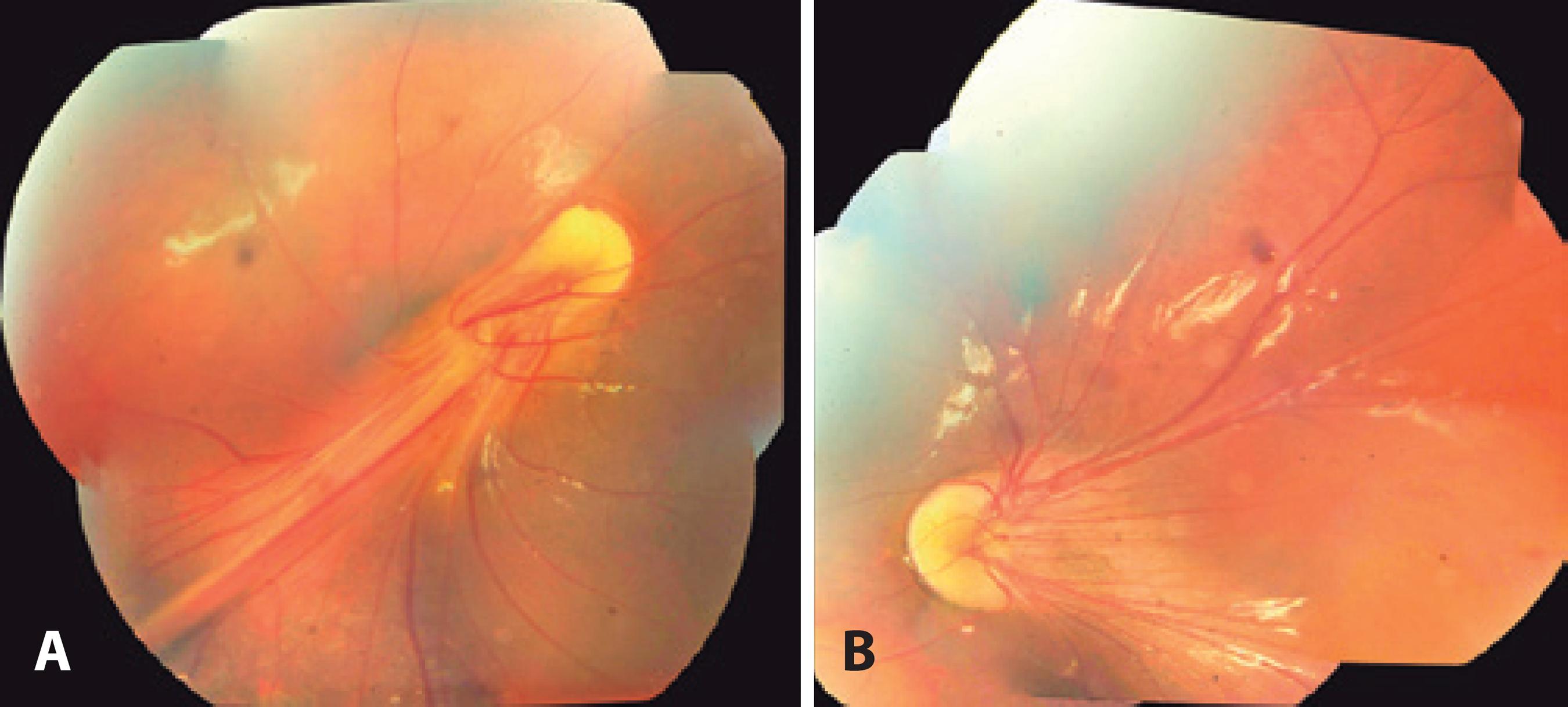
Figure 2 Retinography of both eyes at first visit. A) Dragged optic disc and retrolental membrane in OD, which are characteristic of persistent fetal vasculature; B) Dragged optic disc in OS.
Oral acetazolamide 50 mg t.i.d. and pilocarpine ophthalmic solution 1% OD were prescribed at the same time, and IOP after 24 h was 25 mmHg in OD. At this point, the cornea was clearer, the lens was still anteriorly located close to the cornea, and the anterior chamber was still shallow, with Van Herick Grade I in OD. Carbonic anhydrase inhibitor drug reduced the IOP by decreasing aqueous humor formation3, and topical cholinergic agonist drug induced an anterior movement of the iris lens diaphragm, persisting the angle closure4. Gonioscopy (Zeiss four-mirror lens) showed a closed angle, and although it was difficult to perform dynamic gonioscopy (indentation) because of poor cooperation, some portions of the anterior trabecular meshwork could be seen in OD.
At this point, ocular ultrasonography (B-mode 10-MHz ultrasound, contact technique; Aviso; Quantel Medical, Cournon-d'Auvergne, France) showed peripheral choroidal detachment (choroidal effusion) and a thin membrane adhered to the optic disc with anterior extension, which is compatible with PFV (Figure 3 A). Ultrasound biomicroscopy (50-MHz immersion technique; VuMax II, Sonomed, New Hyde Park, NY, USA) showed a shallow anterior chamber (anterior chamber depth [ACD] = 0.91 mm), closed angle, and anteriorly rotated ciliary body, confirming the diagnosis of ciliary block. A thick retrolental membrane was also identified, which is related to PFV (Figure 3 B, C, D, and E). Pilocarpine was discontinued, and we prescribed atropine 1% q.d., prednisolone 1% q.i.d., and oral prednisolone. After 3 days, IOP lowered to 8 mmHg, and topical steroids were tapered. One month later, IOP was 22 mmHg, and the anterior chamber remained shallow in OD.
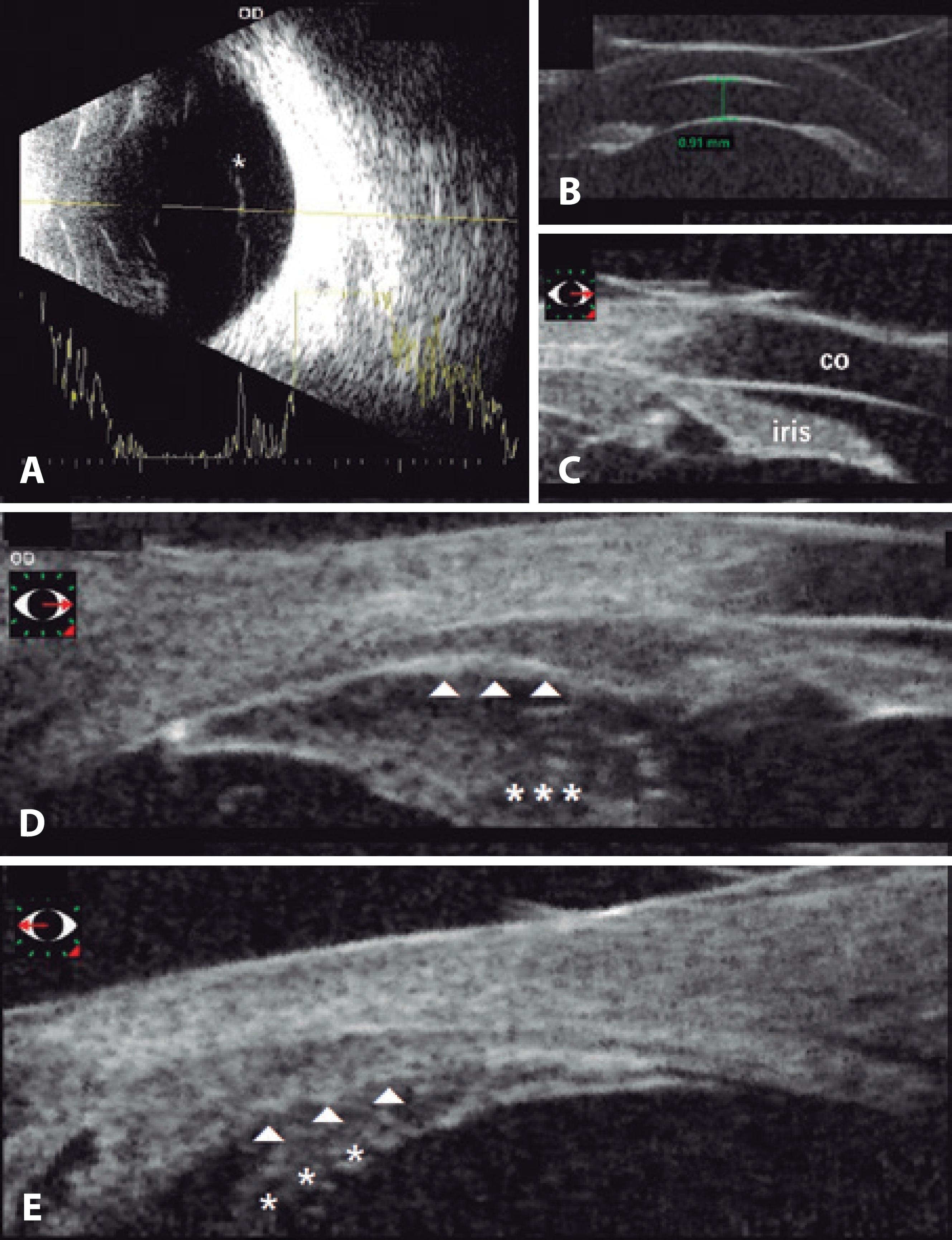
Figure 3 Ultrasound findings. A) 10-MHz B-mode suggested a thin membrane (*) from the optic disc with anterior extension, which is compatible with persistent fetal vasculature. B) 50-MHz ultrasound biomicroscopy demonstrated a shallow anterior chamber (anterior chamber depth = 0.91 mm). C) Angle closure at 3 h (co = cornea). D) Thick retrolental membrane tissue (*) and anterior rotation of the ciliary body (arrows) at 3 h. E) Ciliary body (arrows) and retrolental membrane (*) extension from 3 h to 9 h mid-periphery.
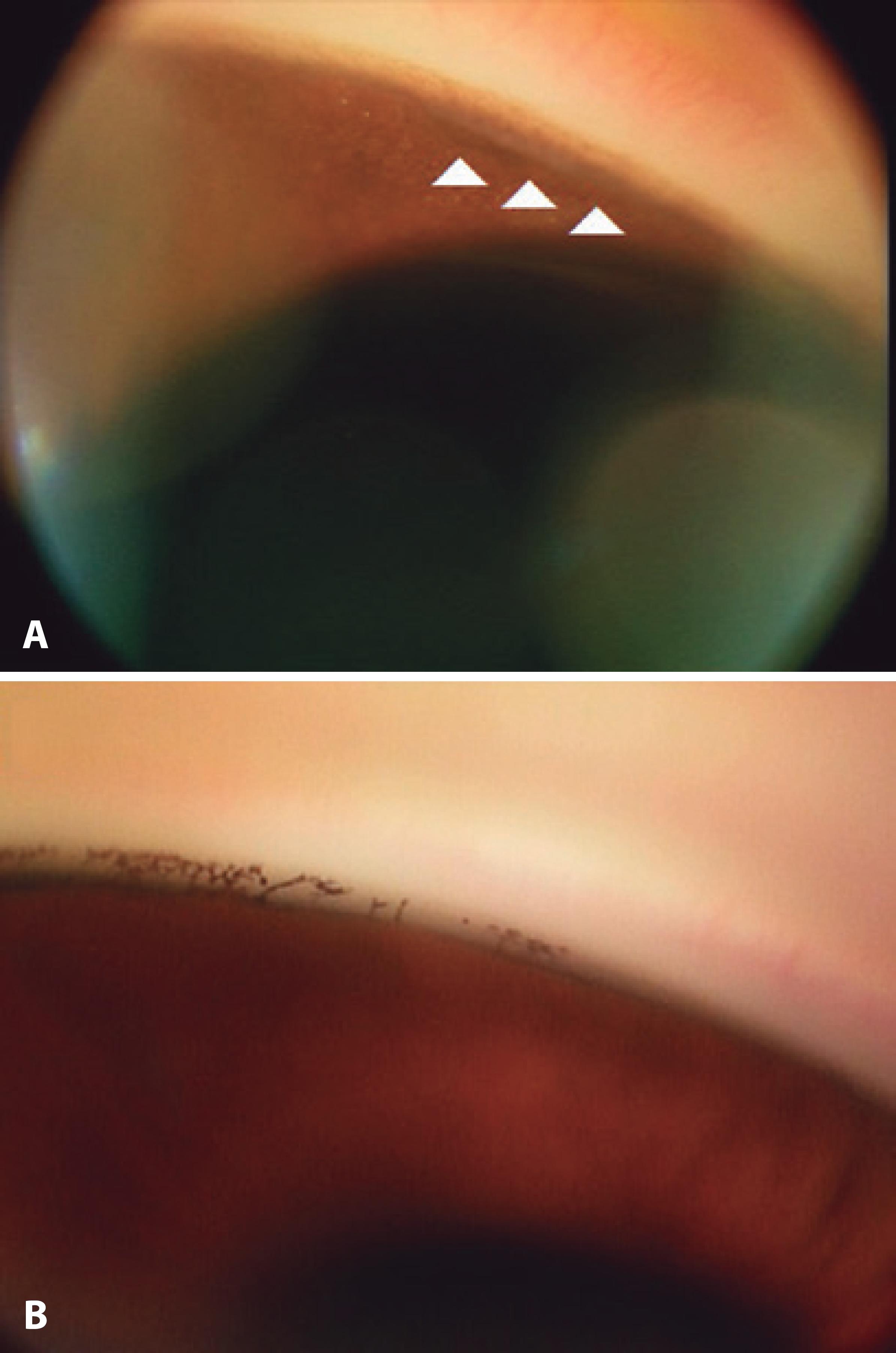
Insufficient control of IOP and persistent ciliary block resulted in surgical intervention, which included lensectomy, iridectomy, and anterior and posterior vitrectomy with no intraocular lens implantation in OD. At the first postoperative visit, IOP control was satisfactory in OD, at 15 mmHg. The best-corrected visual acuity improved to counting fingers at 1 m in OD. At the 6-month postoperative visit, the findings were stable (Figure 1 B), and gonioscopy in OD showed the trabecular meshwork with areas of posterior adhesions, impression of the iris pigments in most of the circumference, and angle recession at 20º in the upper nasal region (Figure 4 A). In OS, gonioscopy showed the trabecular meshwork and the pectinate ligaments of the iris until the camerular sinus (Figure 4 B).
DISCUSSION
Acute angle closure is a rare condition in children. In patients aged 40 years or younger, the incidence of angle closure is 2.34%5. The most common causes for angle closure in young patients are plateau iris syndrome and iridociliary cysts5. There have only been a few cases of angle closure associated with PFV reported in young patients6,7.
The mechanism of acute angle closure has not been fully elucidated in patients with PFV; however, in the present case, the cycloplegic drug might have played a role. The ciliary processes in PFV are usually elongated and pulled into the retrolental membrane8, and type II or "Y-shaped" PFV eyes usually have a shallow anterior chamber and can be accompanied by ciliary detachment and traction or a dense ciliary membrane2. Aqueous misdirection, also known as vitreous block, is a secondary cause of angle closure, and presents with anterior rotation of the ciliary body and positive vitreous pressure9. Cycloplegic drugs tighten the zonule and pull the lens backwards, which opposes aqueous misdirection10. However, after 6 to 24 hours of instillation, the effects of cyclopentolate fade away, which could have induced the blockage of anterior aqueous humor at the level of the retrolental membrane and the ciliary body in the present case. To our knowledge, this is the first case reported in the literature of aqueous misdirection after recovering from cycloplegia in an eye with PFV.
Management of eyes with PFV is still challenging. Early recognition and treatment of the secondary complications are important to minimize the risk of blindness and phthisis bulbi.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

